维持性血液透析患者金黄色葡萄球菌菌血症的临床特征
彭俊琼 周丽芳 储腊萍 周喜连 曹小云

摘要:目的 回顾性分析我院血液透析中心2016年1月至2020年12月维持性血液透析患者发生金黄色葡萄球菌菌血症的临床特征,为临床提供诊断依据。方法 选取我院近五年发生金黄色葡萄球菌菌血症的患者为研究对象,归为感染组,同时未发生感染的维持性血液透析患者为对照组。探讨发生感染患者的易感因素及菌群分布特征,及转归预后分析。结果 血液透析合并金黄色葡萄球菌菌血症患者及对照组各15例,两组基线资料无统计学差异。感染组患者KT/V明显低于对照组(1.63±0.02比2.01±0.23,P<0.01),感染组白蛋白水平(26±3.59比35.64±4.09)、血红蛋白水平明显低于对照组(80.3±13.2比104±5.09)。血透患者金黄色葡萄球菌感染5年发病率为0.18例/血透年,总体治愈率为86.7%,感染死亡率为13.3%。感染组中因长期或临时导管感染比例53.3%(8/15),內瘘及周围皮肤感染比例导致的占13.3%,其他病因导致的占33.4%。结论 营养状况差伴透析不充分、贫血等是金黄色葡萄球菌感染的易感因素。导管感染占金葡菌菌血症感染的重要原因,临床上应加强导管的护理及操作,避免感染的发生。
关键词:血液透析;金黄色葡萄球菌感染;菌血症
【Abstract】Objective To retrospectively analyze the clinical characteristics of the occurrence of Staphylococcus aureus bacteremia in maintenance hemodialysis patients in our hemodialysis center from January 2016 to December 2020 to provide a clinical basis for diagnosis. Methods Patients who developed Staphylococcus aureus bacteremia in the last five years in our hospital were selected as the study subjects and categorized as the infection group, while maintenance hemodialysis patients who did not develop infection were the control group. The susceptibility factors and flora distribution characteristics of the patients who developed infection were investigated, and the prognosis analysis of regression was performed. Results There were 15 patients with hemodialysis combined with Staphylococcus aureus bacteremia and 15 patients in the control group each, and there was no statistical difference between the two groups at baseline. The KT/V of patients in the infected group was significantly lower than that in the control group (1.63±0.02 versus 2.01±0.23, P<0.01), and the albumin level (26±3.59 versus 35.64±4.09) and Hemoglobin level in the infected group was significantly lower than that in the control group (80.3±13.2 versus 104±5.09). The 5-year incidence of Staphylococcus. aureus infection in hemodialysis patients was 0.18 cases/hemodialysis year, with an overall recovery rate of 86.7% and infection mortality rate of 13.3%. The proportion of infections in the group due to long-term or temporary catheter infections was 53.3% (8/15), the proportion of internal fistula and peripheral skin infections resulted in 13.3%, and other etiologies resulted in 33.4%. Conclusion Poor nutritional status with inadequate dialysis and anemia are susceptibility factors for S. aureus infections. Catheter infection accounts for an important cause of Staphylococcus aureus bacteremia infection, and the care and operation of catheters should be strengthened clinically to avoid the occurrence of infection.
【Key words】 Hemodialysis; Staphylococcus aureus infection; bacteraemia
【中图分类号】R457 【文献标识码】A 【文章编号】1673-9026(2022)02-02
感染是终末期透析患者死亡的第二大病因,其中感染导致菌血症占据很大一部分比例【1-3】。与既往的人群相比,透析患者感染导致的死亡率今年较前增加100倍以上【4-5】。金黄色葡萄球菌是维持性透析患者最最常见感染的细菌,占血流感染病原体的>30%以上【6-7】。金黄色葡萄球菌感染可导致各种严重的并发症,包括心内膜炎,骨髓炎,关节炎及肺空洞等表现【8-10】.同时细菌基因类型同样起着更重要的作用,如耐甲氧西林的金黄色葡萄球菌(Methicillin-resistant Staphylococcus. aureus,MRSA)感染导致的死亡率较甲氧西林敏感的金黄色葡萄球菌感染更高【11-12】。MRSA最早于1960s被分离出[13],在近50年间,维持性HD患者的鼻腔内和社区获得性MRSA感染率较前明显增加[14]。2014年报道约40%以上的金黄色葡萄球菌感染样本来源于门诊透析患者[7]。我国流行病学调查报告BSI构成比中,革兰阳性菌占28.5%, 阴性菌占71.5%, 金黄色葡萄球菌中MRSA检出率为34.2%, 但透析患者菌血症的大流行病学数据较少。少数报道提示尿毒症患者导管相关菌血症病原学分布现实格兰阳性菌占64%, 以MRSA及凝固酶阴性的金黄色葡萄球菌耐药菌株(Coagulase-negative staphylococci, CoNS)为主,与国外报道相似[15]。
本研究的主要目的在于分析我院血液透析中心近五年发生金黄色葡萄球菌菌血症患者的临床特征及易感因素及临床转归,为临床诊治提供重要依据。
1 对象和方法
1.1病例選择和来源:选择2016年1月1日至2020年12月30日期间,在我院血液透析中心门诊随访且确诊为金黄色葡萄球菌菌血症感染的患者为感染组,同时以同时期透析年龄及年龄、性别、体重指数为基线指标,选取未发生金葡菌感染的透析患者为对照组。
1.2 纳入与排除标准 纳入标准:(1)年龄大于18岁(2)开始规律血液透析的终末期肾病患者,透析时间大于≥3月。(3)血流感染符合《医院感染诊断标准》中的诊断标准[16]。(4)患者自愿并积极参与完成本项研究。排除标准:(1)血培养病原体除金黄色葡萄球菌外含其他病原体,(2)长期口服激素、免疫抑制剂的患者。(3)合并恶性肿瘤、结核感染患者。(4)近一月有手术或外伤史患者。
1.3 方法
收集整理实验组及对照组各项门诊临床资料,包括性别、年龄及透析参数及透析管路、血红蛋白及白蛋白水平。
1.4 统计分析
采用SPSS17.0软件进行数据分析。两组连续变量间比较采用t检验,计数资料采用率或百分比表示,同时采用卡方检验。易感因素分析采用多变量1:1条件的Logistic回归分析。
2.结果
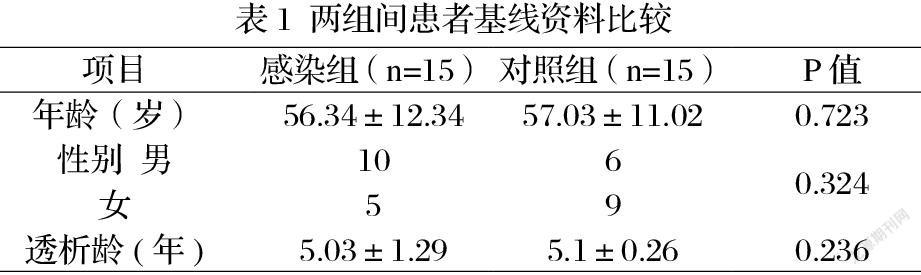
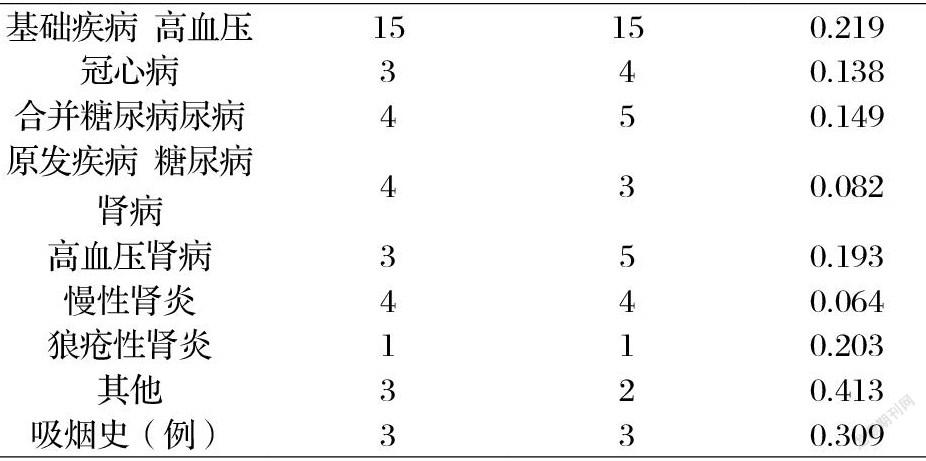
2.1 基线资料:金黄色葡萄球菌菌血症感染组和对照组各纳入15例患者,两组患者在年龄、性别、透析年限、基础疾病、吸烟史等各方面差异均无统计学意义,见表1。
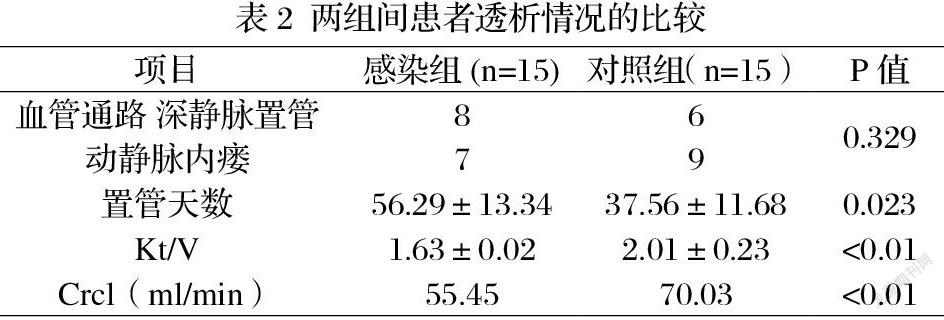
2.2 两组血液透析情况的比较:两组比较在透析通路选择方面无统计学意义。金黄色葡萄球菌感染组尿素清除指数(Kt/V), 肌酐清除指数(CrCL)均明显低于对照组(P<0.01),感染组置管天数较对照组更长(P<0.05),见表2。
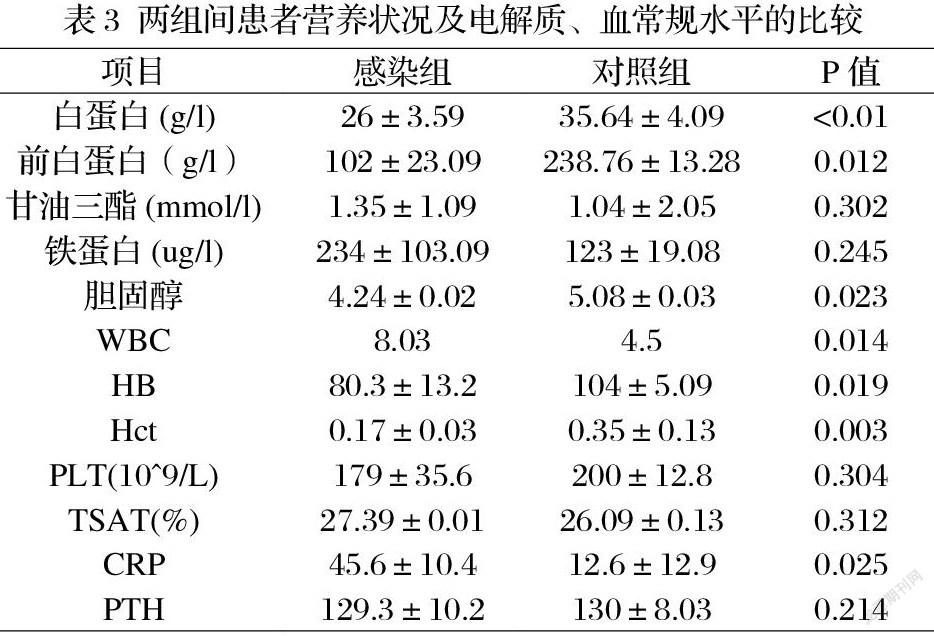
2.3 两组间营养状况及血常规、电解质钙磷代谢水平的比较:感染组患者血清白蛋白及前白蛋白、胆固醇水平均明显低于对照组(P<0.05)。感染组铁蛋白水平、CRP水平均明显高于对照组(P<0.05),感染组血白细胞、中性粒细胞比例水平均明显高于对照组(P<0.05),血红蛋白及HCT水平低于对照组(P<0.01),感染组血清PTH较对照组无差异,见表3。
2.4 综合多因素分析:年龄、性别、透析年、血红蛋白水平、PTH、白蛋白等10个变量进行1:1配对Logistic 多因素分析比较,结果提示各变量均不存在相关关系。
2.5 金黄色葡萄球菌菌血症的临床预后:金黄色葡萄球菌菌血症感染后总体治愈率为86.7%,复发率为13.4%,死亡率为13.3%,见表4。
3.讨论
本研究发现,金黄色葡萄球菌菌血症透析患者白蛋白、血红蛋白水平均低于对照组,提示金葡菌菌血症与患者长期营养不良及贫血相关。营养不良及贫血患者往往免疫力水平较正常患者较差,感染机率明显增加。同时感染反复发作可加重营养不良及贫血水平。发生感染的患者中,长期或临时导管使用患者较内瘘患者发生感染比例更高,达80%。有其他研究发现,置管时间长短与透析患者导管相关血流感染均密切相关【17-18】,故加强导管护理及操作环境的无菌环境对减少医源性感染有重要作用。本研究因样本量较小,未将这些因素纳入进一步分析。
金黄色葡萄球菌是条件致病菌,鼻腔携带是金黄色葡萄球菌菌血症发生的高危因素,S.金黄色葡萄球菌同样能够在宿主组织和异物表面定植,并在各种环境下生存和持续存在。透析患者特别容易受到金黄色葡萄球菌引起的感染,金黄色葡萄球菌感染占透析人群死亡率的8%[19],目前我院单中心的金黄色葡萄球菌菌血症发病率仍较高,这提示需进一步加强导管及内瘘护理等透析患者的卫生宣教及培训制度。现有的治疗指南推荐以青霉素类及万古霉素抗感染治疗为主,对万古霉素耐药的可考虑利奈唑胺或达托霉素治疗[20]。本研究中患者治愈率仍较高,耐万古霉素金黄色葡萄球菌感染目前暂未发生。
目前的抗感染治疗方案明显降低了金黄色葡萄球菌感染的死亡率,但目前仍缺乏预防金黄色葡萄球菌感染的方法,尽管以往有研究认为注射金黄色葡萄球菌疫苗及口服利福平有一定疗效,但目前仍缺乏高质量证据来证实其长期保护作用。这一难题仍待更多更好地研究来指导临床。
參考文献:
[1] Inrig JK, Reed SD, Szczech LA, et al. Relationship between clinical outcomes and vascular access type among hemodialysis patients with Staphylococcus aureus bacteremia. Clin J Am Soc Nephrol. 2006;1(3):518-524.
[2] Jaber BL. Bacterial infections in hemodialysis patients: pathogenesis and prevention. Kidney Int. 2005;67(6):2508- 2519.
[3] Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2018 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019;73(3)(suppl 1):A7-A8.
[4] Sarnak MJ, Jaber BL. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 2000;58(4):1758-1764.
[5] Vogelzang JL, van Stralen KJ, Noordzij M, et al. Mortality from infections and malignancies in patients treated with renal replacement therapy: data from the ERA-EDTA registry. Nephrol Dial Transplant. 2015;30(6):1028-1037.
[6] Tokars JI, Miller ER, Stein G. New national surveillance system for hemodialysis-associated infections: initial results. Am J Infect Control. 2002;30(5):288-295.
[7] Nguyen DB, Shugart A, Lines C, et al. National Healthcare Safety Network (NHSN) dialysis event surveillance report for 2014. Clin J Am Soc Nephrol. 2017;12(7):1139-1146.
[8] Marr KA, Sexton DJ, Conlon PJ, Corey GR, Schwab SJ, Kirkland KB. Catheter-related bacteremia and outcome of attempted catheter salvage in patients undergoing hemodialysis. Ann Intern Med. 1997;127(4):275-280.
[9] Marr KA, Kong L, Fowler VG, et al. Incidence and outcome of Staphylococcus aureus bacteremia in hemodialysis patients. Kidney Int. 1998;54(5):1684-1689.
[10] Kovalik EC, Raymond JR, Albers FJ, et al. A clustering of epidural abscesses in chronic hemodialysis patients: risks of salvaging access catheters in cases of infection. J Am Soc Nephrol. 1996;7(10):2264-2267.
[11] Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003;36(1):53-59.
[12] Del Rio A, Cervera C, Moreno A, Moreillon P, Miro JM. Patients at risk of complications of Staphylococcus aureus bloodstream infection. Clin Infect Dis. 2009;48(suppl 4):S246-S253.
[13] Barber M. Methicillin-resistant staphylococci. J Clin Pathol. 1961;14:385-393.
[14] Carrel M, Perencevich EN, David MZ. USA300 methicillinresistant Staphylococcus aureus, United States, 2000-2013. Emerg Infect Dis. 2015;21(11):1973-1980.
[15] 崔蓉,盧方平,卢照翾,姜磊.替加环素治疗血液透析并发万古霉素不敏感播散性金黄色葡萄球菌败血症一例并文献复习[J].中国研究型医院,2021,8(5):72-76.DOI:10.19450/j.cnki.jcrh.2021.05.019.
[16] 中华人民共和国卫生部. 医院感 染诊断标准(试 行 )[ J] . 中华医学杂志,2 0 0 1 ,81 (5): 314-320.
[17] Saleh H M , T a w f i k M M , Abouellail H . Prospective, r a n d o mized study of l o n g - t e r m h e modialysis catheter r e m o v a l versus guidewire e x c h a n g e to treat catheter-related b l o o d s t r e a m infection[J]. J V a s e S u r g , 2 0 1 7 , 6 6 ( 5 ) 1427-1431.
[18] Chotikanatis K , S u m a n N , B a c k e r M,t»/ al. Pediatric fistula initiative:reducing b l o o d s t r e a m infections in a n outpatient pediatric hemodialysis center [J], J Pediatric Infect Dis Soc,2 0 1 5 , 4 ( 4 ):363-366.
[19] Vandecasteele SJ, Boelaert JR, De Vriese AS. Staphylococcus aureus infections in hemodialysis: what a nephrologist should know. Clin J Am Soc Nephrol. 2009 Aug;4(8):1388-400. doi: 10.2215/CJN.01590309. Epub 2009 Jul 9. PMID: 19590063.
[20] Vandecasteele SJ, Boelaert JR, De Vriese AS. Staphylococcus aureus infections in hemodialysis: what a nephrologist should know. Clin J Am Soc Nephrol. 2009;4(8):1388-1400. doi:10.2215/CJN.01590309