Efficacy and safety of oral Chinese herbal medicine combined with nucleoside antiviral drugs against recurrent genital herpes: a systematic review and meta-analysis
Tian-Li Liu,Tong Liu,Xi-Ming Jin,Qing-Qing Shao,Wen-Jia Wang,Cong Huang,Zhuo Chen*,Ping Yuan
1Institute of Integrated Traditional Chinese and Western Medicine, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology,Wuhan 430030,China.2Department of Biochemistry and Molecular Biology,School of Basic Medicine, Huazhong University of Science and Technology,Wuhan 430030,China.
Abstract Background: To compare the efficacy and safety of Chinese herbal medicine combined with nucleoside antiviral drugs and nucleoside antiviral drugs alone in treating recurrent genital herpes. Methods: PubMed, Embase, Web of Science, Cochrane Library, Chinese Biomedical Literature Database, China National Knowledge Internet, VIP Database, and Wanfang Data were searched from inception to April 2021.Randomized controlled trials on the efficacy and safety of oral Chinese herbal medicine combined with nucleoside antiviral drugs for recurrent genital herpes were collected.All included trials were independently assessed by two reviewers with the Cochrane risk-of-bias tool, and a meta-analysis was conducted using Review Manager 5.4.Results: Compared with the use of nucleoside antiviral drugs alone, combination therapy with oral Chinese herbal medicine plus nucleoside antiviral drugs effectively reduced the herpes recurrence rate after the end of treatment (3 months: P = 0.0002; 6 months: P < 0.00001; 1 year: P < 0.00001) and the number of recurrences each year (P < 0.00001), improved the recurrent Genital Herpes Quality of Life Questionnaire score (P < 0.00001), and regulated the levels of interferon-γ, interleukin-2, tumor necrosis factor-α, and T lymphocyte subsets in the peripheral blood, and the difference was statistically significant.Different subgroups reported mixed results with respect to the efficacy in the short term.The incidence of adverse reactions and the time of symptom disappearance between the two groups were not significantly different.Conclusion: Chinese herbal medicine combined with nucleoside antiviral drugs can effectively reduce the recurrence rate of recurrent genital herpes, improve the patient’s quality of life and enhance the body’s immunity.Considering the possible risk of publication bias, more high-quality randomized controlled trials are still needed to verify the conclusions of this article.
Keywords: recurrent genital herpes; Chinese herbal medicine; nucleoside antiviral drugs;meta-analysis
Background
Genital herpes, caused by herpes simplex virus (HSV) infection, is one of the most common sexually transmitted diseases.HSV-2 and HSV-1 infections account for 80%-90% and 10%-15% of all cases,respectively [1].There are approximately 417 million people living with HSV-2 infection worldwide, and 19.2 million new cases occur each year [2].HSV-1 and HSV-2 establish a latency period in neurons and occasionally reactivate from these cells, thereby causing recurrence in symptomatic and asymptomatic individuals.Therefore,HSV infection often manifests as a chronic and lifelong infection[3-5].Even if the clinical symptoms of herpes are mild in the initial infection,severe or long-term symptoms may appear in the future [6].In addition, HSV-2 reactivates in genital tissues more frequently than HSV-1 [3].Studies have shown that the risk of human immunodeficiency virus infection for HSV-2 carriers in the population is approximately 2 to 3 times that for non-infected people [7, 8],which indicates that infected people face greater health risks.These frequent outbreaks of genital herpes result simultaneously in significant psychological stress on patients and have a tremendous negative impact on the quality of life of patients [9, 10].
Currently, anti-HSV nucleoside drugs, such as acyclovir,valacyclovir, and famciclovir, are still the first-line drugs with which to treat HSV infection [11, 12].Such drugs can inhibit viral DNA replication, thereby achieving antiviral effects, but they cannot eliminate the incubation and recurrence of the herpes virus in the body [13].Thus, it is necessary and urgent to explore new strategies for the treatment of HSV [14].
Genital herpes belongs to the category of “vaginal sores”, “heat sores” and “abnormal vaginal discharge” in traditional Chinese medicine.Thousands of years ago, traditional Chinese doctors started to use herbs to treat genital herpes.The earliest medical book that recorded symptoms related to genital herpes in the Chinese medical literature wasThe Handbook of Prescriptions for Emergencies, written by Hong Ge(283 C.E.-363 C.E.)in the Eastern Jin Dynasty(317 C.E.-420 C.E.) [15].In this book, the author usesPhellodendron,Scutellaria, andCoptisto treat genital herpes.During the Song Dynasty(960 C.E.-1279 C.E.), the Chinese medicine classical book entitledGeneral Medical Collection of Royal Benevolence(1117 C.E.) advocated the use ofAstragalus,Ophiopogon,ScrophulariaandSophora flavescens Aitto treat genital herpes.Last year, the Sexually Transmitted Disease Group of the Chinese Association of Integrative Medicine issued a consensus on the diagnosis and treatment of genital herpes using integrated Chinese and Western medicine [16].Clinicians have a greater authoritative basis when using integrated Chinese herbal medicine and Western medicine to treat genital herpes.
Many clinical trials have evaluated the efficacy of integrated Chinese herbal medicine and nucleoside antiviral drugs (NADs) in treating recurrent genital herpes; however, no relevant systematic analysis or meta-analysis has been published yet.Because of the widespread use of Chinese and Western medicine in the clinical treatment of recurrent genital herpes, we conducted this study to comprehensively evaluate the efficacy and safety of Chinese herbal medicine combined with NADs in the treatment of recurrent genital herpes.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols[17].
Search strategy
To explore the efficacy and safety of oral Chinese herbal medicine combined with NADs in recurrent genital herpes, we searched the following electronic databases: PubMed, Embase, Web of Science,Cochrane Library, Chinese Biomedical Literature Database, China National Knowledge Internet, VIP Database, and Wanfang Data.Additionally, relevant randomized controlled trials (RCTs) were searched through the Chinese Clinical Trial Registry as a supplement.All databases were searched from inception to April 2021.
The keywords included (herpes simplex, genital OR genital herpes simplex OR herpes genitalis OR herpes, genital OR herpes simplex virus genital infection) AND (TCM-WM therapy OR integrated TCM-WM OR traditional Chinese medicine OR herbal medicine OR Chinese drugs, plant OR complementary medicine OR complementary therapy OR alternative medicine) AND (randomized controlled trial OR randomized OR placebo).The region, type and language of publications were not restricted.The search strategy in PubMed, as an example, is shown in Supplementary Table 1.
Inclusion criteria
Type of study.This review only includes clinical RCTs.
Participants.The patient had symptoms of genital herpes more than once.After the first episode of skin lesions subsided, there was a period of asymptomatic disease, followed by reappearance of genital herpes or repeated attacks.
Intervention and control.Patients in the control group used only NADs.Patients in the treatment group were treated with Chinese herbal medicine combined with NADs.
Outcomes.The primary outcomes include changes in clinical symptoms (short-term effective rate; time of symptom disappearance during treatment; recurrence rate after 1, 3, and 6 months or one year after the end of treatment; and frequency of recurrence per year after treatment).The clinical symptoms and signs of the subjects were observed on the seventh day after treatment or after the end of the course of treatment.Treatment of cases in which the area of skin lesions reduced by less than 20% or the symptoms continued to worsen was regarded as ineffective, and that of other cases was considered effective.The efficacy rate in the short term was calculated as the number of effective patients divided by the total number of patients in each treatment group.Starting from the treatment start date, the time when the clinical symptoms (e.g., herpes, skin lesions,scabs) completely disappeared was considered as the time to symptom disappearance.The recurrence rate was calculated as the number of patients with herpes recurrence divided by the total number of patients in each treatment group after a certain period following the end of treatment.The number of relapses per year was the annual average number of relapses of patients in each group after the end of treatment.The secondary outcomes were recurrent Genital Herpes Quality of Life Questionnaire (RGHQOL) score, immune function, and adverse events.The RGHQOL score is a patient-reported outcome measure that determines the impact that recurrent genital herpes has on a patient’s quality of life.The score is used to evaluate recurrent genital herpes patients’ quality of life and ranges from 0 to 20.The higher the score, the better the quality of life [18].Immune function was determined by detecting the contents of interferon-γ (IFN-γ),interleukin-2(IL-2), tumor necrosis factor-α(TNF-α)or T lymphocytes in peripheral blood by biochemical methods.Adverse events include headache, nausea, vomiting, abdominal pain, diarrhoea, and other common drug side effects.
Exclusion criteria
The intervention measures included other treatment methods in addition to traditional Chinese herbal medicine and NADs.The subjects of the study were patients with primary genital herpes.Literature data were incomplete, or the original text could not be obtained.
Data extraction and organization
Two researchers independently screened and extracted the data,evaluated the studies according to the above-mentioned literature inclusion and exclusion criteria, and summarized them in Excel spreadsheets and Word documents.Finally, a third researcher evaluated and screened them.The result was obtained after discussion.The following data were extracted: (a) title of the included study, first author, and year of publication; (b) average age, sex, and sample size of each group; (c) implementation details of intervention measures,such as the type of Chinese herbal medicine and medication plan; and(d) outcome data obtained by the study.
Assessment of methodological quality
The quality of the included RCTs was assessed by 2 evaluators according to the Cochrane Risk of Bias Tool based on the following aspects: (a) random sequence generation (selection bias); (b)allocation concealment (selection bias); (c) blinding of participants and personnel (performance bias); (d) blinding of outcome assessment(detection bias); (e) incomplete outcome data (attrition bias); (f)selective reporting (reporting bias); and (g) other biases.The Grading of Recommendations Assessment Development and Evaluation methodology was used to rate the quality of the evidence.
Statistical analysis
We use Review Manager 5.4 software to perform statistical analysis of all the results.The CochraneQtest was used to analyse heterogeneity(withP< 0.1 indicating significance).Statistical heterogeneity was quantified by theI2statistic.The fixed-effects model was used to analyse the data when the heterogeneity was low (I2< 50%).IfI2>50% in the heterogeneity test, the random-effects model was utilized,and the source of the heterogeneity was analyzed.The continuous data were analyzed by the mean difference (MD) and 95% confidence interval (CI) as the efficacy analysis statistics, and dichotomous data were assessed by the relative risk (RR) and its 95% CI.The meta-analysis results were represented by forest plots.P< 0.05 indicated that the combined effect size of the two interventions was significantly different; otherwise, it indicated that the combined effect size of the two interventions was not significantly different.Publication bias was detected using funnel plots.
Results
Study selection
After a preliminary search, a total of 393 studies were found, 221 duplicates were removed, and 172 studies remained.After further screening by the inclusion and exclusion criteria, 18 RCTs were finally included, with a total of 1,399 patients(Figure 1).
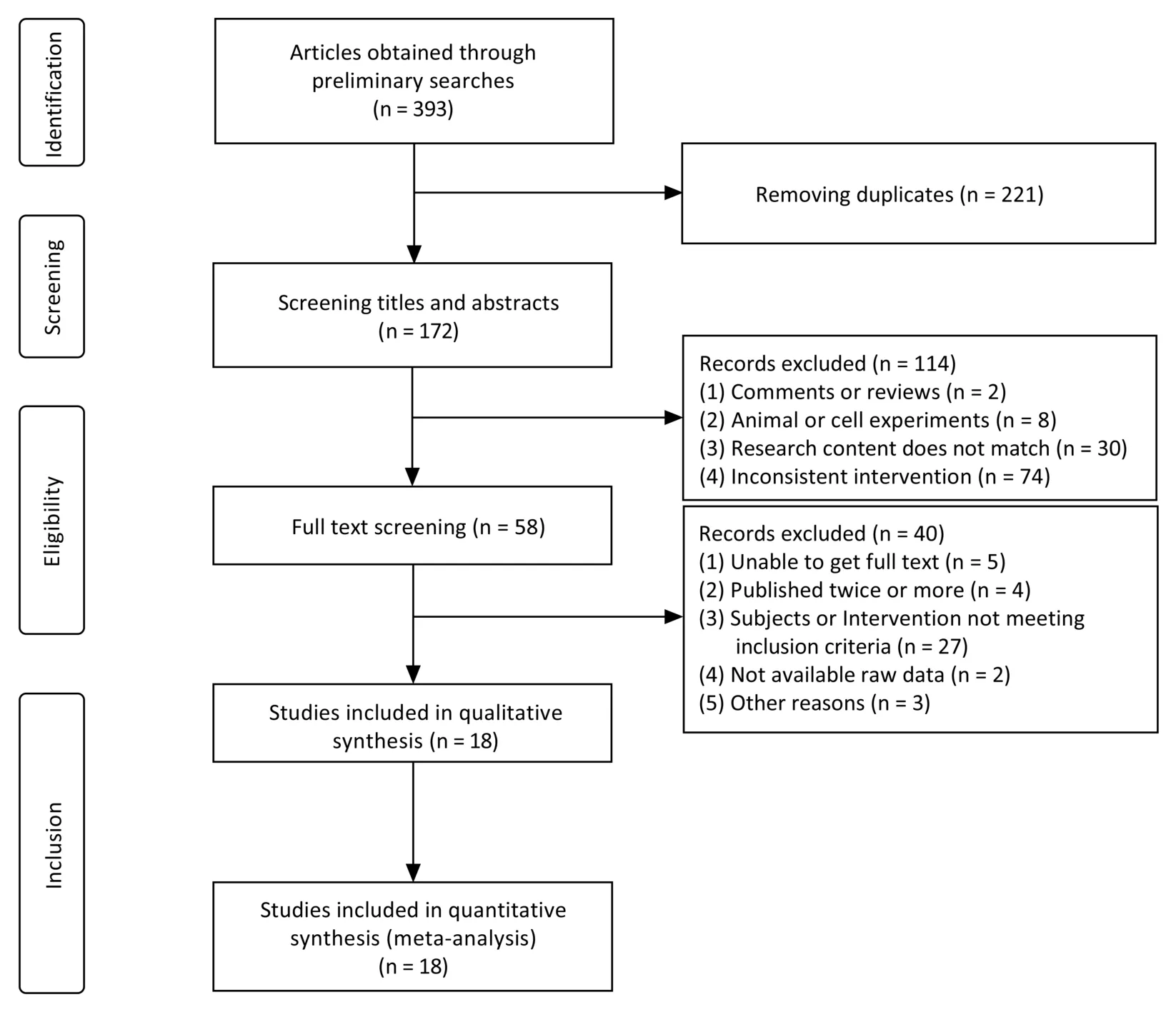
Figure 1 Flow chart of literature screening
Study characteristics
The 18 RCTs included a total of 1,399 patients with recurrent genital herpes.All the studies were published in Chinese.The basic characteristics of the included studies are shown in Table 1 and the ingredients of each prescription are shown in Supplementary Table 2.These studies evaluated the efficacy and safety of oral Chinese herbal medicine plus NADs and NADs alone.Two studies [19, 20] were three-arm trials, including comparisons with oral Chinese herbal medicine alone (not analyzed in this study).Among all the intervention measures included in the study, 10 studies [20-29] used Chinese herbal medicines for oral decoction, and 8 studies[19,30-36]used Chinese patent medicines.Among them, 4 studies used Chinese patent medicines as granular preparations [19, 30, 34, 35], and the remaining 4 used tablets[31, 32]and pills[33, 36].The control group used NADs, including acyclovir [21, 26, 27, 29-31, 35], valacyclovir[24, 25, 28, 32, 34, 36] and famciclovir [19, 20, 22, 23, 33].The intervention time of these studies ranged from 10 days to half a year,and the follow-up time was mostly 6 months (N=7)and 1 year (N=11).
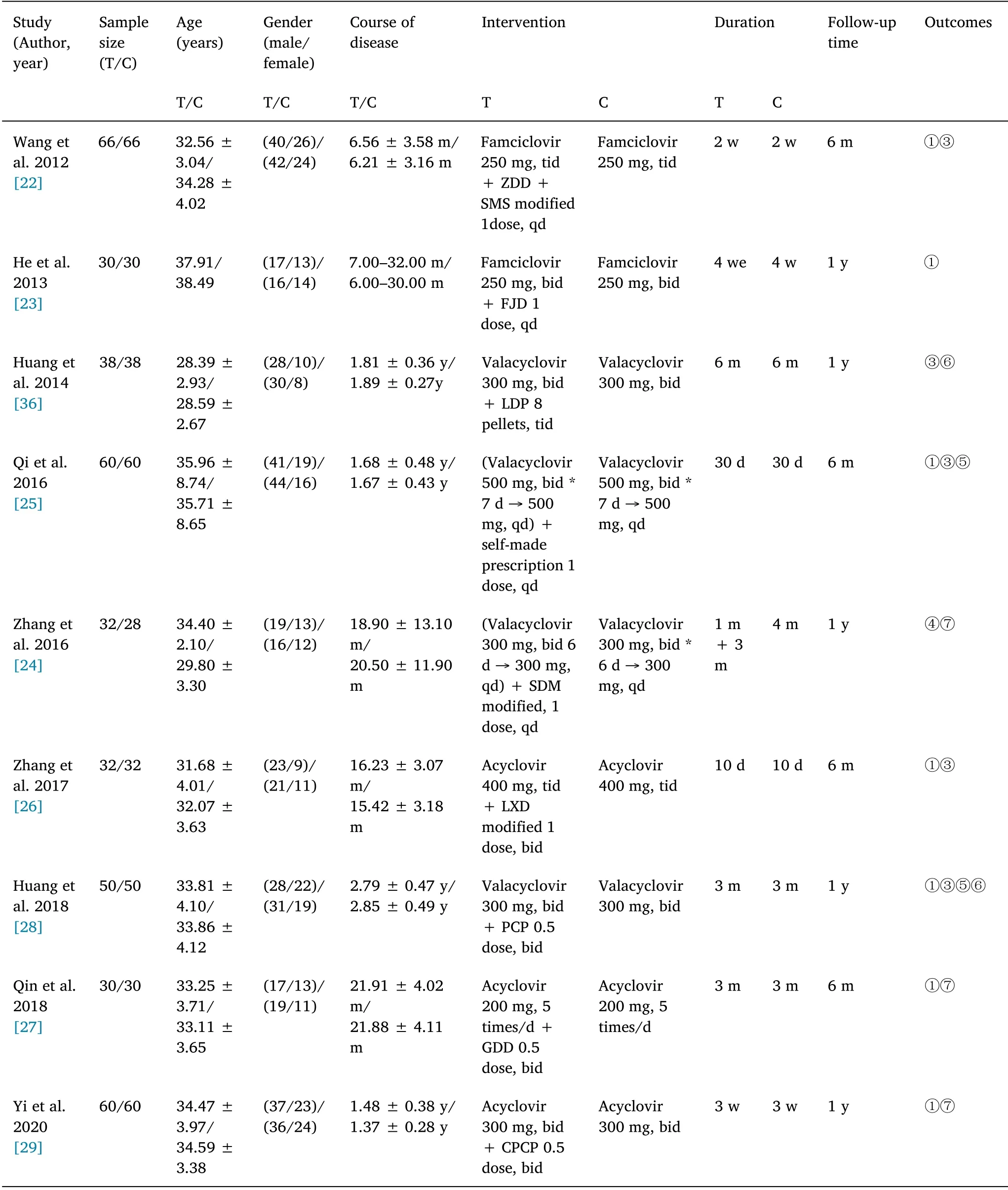
Table 1 The information about all included studies(Continued)
Risk of bias
The Cochrane Risk of Bi as Tool was used to evaluate the quality of the 18 included RCTs.The results of the risk of bias assessment are shown in Figure 2.All the included studies claimed to use the principle of randomization to assign subjects to the experimental or control group,but only 8 studies [19, 20, 24, 26, 29, 30, 32, 36] described the specific principles of randomization.One[36] of the studies randomly assigned patients odd or even numbers based on the order of their visit,which had a higher risk of bias.Seven studies [19, 20, 24, 26, 29, 30,32] were assessed as having a low risk of random sequence bias, one[32] of which used the completely randomized design method of the PEMS software to divide the patients into two groups, and the remaining 6 studies [19, 20, 24, 26, 29, 30] used the random number table method for randomized allocation.Another 10 studies [21-23,25, 27, 28, 31, 33-35] did not describe the principle of randomization allocation, and the risk of bias was unclear.Only one study [20]reported using a blind design (blind of participants) and was evaluated as having a low risk of bias.Other studies [19, 21-36]lacked descriptions of blinding and had a high risk of bias.When at least 10 trials were identified, a funnel chart was used to assess publication bias.The funnel chart shows unsatisfactory symmetry,suggesting that there may be a risk of publication bias(Supplementary Figure 1).
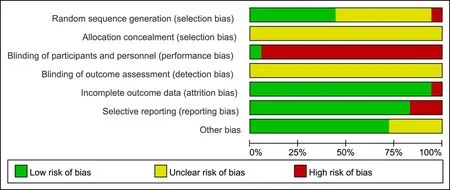
Figure 2 Risk of bias graph
Short-term efficacy rate
Ten [19, 20, 22, 23, 25-30] of the 18 studies used the number of effective cases and the number of ineffective cases as indicators to evaluate the short-term efficacy of the two groups of drugs and included 865 subjects, including 440 in the experimental group and 425 in the control group.The heterogeneity test (I2= 92%,P<0.00001) showed that the difference was statistically significant.We further explored the reasons for the heterogeneity through subgroup analysis.According to the different types of NADs used in the 10 studies, they were divided into three subgroups: the acyclovir,famciclovir and valacyclovir groups.The heterogeneity within the group was not statistically significant (I2= 6%,P= 0.36;I2= 9%,P= 0.30;I2= 47%,P= 0.13), so the fixed-effects model was used for merging.The meta-analysis results show that when the control measure was oral famciclovir, the difference between the two groups was not statistically significant (RR = 1.03, 95% CI = [0.98, 1.07],P= 0.24), indicating that there was no difference in the short-term effectiveness of the two treatment methods(Supplementary Figure 2a).When the antiviral drug used was acyclovir or famciclovir, the meta-analysis results showed that the difference between the two treatments was statistically significant, and the experimental group had a higher efficacy rate than the control group (acyclovir group: RR= 1.24, 95% CI = [1.12, 1.38],P< 0.0001; valacyclovir group: RR= 1.17, 95% CI = [1.06, 1.29],P= 0.002).The reason for the difference between the famciclovir group and the other two groups may be that the effective rate of famciclovir treatment alone is close to 100%.At this time, the combination of treatment with Chinese herbal medicine has little effect on the outcome indicators.
Time to symptom disappearance
A total of four studies [19, 20, 31, 32] used the time of symptom disappearance as an index to evaluate the short-term efficacy of the two groups of drugs.A total of 251 subjects were included, including 126 cases in the experimental group and 125 cases in the control group.Based on the heterogeneity test (I2= 0%,P= 0.77), the difference was not statistically significant, so the fixed-effects model was used to merge.The results of the meta-analysis showed that there was no significant difference in the disappearance time of herpes when Chinese herbal medicine was combined with NADs and when NADs were used alone (MD = 0.14, 95% CI = [−0.38, 0.10],P=0.25), indicating that there was no significant difference in the treatment methods between the two groups with respect to the time to disappearance of symptoms (Supplementary Figure 2b).
Recurrence rate
Seven studies [19, 20, 22, 25, 26, 28, 36] used the recurrence rate after the end of treatment as an index to evaluate the long-term efficacy of the two groups of drugs.The recurrence rates of herpes one month[25], three months[19, 20,25, 36],half a year [19,20, 22, 25,26, 28, 36], and one year [20, 28, 36] after the end of treatment were calculated.
Recurrence rate one month after the end of treatment.Only one study [25] reported the recurrence rate of herpes one month after the end of treatment with a sample size of 60.The herpes recurrence rate in the combined Chinese herbal medicine and NADs group and the NADs only group was not significantly different after one month of treatment (χ2= 0.259,P=0.611).
Recurrence rate three months after the end of treatment.Four studies [19, 20, 25, 36] listed the herpes recurrence rate three months after the end of treatment.One study [36] was eliminated through sensitivity analysis.A total of 260 subjects were included, including 130 in the experimental group and 130 in the control group.Moderate-quality evidence showed (Figure 3a) that the herpes recurrence rate of the combined Chinese herbal medicine and NADs group was significantly lower than that of the NADs group(RR=0.26,95% CI= [0.13, 0.53],P= 0.0002).
Recurrence rate six months after the end of treatment.Seven studies [19, 20, 22, 25, 26, 28, 36] listed data on herpes recurrence rates 6 months after the end of treatment.The heterogeneity test indicated that the difference was statistically significant (I2= 86%,P< 0.00001).A sensitivity analysis of 7 documents was carried out,and it was found that one of the studies [26] had a greater impact on the heterogeneity.If the study was removed, the heterogeneity test was performed again (I2= 0%,P= 0.98), and the difference was found to not be statistically significant; therefore, the fixed effects model was used to merge the remaining 6 studies.A total of 552 subjects were included, including 281 in the experimental group and 271 in the control group.The meta-analysis results in Figure 3b show that the difference between the two groups was statistically significant(RR=0.42,95% CI=[0.32,0.57],P<0.00001), indicating that the recurrence rate in the experimental group was lower than that in the control group half a year after the treatment.The quality of the evidence was high.
Recurrence rate one year after the end of treatment.Three studies[20, 28, 36] assessed the recurrence rate of herpes one year after the end of treatment.Moderate-quality evidence indicates that the recurrence rate of the Chinese herbal medicine combined with NADs group was significantly lower than that of the nucleoside antiviral drug group alone (RR = 0.52, 95% CI = [0.40, 0.67],P< 0.00001)(Figure 3c).
Number of relapses per year
Seven studies [21, 24, 31-35] used the number of recurrences each year after treatment as an indicator to evaluate the long-term efficacy of the two groups of drugs.A total of 457 subjects were included,including 232 in the experimental group and 225 in the control group.From the heterogeneity test (I2= 85%,P< 0.00001), it can be seen that the difference is statistically significant.Considering that the source of the heterogeneity may be due to the large differences in the research objects between the studies, the random-effects model was used for merging.The results of the meta-analysis showed that the number of relapses of subjects in the Chinese herbal medicine combined with NADs treatment group and the NADs group before treatment was basically the same (MD = 0.00, 95% CI = [−0.24,0.25],P= 0.97), and they were comparable (Figure 4a).The difference in the number of recurrences between the two groups after treatment was statistically significant (MD = −2.11, 95% CI =[−2.73, −1.49],P< 0.00001), which means that the number of recurrences per year in the experimental group after treatment was lower than that in the control group, and the quality of the evidence was moderate (Figure 4b).
RGHQOL score
Two studies [25, 28] assessed the RGHQOL scores after treatment.A meta-analysis with a fixed-effects model showed that the quality of life of patients in the treatment group was significantly higher than that in the control group alone after treatment (MD = 3.35, 95% CI = [2.80,3.90],P< 0.00001).No significant heterogeneity was detected in the RGHQOL score after treatment (I2= 0%) (Supplementary Figure 3a).
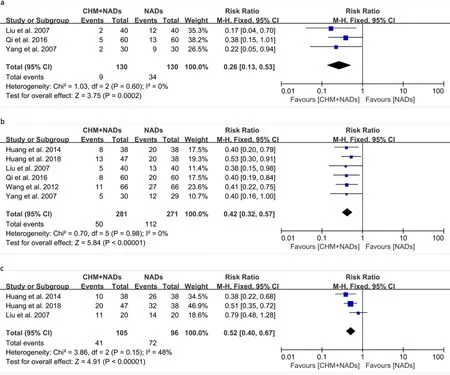
Figure 3 Forest plot of recurrence rate.(a) Recurrence rate three months after the end of treatment.(b) Recurrence rate six months after the end of treatment.(c) Recurrence rate one year after the end of treatment.CHM, Chinese herbal medicine; NADs, nucleoside antiviral drugs; CI,confidence interval.
Serum cytokine content
IFN-γ.Two studies [28, 31] considered the serum IFN-γ levels as an effective index for evaluating the immune function of the two groups of drugs.A total of 164 subjects were included, 82 in both the experimental and control groups.After treatment, the serum IFN-γ level in patients in the oral Chinese herbal medicine combined with antiviral drug treatment group was significantly higher than that in the patients in the NADs treatment group (MD = 121.18, 95% CI =[107.85, 134.51],P< 0.00001) (Supplementary Figure 3b).
IL-2.Two studies [27, 28] assessed the levels of IL-2 in patients to reflect the ability of different treatments to regulate immune function.Two studies have shown that after treatment, the serum IL-2 level of patients in the oral Chinese herbal medicine combined with NADs treatment group was higher than that in the NADs treatment group,and the differences were statistically significant.However, when all the studies were combined in a meta-analysis, the heterogeneity between the studies was relatively large (I2= 99%), which was not suitable for quantitative analysis.
TNF-α.Two studies [29, 35] assessed the serum TNF-α levels of patients,and the results showed that the serum TNF-α level of patients in the oral Chinese herbal medicine combined with antiviral drug treatment group was significantly lower than that in the NADs group.The heterogeneity between the two studies was too large to conduct a quantitative analysis(I2= 100%).
T lymphocyte subsets in peripheral blood
The T lymphocyte subsets in the peripheral blood of the subjects were tested before and after the treatment.It was found that the levels of T lymphocyte subsets in the two groups of subjects before the start of treatment were similar; after the treatment ended, in the Chinese herbal medicine combined with NADs treatment group, patients had higher levels of CD4+T cells in the peripheral blood, while the level of CD8+T cells was lower, and the ratio of CD4+/CD8+T cells was significantly greater than that in the group that received NADs alone.
CD4+T lymphocytes.Three studies [28, 29, 36] reported the changes in the level of CD4+T lymphocytes in peripheral blood as an indicator of the effect of two treatments on the regulation of immune function.One study [28] was removed by sensitivity analysis, and meta-analysis was performed on the remaining two studies [29, 36](Supplementary Figure 3c).A total of 196 subjects were included,including 98 in the experimental group and 98 in the control group.From the heterogeneity test (I2= 0%), the homogeneity was good, so the fixed-effects model was used to combine the effect size.The results showed that there was no statistically significant difference in the levels of CD4+T lymphocytes in the peripheral blood of the two groups of subjects before treatment (MD = 0.94, 95% CI = [−0.12,2.00],P= 0.08).After treatment, the level of CD4+T lymphocytes in the peripheral blood of patients in the integrated Chinese herbal medicine and NADs group was significantly higher than that in the NADs group (MD = 6.63, 95% CI= [5.36, 7.90],P< 0.00001).
CD8+ T lymphocytes.Three studies [28, 29, 36] reported changes in the level of CD8+T lymphocytes in peripheral blood.A total of 296 subjects were included, including 148 in the experimental group and 148 in the control group.After treatment, the level of CD8+T lymphocytes in the peripheral blood of patients in the combined oral Chinese herbal medicine and NADs group was significantly lower than that in the NADs alone group (MD = −5.67, 95% CI = [−8.51,−2.82],P< 0.0001) (Supplementary Figure 3d).
CD4+ T lymphocytes/CD8+ T lymphocytes.Two studies [28, 36]calculated the ratio of CD4+T lymphocytes to CD8+T lymphocytes in peripheral blood to reflect the ability of the two medication regimens to regulate immune function.A total of 176 subjects were included,including 88 in the experimental group and 88 in the control group.A meta-analysis showed that the ratio of CD4+/CD8+T lymphocytes in the peripheral blood of the Chinese herbal medicine and NADs groups was significantly higher than that of the NADs group (MD = 0.52,95% CI = [0.08, 0.96],P< 0.00001) after the treatment(Supplementary Figure 3e).
Adverse events
Eight studies [19, 20, 24, 27, 29, 32-34] mentioned that subjects had adverse reactions, 3 of which [19, 33, 34] could not be meta-analyzed because they did not specify the group in which the adverse reactions occurred.The remaining five studies were included in the meta-analysis.A total of 377 subjects were included, including 186 in the experimental group and 181 in the control group.From the heterogeneity test (I2= 0%), the difference was not statistically significant, so the fixed-effects model was used for merging.The results of the meta-analysis shown in Supplementary Figure 4 demonstrate that the difference between the two groups was not statistically significant(RR=1.01,95%CI=[0.51,2.00],P=0.98),indicating that the incidence of adverse reactions in the experimental and control groups is equivalent and that the combination of Chinese and Western treatment does not increase the incidence of adverse reactions.The adverse reactions in these studies were transient dizziness, headache, or mild gastrointestinal reactions, which did not affect the follow-up treatment, and no serious adverse consequences occurred.
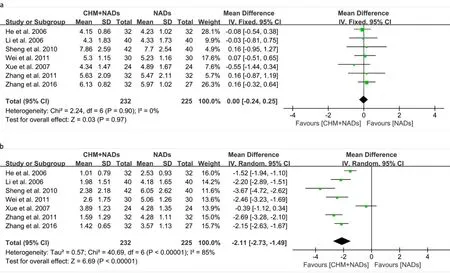
Figure 4 Forest plot of number of relapses per year.(a) Number of relapses per year before treatment.(b) Number of relapses per year after treatment.CHM, Chinese herbal medicine; NADs,nucleoside antiviral drugs; CI, confidence interval.
Sensitivity analysis
After the sensitivity analysis test, three studies [26, 28, 36] were not merged because they had a greater impact on homogeneity after merging the effect size.After removing these studies, the overall effect direction of the meta-analysis was unchanged.
The quality of the evidence
Based on Grading of Recommendations Assessment Development and Evaluation criteria, the quality of evidence was assessed as high or moderate(Supplementary Table 3).
Discussion
Herpes simplex virus can hide in the ganglia after entering the body,and it is difficult to completely eliminate [37].There are clinical data showing that after two years of infection with HSV-2, the virus shedding rate is still high [38].Herpes simplex virus has a long-term recurring feature that has a significant impact on the quality of life of patients.This feature also renders the prevention and treatment of the virus difficult.NADs recommended by the current World Health Organization guidelines, such as acyclovir, valacyclovir, and famciclovir, have limited the control of genital herpes recurrence.Studies have explored complementary or alternative drugs to NADs,but the effectiveness of such drugs in preventing and treating herpes recurrence needs to be verified [39, 40].
Traditional Chinese medicine posits that recurrent genital herpes is caused by exogenous toxins, the accumulation of toxic heat, the accumulation of heat for a long time, and to damp heat down.According to the theory of “differentiation and treatment”, in the treatment of recurrent genital herpes,the main purpose is to clear heat and dampness, cool blood and detoxification, and benefit Qi to strengthen the body’s immunity and avoid herpes recurrence.The selected Chinese herbal medicines in the included trials all strengthened the body and exorcised evil.Additionally, different Chinese herbal medicine components are selected according to the patient’s physique to achieve the purpose of clearing the liver and dampness, strengthening the spleen and relieving depression, or nourishing Yin and clearing heat.
A pooled analysis of 18 RCTs containing 1,399 subjects showed that in addition to the standard treatment recommended by the guidelines,the combined use of oral Chinese herbal medicine can help enhance the body’s immune capacity, effectively reduce the long-term recurrence rate, and improve the quality of life of patients.It can also improve the near-term efficiency to a certain extent, but no improvement with respect to the time to symptom disappearance has been found.The safety analysis of the included studies showed that patients tolerated oral Chinese herbal medicine combined with NADs well, and the incidence of adverse reactions was not significantly different from that of NADs alone.None of the studies reported serious adverse events.
To ensure the comparability of the experimental and control groups,we strictly controlled the two groups of subjects included in the study to have the same baseline before starting treatment.Meta-analysis of the number of annual recurrences, IFN-γ, IL-2, TNF-α, and CD4+,CD8+and CD4+/CD8+T lymphocyte ratios of the two groups of subjects before the start of treatment showed that there was no significant difference in the value, and its homogeneity was ideal,indicating that the two groups of patients had the same severity of illness and were comparable.
In the subgroup analysis, we found that when Chinese herbal medicine was used in combination with acyclovir or valacyclovir, the short-term efficacy rate was better than that of Western medicine alone; when famciclovir was used alone, the efficacy rate was close to 100%,and there was no statistically significant increase in the efficacy rate in the combined treatment group of Chinese herbal medicine.When assessing other outcome indicators, famciclovir was not eliminated in advance.The meta-analysis results suggest that for the treatment of patients with recurrent genital herpes, when famciclovir is used in combination with Chinese herbal medicine, the short-term efficiency is not significantly greater compared with famciclovir alone;however, it still shows obvious effects in terms of immune system activation and reduction of recurrence rate.
The number of recurrences in the two groups of test populations after the end of treatment was counted for a certain time period, and the recurrence rate of the Chinese herbal medicine combined with NADs treatment group at 3 months, 6 months, and one year after treatment was lower than that resulting from NADs alone.
Recurrent episodes of genital herpes are closely related to a patient’s own immune status.To assess a patient’s immune function at the end of treatment, some of the included RCTs analyzed cytokines and immune cells.The results show that Chinese herbal medicine combined with NADs can significantly increase the serum levels of IFN-γ, IL-2 and other cytokines in patients; at the same time, the level of CD4+T lymphocytes in peripheral blood increased, the level of CD8+T lymphocytes decreased, and the ratio of CD4+/CD8+cells increased.In addition, studies have confirmed that TNF-α can enhance viral replication and promote immune escape [41].Two studies [29,35] included in this article assessed the levels of TNF-α in patients after treatment and found that the TNF-α levels in the test group were lower than those in the control group, and the difference was statistically significant.The lower level of TNF-α may prevent the recurrence of herpes caused by frequent shedding of the virus to a certain extent.The above results indicate that the combination therapy of Chinese herbal medicine and NADs can coordinate the body’s immune function and maintain the continuous activation of the immune system, thereby reducing the recurrence rate of herpes.
It should be noted that since the theory of Chinese medicine emphasizes adapting measures to individual conditions and treating according to syndrome differentiation, clinicians need to add and subtract prescriptions according to the different syndrome differentiation types of each patient when formulating medication plans for patients.It is difficult to unify the types and dosages of Chinese herbal medicine.Therefore, this article does not place too many restrictions on the ingredients, formulations and treatments of Chinese herbal medicine but strives to identify the advantages and disadvantages of the combination of traditional Chinese and Western medicine in the treatment of recurrent genital herpes from the methodological level of intervention methods.In addition, the 18 studies included in this article were all Chinese literature, and the risk of publication bias cannot be ruled out.However, there are fewer RCTs analyzed by immunological methods (only 33.3%), and the detection methods and standards are not uniform.The resulting high heterogeneity indicates that similar clinical studies in my country require a more standardized design, more accurate detection, and more scientific analysis.Therefore, the conclusions of this article are worthy of further discussion to provide a reference for clinical and scientific research.
Conclusions
In conclusion, evidence from this review showed that Chinese herbal medicine combined with NADs is more effective in reducing the recurrence rate of genital herpes than NADs alone, and it is safe and reliable.At the same time, combination therapy can also improve the body’s immunity to a certain extent.Considering the low evidence-based qualities of the included research studies, more high-quality research is needed to render this conclusion of higher reference value.
 Traditional Medicine Research2022年1期
Traditional Medicine Research2022年1期
- Traditional Medicine Research的其它文章
- The artificial intelligence watcher predicts cancer risk by facial features
- Evaluation of bioactive flavonoids in Citri Reticulatae Pericarpium from different regions and its association with antioxidant and α-glucosidase inhibitory activities
- Exploring the anti-diabetic effects and the underlying mechanisms of ethyl acetate extract from Sophora flavescens by integrating network pharmacology and pharmacological evaluation
- Effects of Shenling Baizhu powder on endoplasmic reticulum stress related signaling pathway in liver tissues of nonalcoholic fatty liver disease rats
- Artificial neural network techniques to predict the moisture ratio content during hot air drying and vacuum drying of Radix isatidis extract
- Safety of Lycium barbarum L.:more information needed
