Jiangtangjing ameliorates type 2 diabetes through effects on the gut microbiota and cAMP/PKA pathway
Yu-Meng Sun,Wei Qu,Jia-Bao Liao,Le Chen,Yong-Jun Cao*,Hui-Lin Li
1Department of Diabetes and Endocrinology, Nantong Affiliated Hospital of Nanjing University of Chinese Medicine, Nantong 226000, China.2Department of Diabetes and Endocrinology, Affiliated Traditional Chinese Medicine Hospital of Nantong University, Nantong 226000, China.3Department of Diabetes and Endocrinology,Jiaxing Hospital of Traditional Chinese Medicine,Jiaxing 314000,China.4Department of Diabetes and Endocrinology,Shenzhen Affiliated Hospital of Nanjing University of Chinese Medicine,Shenzhen 518000,China.
Abstract Background: During the clinical use of Jiangtangjing granules, we have found that they improve glucose metabolism and relieve symptoms in patients with type 2 diabetes mellitus.We aimed to further investigate the hypoglycemic effects of Jiangtangjing granules and the mechanisms involved. Methods: Type 2 diabetes mellitus was induced in rats by high-fat diet feeding and streptozotocin injection.The rats were then orally administered Linagliptin (3 mg/kg) or Jiangtangjing granules (13 g crude preparation/kg) for 4 weeks.The therapeutic effects of Jiangtangjing granules on glucose metabolism were then investigated.The serum glucagon-like peptide-1, insulin and glycosylated hemoglobin concentrations were measured using enzyme linked immunosorbent assay.Immunohistochemistry and quantificational real-time polymerase chain reaction were performed to quantify glucagon-like peptide-1 protein expression and cAMP, protein kinase A, and Epac1 mRNA expression, respectively.In addition,amplicon sequencing of bacterial 16s rDNA genes in rat feces was also performed to analyze the richness and diversity of the intestinal microbiota and to determine the relative abundances of the dominant bacterial phyla in the intestinal contents of the rats. Results: Jiangtangjing reduced fasting blood glucose concentration (P < 0.05) and blood glucose concentrations during oral glucose tolerance testing (P < 0.01), increased serum glucagon-like peptide-1 concentration after glucose administration (P < 0.05) and improved glucose tolerance (P <0.05).It also increased glucagon-like peptide-1 protein expression (P < 0.05) and the mRNA expression of cAMP (P < 0.05), PKA (P < 0.05), and Epac1 (P < 0.05) in the jejunum.Jiangtangjing also affected the composition of the intestinal microbiota in rats with type 2 diabetes mellitus.Specifically, it increased the relative abundance of Bacteroides and reduced that of Actinobacteria. Conclusion: Jiangtangjing granules have anti-diabetic effects, increasing circulating insulin concentration and glucose tolerance.These effects may be mediated by increases in glucagon-like peptide-1 secretion via upregulation of the cAMP/PKA signaling pathway in the jejunum and alterations in the composition of the intestinal microbiota.
Keywords:Jiangtangjing granule; blood glucose;glucagon-like peptide-1; intestinal microbiota
Background
Diabetes mellitus (DM), which is characterized by hyperglycemia resulting from defective insulin secretion and/or insulin action, is a complex and serious metabolic disease that has increased in prevalence worldwide in recent years[1].It is estimated that by 2,045,the numbers of patients with DM will reach 693 million worldwide and 147.2 million in China, which represents a major health and economic burden [2, 3].More than 90% of patients with DM have type 2 diabetes mellitus (T2DM), which is characterized by insulin resistance and/or a gradual loss of pancreatic insulin secretion [4].The number of patients diagnosed with T2DM is predicted by the World Health Organization to reach > 300 million by 2030 [5].In addition, diabetic complications that cause the dysfunction and/or failure of various organs, such as chronic kidney failure,cardiovascular disease, non-alcoholic steatohepatitis, and cerebral infarction, are becoming highly prevalent [6-8].Therefore, further research regarding the pathogenesis of DM and the development of reliable and effective therapies are urgently needed.
A number of conventional hypoglycemic drugs, such as insulin,sulfonylureas, biguanides, and thiazolidinediones, are widely used in clinical practice.In addition, new drugs, such as sodium-dependent glucose transporters 2 inhibitors, dipeptidyl-peptidase IV inhibitors,and glucagon-like peptide-1 (GLP-1) analogues, have also been introduced [9, 10].However, because of a single hypoglycemic mechanism and/or the specific target, each of these hypoglycemic drugs may not significantly ameliorate diabetic complications.In particular, in some older adults with impaired renal function, a single treatment may be associated with serious side effects, owing to abnormal renal metabolism [11, 12].However, the use of traditional Chinese medicine (TCM), acupuncture, and/or cupping can reduce the side effects of such medical treatments, in addition to having hypoglycemic and lipid-lowering effects of their own [13, 14].This may be explained by beneficial effects in the spleen, kidney, and circulation [15].Moreover, recent studies have shown that the active ingredients of TCMs increase the activity of sputum glucosidase and improve the function of peripheral blood vessels, which are beneficial for diabetic cardiovascular complications [16].Therefore, the use of novel drugs derived from natural products or TCMs and the use of TCMs as adjuvant therapies are of increasing interest, and their pharmacological mechanisms and molecular targets are being actively studied [17].
In the philosophy of TCM, dysfunction of the spleen and stomach and poor blood flow (blood stasis) are thought to be closely related to the development of diabetes [18, 19].As early as the era of the Warring States, the earliest Chinese medical text,Inner Canon of Huangdi(written in 722 B.C.E.-221 B.C.E.), put forward the view that a high-fat and high-sugar diet causes spleen and stomach damage,leading to “Xiaoke” (a disease documented in TCM as being characterized by dry mouth, frequent urination, and fatigue, which is similar to the typical symptoms of diabetes in Western medicine), and states that blood stasis and the progression of diabetes interact as both cause and effect.Over the next 2,000 years, this view has been reinforced and developed by many scholars,such as Zhong-Jing Zhang(about 150 C.E.-154 C.E.to about 215 C.E.-219 C.E.), Xian-Ke Zhao(1573 C.E.-1664 C.E.), and Rong-Chuan Tang (1846 C.E.-1897 C.E.).Based on this theory, Jiangtangjing granules (product with code number Z04001366, approved by Jiangsu Medical Products Administration in China),have been used for the treatment of diabetes at Nantong Hospital of Traditional Chinese Medicine of Jiangsu Province (Nantong, China).They are prepared in Nantong Hospital of Traditional Chinese Medicine and have been widely used for the treatment of T2DM for more than 20 years.They are composed ofAstragali Radix, Polygonati Rhizoma, Coicis Semen, Puerariae Lobatae Radix, Dioscoreae Rhizoma, Crataegi Fructus, Hirudo, and Semen Brassicae(Figure 1), and represents a TCM for the treatment of diabetes associated with splenic dysfunction and blood stasis.
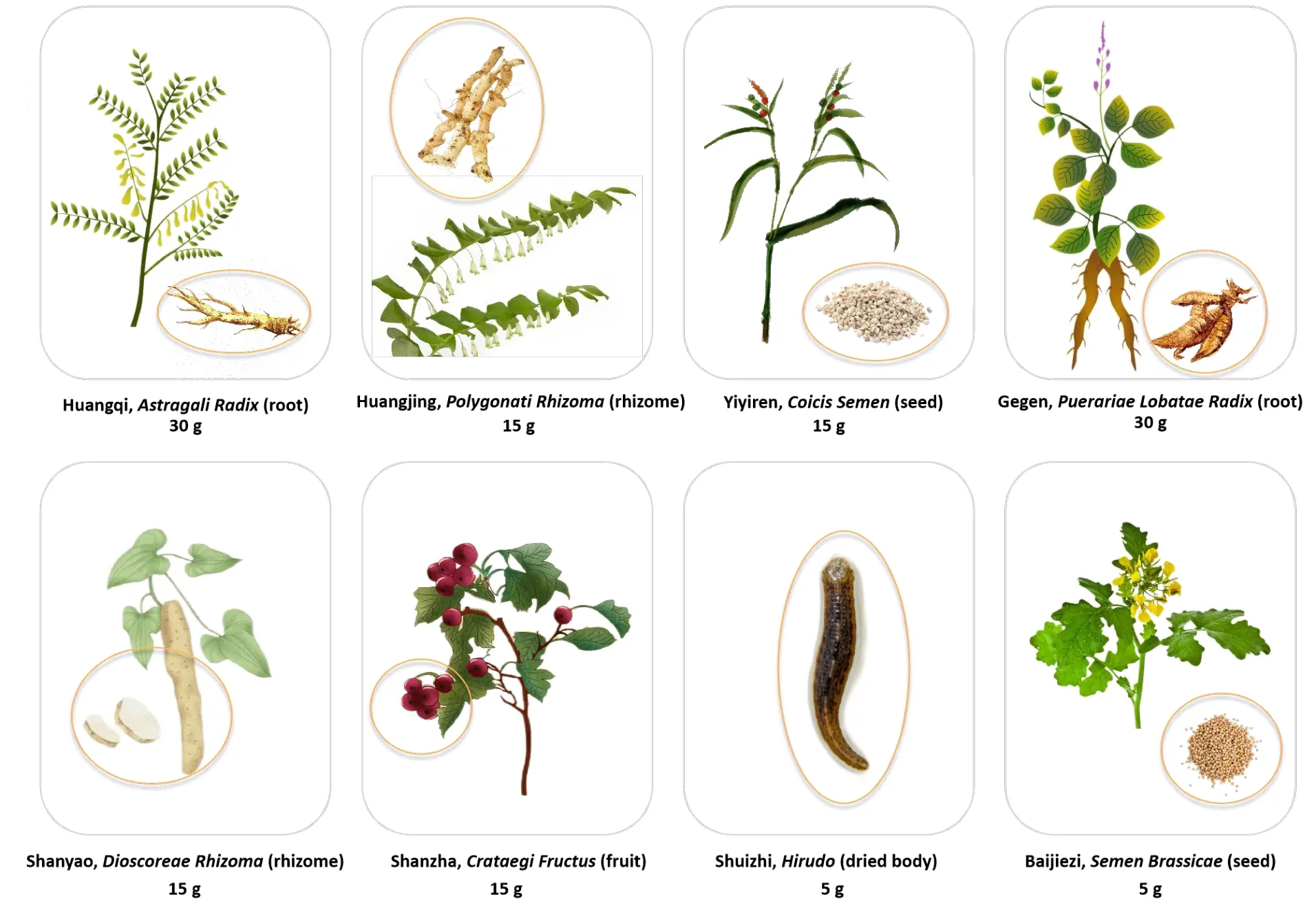
Figure 1 Components of Jiangtangjing granules and their dosage.The parts circled in the figures represent the components with medicinal uses.
Jiangtangjing granules are an adaptation of a classical TCM, Yuye decoction, which is composed ofAstragali Radix, Puerariae Lobatae Radix, Dioscoreae Rhizoma, Anemarrhenae Rhizoma, Galli Gigeriae Endothelium Corneum, Schisandrae Chinensis Fructus, and Trichosanthis Radix.This is recorded in the book of TCM,Records of Traditional Chinese and Western Medicine in Combination, which was written in 1909 C.E.by Xi-Chun Zhang of Qing Dynasty of China (1636 C.E.-1912 C.E.).Yuye decoction was used to treat “Xiaoke” [20].To address the two major causes described above, herbs were added that improve the function of the spleen and stomach and the circulation.Our experience with the use of these granules in clinical treatment suggests that they improve glucose metabolism and relieve symptoms related to TCMs in patients with T2DM.In addition, in older adults with T2DM, Jiangtangjing granules both reduce blood glucose and ameliorate dyslipidemia.Therefore, in the present study, we aimed to further investigate the hypoglycemic effects of Jiangtangjing granules and the mechanisms underlying their beneficial effects in T2DM.The results should provide a theoretical basis for the wider clinical use of Jiangtangjing granules.
Methods
Induction of diabetes in rats
Twenty-six healthy male Sprague-Dawley rats, weighing 220 ± 20 g,were purchased from Qinglongshan Animal Breeding Company(Nanjing, China).The animals were used according to the experimental protocols outlined in theGuide for the Care and Use of Laboratory Animalsand the study was approved by the Research Ethics Committee of Nantong Hospital of Traditional Chinese Medicine of Jiangsu Province (approval No.20200323-176).After 1 week of adaptation, the rats were randomly allocated to two groups: a control(vehicle) group (n = 6) and a T2DM model group (n = 20).T2DM was induced by feeding the rats a high-fat diet (HFD) consisting of 70% rat maintenance feed + 15% lard + 5% sucrose + 10% egg yolk powder (obtained from Qinglongshan Animal Breeding Company,Nanjing, China), for 4 consecutive weeks.Subsequently, after 12 h of fasting, the rats were injected intraperitoneally with 40 mg/kg streptozocin (0.1 mol/L, pH 4.5, Sigma Aldrich, St.Louis, Missouri,America) on 2 consecutive days, as previously described [21].The control group was fed 100% rat maintenance feed and injected with 1 mL/kg 0.01 mol/L sodium citrate buffer (vehicle, pH 4.5).One week later, fasting blood samples were collected by tail incision for the measurement of fasting blood glucose (FBG) using blood glucose test strips (Roche Diagnostics, Munich, Germany).Rats with an FBG concentration > 16.7 mmol/L were considered to be diabetic and were used in the study.
Animal grouping and treatment
Diabetic rats were randomly allocated to three groups: a model group(n = 6), a Jiangtangjing granule group (n = 6), and a Linagliptin group (n = 6).Rats in the model group were intragastrically administered equivalent volumes of normal saline and those in the Jiangtangjing group were intragastrically administered Jiangtangjing granules at a dose of 13 g crude substance/kg body mass once daily.This was based on the dose per unit mass for rats being about 5.98 times that for humans, according to body surface area.The standard dose used in adult humans is 130 g/d, so the daily dose for rats was calculated to be 13 g/kg, according to the following formula:
On the afternoon before Jurgen s departure from home, and beforethe murder, Niels the thief, had met Martin at a beer-house in theneighbourhood of Ringkjobing. A few glasses were drank, not enough to cloud the brain, but enough to loosen Martin s tongue. He began to boast and to say that he had obtained a house and intended to marry, and when Niels asked him where he was going to get the money, he slapped his pocket proudly and said:
Rats in the Linagliptin group (positive control) were intragastrically administered Linagliptin (Boehringer Ingelheim Pharmaceuticals Inc,Frankfurt, Germany) at a dose of 3 mg/kg body mass once daily,which is close to the 5 mg/day dose that human diabetic patients receive.This drug dose was determined according to the drug instructions and previous relevant studies [22].Each substance was administered for 4 weeks.
Preparation of Jiangtangjing granules
Jiangtangjing granules were produced in the preparation room of Nantong Hospital of Traditional Chinese Medicine (Nantong, China).Decoctions ofCoicis Semen,Dioscoreae Rhizoma,Puerariae Lobatae Radix, andCrataegi Fructuswere prepared by boiling in water for 2 h and then for a further 1 h.The filtrates were then mixed and concentrated to a specific gravity of 1.2 at 60 °C.After the filtrates were cooled, ethanol was added and the mixture stirred to an alcohol content of 50%, it was allowed to stand for 24 h, the supernatant was removed, the ethanol was recovered and the liquid medicine was placed separately.Decoctions of the other four herbs were then prepared in water using the same method, the filtrates were mixed,the mixture was allowed to precipitate overnight, and the supernatant was removed.Finally, the two supernatants were mixed, concentrated to a paste with a specific gravity of 1.30-1.35 at 60 °C, dextrin was added to facilitate granulation, and the product was dried.The resulting powder was dissolved in normal saline and stored at 1.3 g/mL.
Oral glucose tolerance testing(OGTT)
At the end of the treatment period, the rats underwent OGTT after fasting for 12 h.Blood samples were collected at baseline and 5, 10,15, 30, 60, and 120 min after the intragastric administration of 40%glucose (2 g/kg).Before glucose administration and 30, 60, and 120 min afterwards, the glucose concentrations of blood obtained from a tail vein of each rat was measured using blood glucose test strips.
Glycated hemoglobin (HbA1c) assay
Two days after OGTT, the rats were fasted for 12 h and then terminally anesthetized by the intraperitoneal injection of pentobarbital sodium to obtain blood samples from the abdominal aorta.The samples were centrifuged at 1358.37 xg for 10 min to collect serum, which was used for the measurement of HbA1c concentration.In addition, the jejunum and pancreas of the rats were also collected.Glucose concentration was determined using blood glucose test strips and a glucometer (Roche Diagnostics, Munich,Germany) and serum HbA1c levels were determined using a rat HbA1c enzyme linked immunosorbent assay (ELISA) kit (Elabscience Biotechnology Co., Ltd, Wuhan, China), according to the manufacturer’s protocol.
Measurement of insulin and GLP-1 concentration
Blood samples collected at 0, 5, 10, 15 min of OGTT were allowed to coagulate in tubes for 2 h at room temperature, then centrifuged at 3,000 rpm/min for 10 min.The supernatants were collected and diluted 10-fold in the provided sample diluent prior to evaluation.The serum insulin and GLP-1 concentrations were measured using a high-sensitivity rat insulin immunoassay kit (EZassay Ltd., Shenzhen,China) and rat glucagon-like peptide-1 ELISA kit (Cusabio, Houston,Texas, America), respectively, according to the manufacturers’protocols.
Briefly, 100 μL of each serum sample was added to the test wells,with phosphate buffer saline (PBS) as the negative control, and they were incubated for 2 h at 37 °C.After washing, 100 μL of biotin-labeled antibody was added to each well and the plate was incubated for 1 h at 37 °C.After washing, 100 μL of horseradish peroxidase-labeled anti-biotin protein was added and the plate was incubated for a further 1 h at 37 °C.Subsequently, 90 μL of tetramethylbenzidine reaction substrate was added and the plate was incubated at 37°C, followed by 90 μL of stop solution.The absorbance of each well was measured using a microplate reader at 450 nm and the serum HbA1c, insulin, and GLP-1 concentrations were calculated using standard curves.
Immunohistochemical analysis of GLP-1 expression in rat jejunum
The rat jejunal samples were fixed in 4% paraformaldehyde for 24 h,embedded in paraffin, and cut into 4-6-μm-thick sections for immunohistochemical analysis.Briefly, to fix the jejunal tissue to the slides, paraffin-embedded sections were baked at 65 °C for 2 h.Then,the tissues were deparaffinized with xylene and an ethanol gradient.The hydrated slides were subjected to microwave antigen retrieval,washed with PBS, blocked with 5% bovine serum albumin, and incubated with anti-GLP-1 antibody (Abcam, No.ab22625, London,Britain) at 4 °C overnight.The slides were subsequently incubated with a secondary horse radish peroxidase-conjugated antibody for 1 h at 37 °C and stained using a diaminobenzidine horseradish peroxidase color development kit(Biotech Well, Changzhou, China).After rinsing with double distilled H2O, the sections were counterstained with hematoxylin, differentiated with 1% HCl-alcohol, and dehydrated using an ethanol gradient.
Measurement of the expression of cAMP, protein kinase A (PKA),and Epac1
Rat jejunal tissue samples (about 30 mg) were powdered in liquid nitrogen, then RNA was extracted using RNAiso Plus (Takara, Kyoto,Japan), according to the manufacturer’s protocol.After the assessment of RNA purity and integrity, reverse transcription was performed using a PrimeScript™RT kit with gDNA eraser (Takara, Kyoto, Japan).Subsequently, the reverse-transcribed cDNA templates were subjected to plymerase chain reaction (PCR) using SYBR® Premix Ex Taq™II(Takara, Kyoto, Japan).Amplification was performed using the following conditions: 95 °C for 10 min, followed by 40 cycles of 95 °C for 5 s and 60 °C for 1 min, and a final annealing and extension at 65 °C for 15 s.The primers used were: cAMP (forward): 5’-ACC AAT CTC TAC CGT CTC CT-3’, cAMP (reverse): 5’-CTT GCT ACA GAC AGT CTC CTT C-3’;PKA(forward):5’-CTA GCC AAA GCC AAG GAA GA-3’,PKA (reverse): 5’-GTG CCA AGG GTC TTG ATT CTA-3’; Epac1(forward): 5’-CTT CGA GGA GCT CGT ACA TAT C-3’, Epac1 (reverse):5’- CCT TGC TGT GTG GTT CAA AG-3’; GAPDH (forward): 5’-GGG AAA CCC ATC ACC ATC TT-3’, and GAPDH (reverse): 5’-CCA GTA GAC TCC ACG ACA TAC T-3’.GAPDH served as the reference gene and was used to normalize the relative expression of the target genes,using the 2-ΔΔCt method.
Collection of feces and DNA extraction
To avoid cross contamination, each rat was kept in a sterilized,bedding-free cage and fecal pellets were collected in sterile tubes.Gut microbial DNA was extracted as described previously [23].Briefly,fresh feces (0.2 g) were dissolved in PBS (0.05 mol/L, pH 7.4),homogenized for 5 min,and centrifuged at 1,000 rpm for 15 min three times.The supernatants were then collected and centrifuged at 12,000 rpm for 10 min.The pellets were each vortexed in 1 mL of PBS and then centrifuged for 5 min at 14,000 rpm, and this was repeated five times.The final pellets were washed with sterile water and the cells were lysed using TritonX-100.Then, 200 μL of each supernatant obtained by the centrifugation of each lysate at 12,000 rpm for 30 s were extracted using phenol/chloroform (1: 1 v/v) for 10 s, then centrifuged for 30 s at 12,000 rpm.The supernatants were collected and mixed with 2.5-fold volumes of cold ethanol for 1 h at −20 °C.After centrifugation at 12,000 rpm for 1 min, the pellets obtained were resuspended in cold ethanol, incubated at −20 °C for 1 h, and centrifuged for 1 min at 12,000 rpm.Finally, the DNA pellets obtained were dried and dissolved in 30 μL of double distilled H2O.
Sequencing
The purity and concentration of the DNA samples obtained were measured using a NanoDrop Spectrophotometer (Thermo Fisher Scientific, Waltham, Massachusetts, America).Then, the relative abundance of each bacterial species was assessed using 16S rDNA PCR.The isolated DNA was amplified in total reaction volumes of 25 μL,which comprised SYBR®Premix Ex Taq™II 12.5 μL, cDNA template 2 μL, forward primer 0.5 μL, reverse primer 0.5 μL, and double distilled H2O 9.5 μL, under the following reaction conditions: 95 °C for 10 min;followed by 40 cycles of 95°C for 15 s and 60 °C for 45 s; 95 °C for 15 s; 60 °C for 1 min; 95 °C for 15 s; and 60 °C for 15 s.The V3-V4 hypervariable regions of the 16S rRNA genes ofActinobacteriaandBacteroidaleswere amplified using the universal primers 5’-GTA CTC CTA CGG GAG GCA GCA-3’and 5’-GTG GAC TAC HVG GGT WTC TAA T-3’, with 8-nt barcodes.The amplified products were purified using a PCR purification kit (Invitrogen, Carlsbad, Southern California,America)and then used as DNA standard samples for amplification, as described above.In addition, diethylpyrocarbonate-treated water was used as a negative control in the PCR reaction.To analyze the diversity and abundance of the intestinal microbiota in diabetic rats administered Jiangtangjing granules, clustering analysis, diversity analysis, and taxonomic analysis of the operational taxonomic units of the sequencing data were performed.
Statistical analysis
Data is presented as mean ± standard deviation.SPSS (version 22)was used for data analysis.One-way analysis of variance was used to analyze the data, after confirmation of the homogeneity of variance using Levene’s test.To identify differences among the treatment groups, Tukey’s test was then used.P< 0.05 was considered to represent statistical significance.
Results
Diabetes is induced in rats by HFD-feeding and streptozotocin injection
The FBG concentrations of the rats did not significantly differ before the induction of diabetes.After HFD-feeding and streptozotocin injection, the FBGs of the model group were significantly higher than those of the control group (22.83 ± 1.82 vs.5.1 ± 0.79 mmol/L,respectively,P< 0.01), confirming the successful induction of diabetes.
Jiangtangjing improves glucose tolerance in diabetic rats
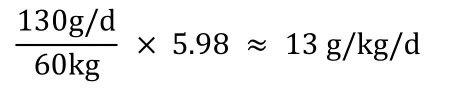
The administration of 40% glucose(2 g/kg) caused a rapid increase in the blood glucose concentrations of diabetic rats to about 30 mM, and this hyperglycemia was maintained until 120 min.However, diabetic rats administered Jiangtangjing granules for 4 weeks had lower blood glucose concentrations.As shown in Figure 2A, the administration of glucose also rapidly increased blood glucose in the Jiangtangjing granule and Linagliptin groups, but at 0.5, 1, and 2 h of OGTT, the concentrations were significantly lower than those in the model group(P< 0.05 orP< 0.01).In particular, at the 2-h time point, the blood glucose concentrations of the Jiangtangjing granule and Linagliptin groups were 20.57 ± 1.17 mM and 16.43 ± 1.46 mM, respectively.Thus, Jiangtangjing granules improved the glucose tolerance of the diabetic rats.The FBG of the model group was much higher than that of the control group after 4 weeks.However, both Jiangtangjing granules and Linagliptin significantly reduced the FBG of the diabetic rats (22.80 ± 1.80 mM vs.16.90 ± 1.70 mM,P< 0.05 and 22.80 ±1.80 mM vs.12.10 ± 1.20 mM,P< 0.01, respectively).
Jiangtangjing affects the long-term glucose status of diabetic rats
Two days later after OGTT, the FBG and HbA1c concentrations of the rats were also determined to further evaluate the effects of Jiangtangjing granules on glucose status.As shown in Figure 2B and Figure 2C, FBGs and HbA1cs in diabetic rats increased significantly compared with the control group (23.07 ± 1.48 vs.4.47 ± 0.65 mM for FBG and 6.67% ± 0.51% vs.3.53% ± 0.25% for HbA1c,P<0.01).FBGs and HbA1cs in diabetic rats decreased significantly after 4 weeks of Jiangtangjing treatment compared with the model group(18.17±1.72 mM vs.23.07±1.48 mM for FBG and 5.23% ±0.40%vs.6.67% ± 0.51% for HbA1c,P< 0.05), and although these effects were slightly weaker than those of Linagliptin, this confirms that Jiangtangjing granules have long-term effects on the glucose status of diabetic rats.
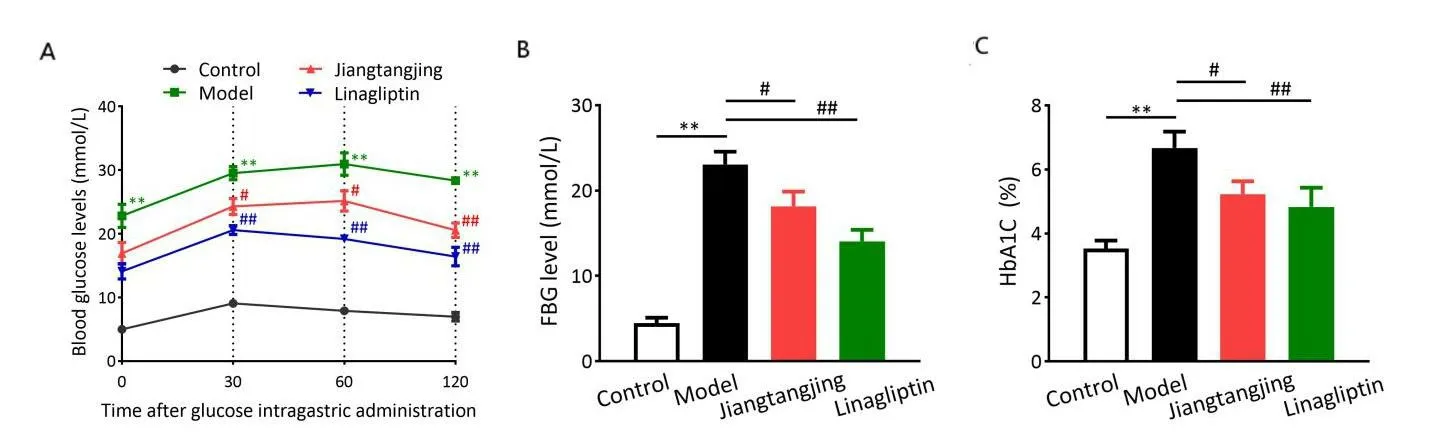
Figure 2 Jiangtangjing improves glucose tolerance in diabetic rats.After 4 weeks of treatment, the blood glucose concentrations of diabetic rats were measured at the indicated time points during OGTT (A).Jiangtangjing granules affect the glucose status of diabetic rats.Two days later after OGTT, the FBG (B) and serum HbA1c (C) concentrations of each group were measured.**P < 0.01 represents comparison with the control group;#P < 0.05 and##P < 0.01 represent comparison with the model group.OGTT, oral glucose tolerance testing; FBG, fasting blood glucose;HbA1c, glycated hemoglobin.
Jiangtangjing increases the serum GLP-1 concentration and improves glucose tolerance
GLP-1 is an incretin hormone that is secreted by intestinal L-cells.It helps maintain glucose homeostasis by stimulating glucose-dependent insulin secretion and inhibiting gastric emptying and glucagon secretion [24].Therefore, we measured the serum GLP-1 and insulin concentrations of the rats during OGTT by ELISA.The serum GLP-1 concentration of the control rats was 24.49 ± 1.84 pg/mL, which was higher than that of the model group (P< 0.05), before glucose administration.The serum fasting GLP-1 concentration was increased by drug administration, and Linagliptin treatment had a more marked effect (P< 0.05 vs.the model group).Glucose administration significantly increased the serum GLP-1 concentrations.In the Linagliptin-treated group, it increased from 21.71 ± 1.59 to 23.22 ±1.38 pg/mL within 5 min and increased to 26.16 ± 1.60 pg/mL at 15 min.In the Jiangtangjing-treated group, the serum GLP-1 concentrations 5, 10, and 15 min after glucose administration were 21.66 ± 1.35, 23.48 ± 1.16, and 24.57 ± 0.90 pg/mL, which were higher than those of the model group (Figure 3A).In addition, the serum insulin concentrations of the rats were determined.Control rats had lower fasting insulin concentrations than the diabetic rats (13.27± 0.73 ng/mL vs.22.55 ± 3.54 ng/mL, respectively,P< 0.01)before OGTT.The serum insulin concentrations of the diabetic rats remained high after fasting and during OGTT.They increased from 22.55 ± 3.54 ng/mL at 0 min to 28.82 ± 2.97 ng/mL after 15 min of OGTT.However, the administration of Jiangtangjing granules and Linagliptin reduced the fasting insulin concentrations of the diabetic rats (P< 0.05).During OGTT, the serum insulin concentrations increased from 18.48 ± 2.27 ng/mL to 28.20 ± 1.34 ng/mL in the Jiangtangjing-treated group.This improvement in glucose tolerance was comparable to that induced by Linagliptin (Figure 3B).These data imply that Jiangtangjing granules may affect insulin secretion in diabetic rats.
Figure 3 Jiangtangjing granules increase the serum GLP-1 and insulin concentrations of diabetic rats.Serum GLP-1 (A) and insulin (B)concentrations of normal and diabetic rats at the indicated time points after glucose administration during an OGTT.*P < 0.05 and**P < 0.01 represent comparison with the control group;#P < 0.05 represents comparison with the model group.GLP-1, glucagon-like peptide-1; OGTT, oral glucose tolerance testing.
Jiangtangjing administration increases GLP-1 expression in rat jejunum
We also identified GLP-1 expression in the jejunum of the rats: GLP-1 immunoreactivity was identified by the presence of brown-yellow granules in the cytoplasm of columnar villous epithelial cells.The expression of GLP-1 in the jejunum of diabetic rats was significantly lower than that in control rats (P< 0.01), and Linagliptin treatment significantly increased the expression of GLP-1 (P<0.01).In addition,the expression of GLP-1 was also slightly higher in the Jiangtangjing-treated group (P< 0.05, Figure 4), suggesting that Jiangtangjing granules may have their anti-diabetic effects at least in part by affecting GLP-1 expression in the jejunum of rats.

Figure 4 Jiangtangjing granules increase the expression of GLP-1 in rat jejunum.(A)Immunohistochemical analysis of GLP-1 expression in rat jejunum.GLP-1 immunoreactivity is indicated by the presence of brown-yellow granules in the intestinal gland columnar villous epithelial cells.Upper panel:magnification ×100; lower panel: magnification ×200.(B)Quantification IOD of GLP-1 protein expression in each group.**P <0.01 represents comparison with the control;#P < 0.05 and##P < 0.01 represent comparison with the model group.GLP-1, glucagon-like peptide-1;IOD, integral optical density.
Jiangtangjing reduces the expression of cAMP, PKA and Epac1
We also measured the expression of cAMP, PKA and Epac1 in rat jejunum by quantificational real-time polymerase chain reaction.As shown in Figure 5, the expression of cAMP, PKA and Epac1 was significantly higher in diabetic than control rats (> 3.5-fold higher for cAMP and PKA and about 2-fold for Epac1,P< 0.01).Jiangtangjing reduced the expression of these three genes, albeit that this effect was weaker than that of Linagliptin (P< 0.05).
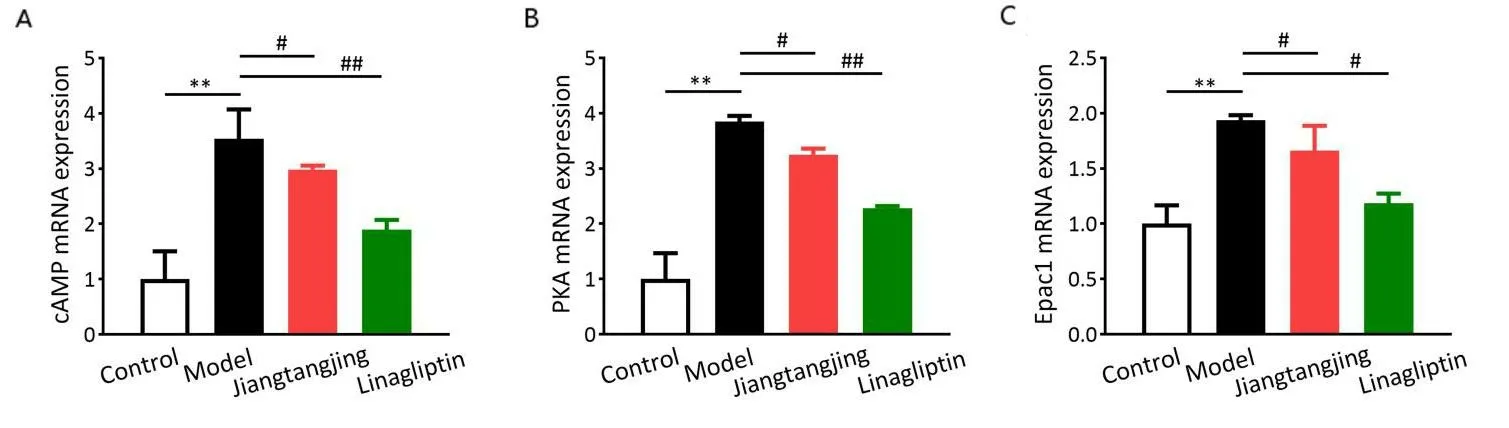
Figure 5 Jiangtangjing granules reduce the expression of cAMP, PKA and Epac1.qRT-PCR assay was used to measure the expression of cAMP,PKA and Epac1 in the jejunum of the rats.The relative expression of the target genes was normalized to that of the control group.**P < 0.01 represents comparison with the control group;#P < 0.05 and##P < 0.01 represents comparison with the model group.PKA, protein kinase A;qRT-PCR, quantificational real-time polymerase chain reaction.
Jiangtangjing increases the richness and diversity of the intestinal microbiota
The relative abundances of target bacterial taxa were assessed using 16S rDNA PCR.Heat maps are used to display the abundance of the selected taxa and show similarities and differences between treatment groups.A heat map for the present analysis is shown in Figure 6, in which the rows represent single taxa, the columns represent the groups (n = 3 samples per group; indicated as #1, 2 and 3), and the color of each square represents the relative abundance of the taxa in each row.High abundance is indicated in blue and low abundance is indicated in white.The diabetic rats had significantly lower intestinal bacterial richness (Figure 6A).Beta diversity analysis was used to compare the similarity of species diversity between the groups,involving principal coordinates analysis, in which the distance between the sample points represents the similarity of the microbial community in the sample, with smaller distances representing greater similarity.The control and diabetic groups were widely separated.The intestinal bacterial diversity of the Jiangtangjing and Linagliptin groups significantly differed from that of the model group(Figure 6B).
Alpha diversity analysis was used to assess the richness and diversity of the microbial communities.The Chao index is often used to describe the richness of a bacterial community, while Shannon’s index is used to characterize species diversity.The Chao1 index and Shannon index of the diabetic rats were significantly lower than those of the control group (P< 0.01, Figure 6C and Figure 6D).However,Jiangtangjing treatment increased both the Chao1 index and Shannon index (P< 0.05).In summary, both the Chao1 index and Shannon index showed the following trend: control group > Linagliptin group > Jiangtangjing group > model group.These data indicate that both the bacterial richness and species diversity of diabetic rats are improved by Jiangtangjing granule treatment.
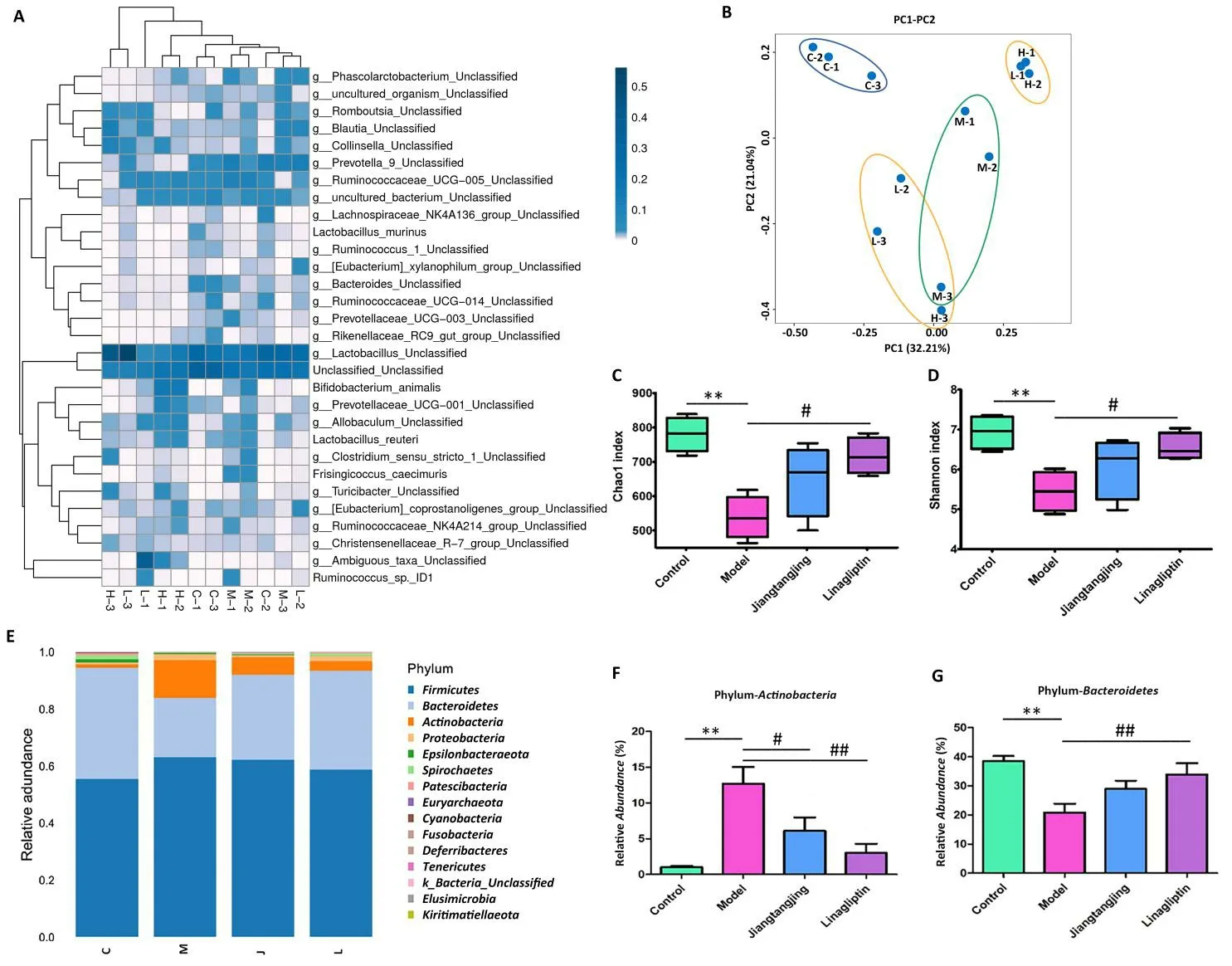
Figure 6 Jiangtangjing granules improve the richness and diversity of the intestinal microbiota.The richness and diversity indices for the intestinal microbiota of control and diabetic rats, with or without treatment, are shown as a heat map (A).In the heat map, the rows represent single taxa and the columns represent the groups, with three samples per group (indicated as #1, 2 and 3), and the color of each square represents the relative abundance of each taxon in each row.High abundance is displayed as blue and low abundance is displayed as white.The similarity of the species diversity among the groups is indicated using principal co-ordinates analysis (B).The distance between sample points represents the similarity of the microbial communities in the samples.The smaller the distance between the points, the higher the similarity.The Chao1 index and Shannon index show the diversity and richness of the intestinal microbiota in the control and diabetic rats.**P < 0.01 represents comparison with the control group;#P < 0.05 represents comparison with the model group (C & D).Jiangtangjing granules affect the composition of the intestinal microbiota in diabetic rats.The relative abundances of the dominant bacterial phyla in rat feces from control and diabetic rats, with or without treatment (E).The distribution of the phylum Actinobacteria (F) and the phylum Bacteroidetes (G) in each group.PC1, principal coordinate 1; PC2,principal coordinate 2; C-1, 2, 3, three samples from control group; M-1, 2, 3, three samples from model group; L-1, 2, 3, three samples from Linagliptin group; H-1, 2,3, three samples from Jiangtangjing group.
Jiangtangjing affects the composition of the intestinal microbiota of diabetic rats
We also assessed the relative abundances of fecal microbial phyla.In general, the bacterial composition of the samples was similar with respect to the phyla present, but the relative abundance of each phylum varied.As shown in Figure 6E, the bacterial phyla present in the rat feces includedFirmicutes,Bacteroidetes, andProteobacteria.FirmicutesandBacteroideteswere the most abundant phyla in the control rats.The relative abundances ofFirmicutesandActinobacteriawere significantly higher and that ofBacteroideteswas lower in the diabetic rats than in that control rats.Jiangtangjing and Linagliptin both affected the relative abundances of these phyla.Jiangtangjing treatment reduced the relative abundance ofActinobacteria(P< 0.05)but increased that ofBacteroidetes(P< 0.01), which was similar to the effects of Linagliptin (Figure 6F and Figure 6G).This implies that Jiangtangjing granules affect the intestinal microbiota of diabetic rats.
Discussion
DM is a metabolic disease that is characterized by hyperglycemia, the result of a deficiency of insulin secretion and/or impaired insulin action.Diabetes-related symptoms also characterize “Xiaoke” in the theory of TCM [25].It has been reported that a Yin deficiency and dryness heat are the typical manifestations of DM and the weakness or dysfunction of the spleen and stomach is a principal feature of the pathogenesis of this disease.A therapeutic effect can be achieved by regulating the function of the spleen and/or stomach of diabetic patients [26].Therefore, the function of the spleen and/or stomach may represent a target in the treatment of diabetes.
Jiangtangjing granules are a promising candidate for the treatment of T2DM, according to the long-term results of their clinical use at Nantong Hospital of Traditional Chinese Medicine of Jiangsu Province,and because they represent a treatment that follows the spleen theory of TCM.Astragali Radixis the principal ingredient in this preparation,and improves yang and improves vital energy.Polygonati Rhizoma,Coicis Semen, andPuerariae Lobatae Radixare the synergistic components that nourish Yin and remove lung heat, correct dryness,and quench thirst.Dioscoreae Rhizoma,Crataegi Fructus,Hirudo, andSemen Brassicaeare adjuvant substances that improve blood stasis and clear collateral vessels [27].Our clinical experience of the use of Jiangtangjing granules suggests that they reduce blood glucose concentration and improve the lipid profile of older adults with T2DM,as well as increasing the serum GLP-1 concentration of patients with T2DM.However, the hypoglycemic effect of Jiangtangjing granules requires more detailed study and the underlying mechanisms remain to be identified.In the present study, we induced diabetes in rats by HFD-feeding for 4 weeks and the intraperitoneal injection of streptozocin, and this was confirmed by a significant increase in FBG concentration (≥16.7 mmol/L).Jiangtangjing granules significantly reduced the FBG of the diabetic rats and also reduced the concentrations at the 0.5, 1, and 2-h time points of OGTT.Their hypoglycemic effect was only slightly weaker than that of Linagliptin,suggesting that Jiangtangjing granules represent an effective means of improving the glucose tolerance of diabetic rats.HbA1c reflects the mean blood glucose concentration over 2-3 months, and we found that Jiangtangjing treatment also significantly reduced the serum HbA1c of the diabetic rats.This suggests that Jiangtangjing granules have beneficial effects on glucose metabolism.
GLP-1 has been shown to regulate blood glucose by stimulating glucose-dependent insulin secretion and inhibiting glucagon secretion.Furthermore, GLP-1 and glucagon-like peptide-2 have become important targets in the treatment of T2DM, obesity, and intestinal diseases [23].In the present study, we measured the serum GLP-1 and insulin concentrations during OGTT and found that the reduction in serum GLP-1 5, 10, and 15 min after glucose administration to diabetic rats could be significantly ameliorated by Jiangtangjing granules.In addition, they ameliorated the high fasting insulin concentration of the diabetic rats, but increased the serum insulin concentrations after glucose administration.These data imply that Jiangtangjing granules may improve insulin secretion by affecting the production of GLP-1 in diabetic rats.We also measured the expression of GLP-1 protein in the jejunum of the rats, and found that it was lower in diabetic rats than in control rats.However, Jiangtangjing treatment increased the jejunal expression of GLP-1 in the diabetic rats, which is also consistent with Jiangtangjing granules promoting insulin secretion by upregulating GLP-1 expression in the jejunum.
We next aimed to identify the signaling pathway involved.The GLP-1 receptor is a G protein-coupled receptor, and cAMP is its principal second messenger.The cAMP/PKA signaling pathway regulates glucose homeostasis at multiple levels, including via insulin and glucagon secretion, glucose uptake, glycogen synthesis and breakdown, gluconeogenesis, and the neural control of glucose homeostasis [28].Binding of ligand to the GLP-1 receptor activates the cAMP/PKA signaling pathway: it results in the activation of adenylate cyclase and an increase in intracellular cAMP concentration.This higher cAMP concentration causes PKA activation, and therefore the opening of voltage-dependent Ca2+channels and the influx of Ca2+.In addition, Epac signal transduction is activated, which stimulates Ca2+efflux from the endoplasmic reticulum.These changes promote insulin secretion [29, 30].Therefore, we hypothesized that Jiangtangjing granules affect insulin secretion by activating the GLP-1-associated cAMP/PKA signaling pathway.In the present study,we measured the expression of cAMP, PKA and Epac1 and found that the high expression of cAMP, PKA and Epac1 in the diabetic rats was significantly reduced by Jiangtangjing granules, which implies that they ameliorate diabetes by activating the GLP-1-related cAMP/PKA signaling pathway.
Growing evidence implicates the gut microbiome in the effects of diabetes.The effects of the gut microbiome on bowel permeability,endotoxemia, and bile acid metabolism are closely associated with insulin resistance and diabetes [31].The intestinal and plasma GLP-1 concentrations of rodents are increased by probiotics (BifidobacteriumanimalisandBifidobacterium bifidum) [32] and some composite prebiotics [33], whereas GLP-1 depletion in rodents alters the composition of the enteric microbiota [34].This suggests that the gut microbiome affects GLP-1 production, and thereby the development of diabetes.In the present study, we found that Jiangtangjing treatment increases the serum GLP-1 concentration and the jejunal expression of GLP-1 in diabetic rats, which may be attributed to changes in the composition of the gut microbiome.The most abundant bacteria in the intestines of Sprague-Dawley rats includeFirmicutes,Bacteroidetes,Proteobacteria, andActinobacteria[35].Firmicutesare fat-digesting bacteria that increase in abundance in obesity.Bacteroideteshave an important role as producers of short-chain fatty acids, whileActinobacteriaare responsible for the biodegradation of resistant starch.Therefore, changes in their relative abundance are closely related to the development of diabetes [36].Previous studies [37, 38]have shown that the abundances ofFirmicutesandActinobacteriapositively correlate with FBG, whereas those ofBacteroidetesandProteobacterianegatively correlate.A highBacteroidetes/Firmicutesratio is associated with greater GLP-1 secretion and an amelioration of diabetes.In the present study, Jiangtangjing granules increased the richness and species diversity of the microbiota, which had been suppressed by diabetes.In addition, along with the lower GLP-1 secretion and expression, the relative abundances of theFirmicutesandActinobacteriawere significantly higher in diabetic rats, which may be attributed to insulin resistance.However, treatment with Jiangtangjing granules increased the abundance ofBacteroidetesand reduced that ofActinobacteria, which implies that Jiangtangjing granules regulate the composition of the intestinal microbiota in diabetic rats.
Conclusion
Jiangtangjing granules reduce FBG, improve glucose tolerance,increase serum GLP-1 concentration, increase jejunal GLP-1 expression, increase the expression of components of the GLP-1-associated cAMP/PKA signaling pathway, and affect the composition of the intestinal microbiota of diabetic rats.Specifically,they increase the relative abundance ofBacteroidetesand reduce that ofActinobacteria.These findings provide insight into the mechanism whereby Jiangtangjing granules have beneficial effects in patients with T2DM and provide a theoretical basis for the expansion of the clinical use of Jiangtangjing granules.
 Traditional Medicine Research2022年1期
Traditional Medicine Research2022年1期
- Traditional Medicine Research的其它文章
- The artificial intelligence watcher predicts cancer risk by facial features
- Evaluation of bioactive flavonoids in Citri Reticulatae Pericarpium from different regions and its association with antioxidant and α-glucosidase inhibitory activities
- Exploring the anti-diabetic effects and the underlying mechanisms of ethyl acetate extract from Sophora flavescens by integrating network pharmacology and pharmacological evaluation
- Effects of Shenling Baizhu powder on endoplasmic reticulum stress related signaling pathway in liver tissues of nonalcoholic fatty liver disease rats
- Artificial neural network techniques to predict the moisture ratio content during hot air drying and vacuum drying of Radix isatidis extract
- Safety of Lycium barbarum L.:more information needed
