A Topic Paper on Flexor Tendon Repair:A Theoretical and Evidence—Based Approach
FELDHACKER Diana R.,LOHMAN Helene,BRACCIANO Alfred
Department of Occupational Therapy,Creighton University,Omaha,Nebraska 68178,USA
ABSTRACT For occupational therapists treating individuals with hand dysfunction,including flexor tendon repairs(FTR),it is necessary to incorporate research evidence,clinical experience,and theoretical concepts to clinically and professionally reason through evaluation and intervention.Central to guiding treatment should be occupation-based theory,as this ensures that occupation,or meaningful activities,is a core emphasis.However,providing occupation-centered therapeutic interventions is uniquely more challenging in orthopedic settings where medical and biomechanical approaches,or treatment grounded on remediation of strength and range of motion,primarily guide intervention.This topic paper uses a guided case study for a client with a zone 2 FTR,the most typical type of flexor tendon injury.Readers are guided through the clinical and professional reasoning with review of research evidence;discussion of occupation-based,tissue healing,and biomechanical theories;and application to client evaluation and intervention.Therapist intent of being client-and occupation-centered is evidenced throughout the case,with a focus on understanding the client and their perception of how the injury impacts their life.The reader is guided through identification of a specific treatment protocol for flexor tendon repair which is based on sound research evidence.This protocol is integrated with occupational,biomechanical,rehabilitative and tissue healing theories in order to provide effective intervention which meets the client's goals.Ultimately,the case study illustrates how therapy should be client-centered,evidenced-based,and grounded in theory with occupation at its foundation.
KEY WORDS flexor tendon repair;evidence-based;occupational therapy;client-centered
As an evidenced-based,client-centered profession,occupational therapy clinicians incorporate clinical research and experience to implement therapeutic interventions for clients with orthopedic hand injuries.Combining theoretical concepts with research evidence provides a foundation for informed decision making regarding therapeutic treatment options and approaches[1].Theory guides clinical evaluation and intervention by establishing parameters for where to focus,how to explain the significance of findings,and how to monitor progress and,outcomes[2].Occupation-based theories focus upon an individual's ability to engage in everyday life activities.It is this engagement that brings purpose and fulfillment to a person's life,enables health,organizes behavior,and improves quality of life[3].Occupation-and activity-based approaches demonstrate that engagement in meaningful occupation is associated with improved well-being,life satisfaction,and physical and emotional health[3-5].Meaningful occupations which impact overall health include self-care[activities of daily living (ADLs)and instrumental ADLs (IADLs)],health management,rest and sleep,leisure and recreation,social participation,employment and work,and education[6-7].
Occupation-centered or activity-based therapeutic interventions are uniquely more challenging in orthopedic or hand therapy settings where a medical and biomechanical approaches may organize and guide treatment.A biomechanical approach addresses remediation of strength,range of motion (ROM),or endurance to facilitate functional activities and tasks.A medical approach focuses on identifying and treating specific anatomical structures and functions.However,occupation-and activity-based methods are more holistic,client-centered,motivating,and meaningful.Grounding occupational therapy practice in theory is what differentiates it as a profession instead of a technical discipline and makes intervention effective and meaningful[8].In treating clients with complex characteristics and individualized needs,therapists must rely on multiple sources of knowledge,combining several theoretical models to fully address all issues and predict outcomes.For example,this might include combining occupational,biopsychosocial,and biomechanical approaches to provide treatment.Initially,the therapist may intervene through biomechanically based preparatory activities,such as ROM exercises and therapeutic ultrasound to facilitate tissue healing.Such activities prepare clients to actively participate in meaningful activities or occupations later.This is illustrated in the intervention portions of the case study.
Theory and research evidence serve to inform occupational therapy evaluation and treatment.Evidencebased practice uses clinical research evidence to make decisions about the provision of therapy services[9].Critically evaluating research ensures delivery of the most effective interventions which emphasize occupational performance[9].Use of research evidence and occupational therapy theory provides a unique perspective and occupation-based approach to facilitate healing and functional performance in patients with orthopedic hand injuries.
The purpose of this topic paper is to explore theoretical and evidence-based practice approaches in hand therapy through use of a guided case study for a client with a flexor tendon repair(FTR).
1 Case study
The use of theoretical and evidence-based practice is represented through a single case study.
1.1 Case introduction
ZHANG Wei is a 28-year-old male employed as an accountant at a major technology firm.He sustained a traumatic laceration of the flexor tendon of his right index finger when he was washing the dishes and reached into the sink,cutting himself on a broken glass hidden beneath the soapy water.Because he was bleeding heavily,ZHANG asked his roommate to take him to the hospital.There,he was informed by the physician that he sustained a flexor tendon injury zone 2 (refer to figure 1)[10],requiring surgery the next day.The surgeon performed a 2-strand suture technique.Following surgery,ZHANG was placed in a dorsal cast that kept his wrist in a slightly flexed position.The physician ordered to have occupational therapy evaluate and treat ZHANG.
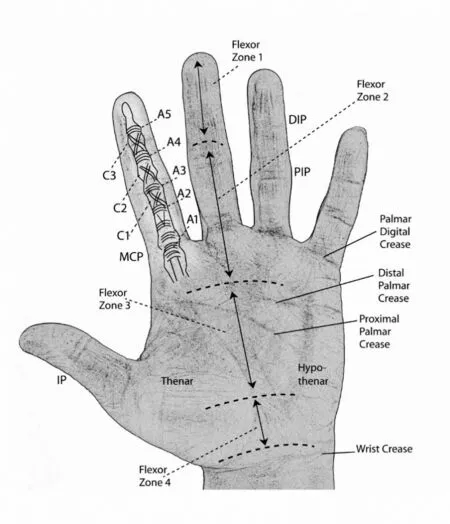
Figure 1 Zones and anatomical structures of the hand(reprinted by permission from author)
1.2 Initial case review
Management of a flexor tendon repair involves understanding theory and evidence related to occupational therapy,anatomy,tissue healing,surgical approaches,and protocols.Frequent communication with the surgeon to determine the appropriate therapeutic approach is essential.A collaborative,team-based approach involving the surgeon,hand therapist,and patient should be used[11].Because of the challenges and risks for treating FTR,it is generally advised to have an experienced and certified hand therapist provide intervention for the best clinical results[12].If an experienced therapist is not available,the therapist should consult with a mentor.However,if a mentor is not available,then the therapist should complete a literature search,review the surgical report,and consider a conservative passive motion approach,such as the Modified DURAN[13]or the Combined DURAN and KLEINERT approach[14].
For ZHANG,the surgeon utilized a 2-strand suture approach.Such an approach typically warrants a more conservative therapeutic protocol,as the tensile strength will not withstand a more aggressive approach.The occupational therapist who received the referral for ZHANG is not a certified hand therapist and has limited experience in treating FTR zone 2.The therapist has limited access to a mentor and thus conducted a review of the literature and surgical report.The therapist noted several options to approach therapeutic interventions following zone 2 FTR,as outlined in the below research evidence.
2 Research evidence
Zone 2 is located between the center of the middle phalanx to the distal palmar crease (refer to figure 1).Within this zone are both flexor tendons and vascular structures (veniculi),encased in a tight flexor sheath consisting of annular and cruciate pulleys.In the past,zone 2 flexor tendon injuries were challenging to treat because of the numerous anatomical structures in close proximity.Repair within this zone often resulted in a high risk for scar tissue,rupture,and gapping which led to a non-functional finger and limited grasp for daily activities.Up until the 1970s,individuals who underwent FTR were often immobilized post-surgery.This immobilization resulted in adhesions (scar tissue) and little functional movement following healing.
In the 1970s two well-known passive motion protocols were introduced by DURAN and HOUSER[15]and KLEINERT and colleagues[16].At that time surgeons were only performing 2-strand repairs.Both protocols involve a dorsal blocking,forearm-based orthosis that prevents metacarpophalangeal (MCP) extension and positions the wrist in neutral-to-partial flexion (refer to figures 2 and 3).Blocking MCP extension places the finger in a protected position to prevent rupture while allowing structures to heal.Within the orthosis,the interphalangeal (IP) joints can flex but cannot extend beyond the limits of the orthosis.The DURAN and HOUSER[15]protocol involves controlled passive range of motion (PROM) exercises which allow 3 to 5 mm of tendon glide,helping to prevent adhesions.A more recent adaption of the DURAN and HOUSER protocol is the Modified DURAN approach[13]which includes a specific exercise regimen of passive and active exercises along with a dorsal protective orthosis.The KLEINERT early passive mobilization protocol includes a dorsal blocking,forearm-based orthosis with a rubber band traction system,allowing passive flexion and active extension of the injured finger within the confines of the orthosis[16].These passive motion protocols continue to be used and recommended today with current practice[17].
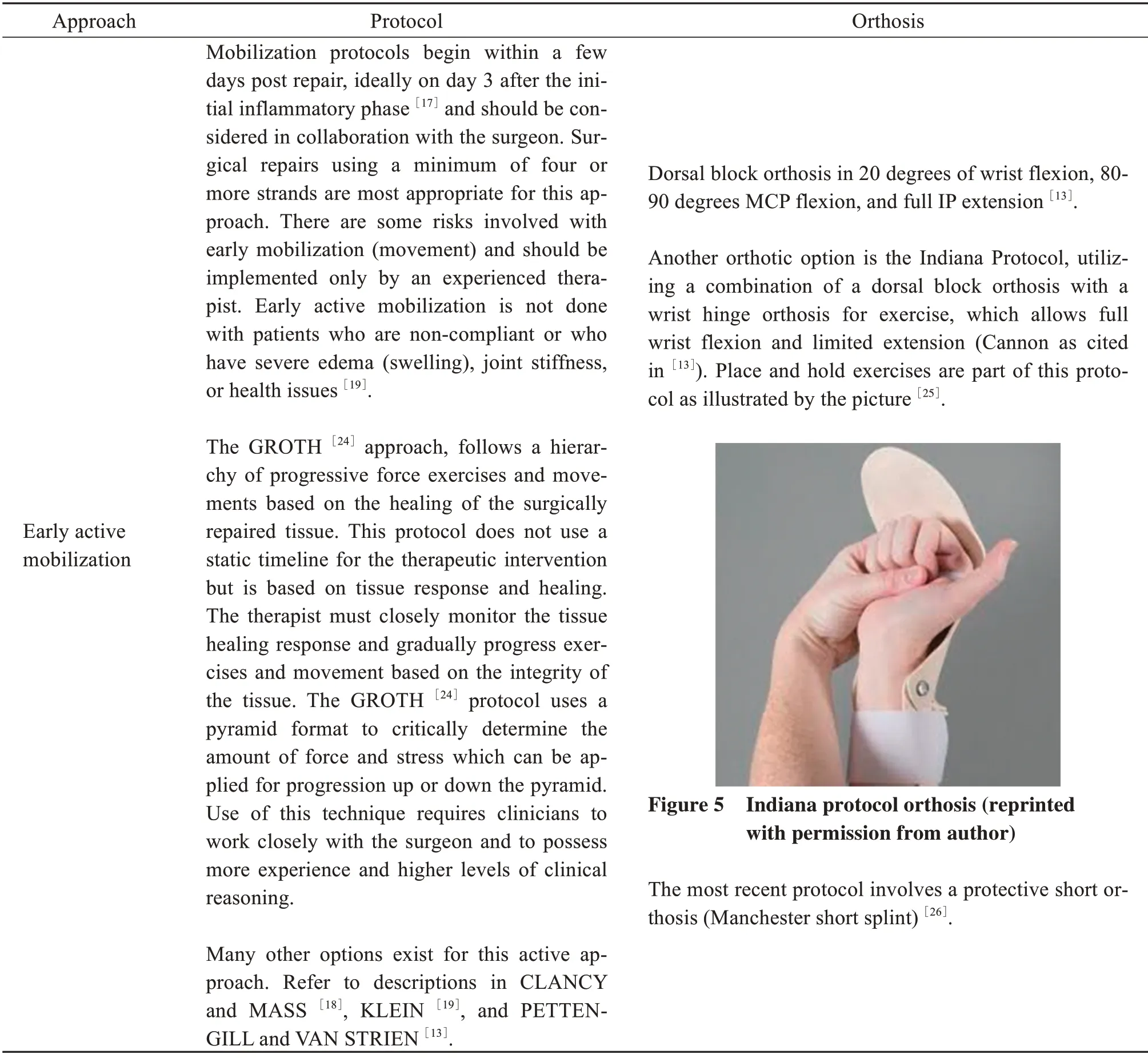
Newer approaches,such as those promoting early active movement or mobilization,have developed as a result of advanced surgical techniques with stronger and improved sutures.Early active mobilization protocols are currently being applied more frequently by experienced hand therapists,with one survey study identifying that hand therapists used these protocols in 79.7% of their cases[17].These active protocols are purported to provide better tendon excursion and differential glide from other tendons in close proximity than the traditional passive protocols[12],and a randomized controlled study supports their usage.
Regardless of the protocol selected for FTR,the objective is to promote healing,decrease adhesions(scar tissue),develop a smooth tendon glide without tendon gapping,and ultimately obtain a functional hand.This allows the individual to complete all activities by the end of the healing process because of the implementation of these early movement(passive or active)protocols.
Protocol options are divided into three approaches:immobilization,early passive mobilization,and early active mobilization.Table 1 provides an overview of commonly used protocols for FTR.The reader is encouraged to review the literature which outlines the full protocols in-depth and provides additional approaches for early,intermediate,and late stages of healing.
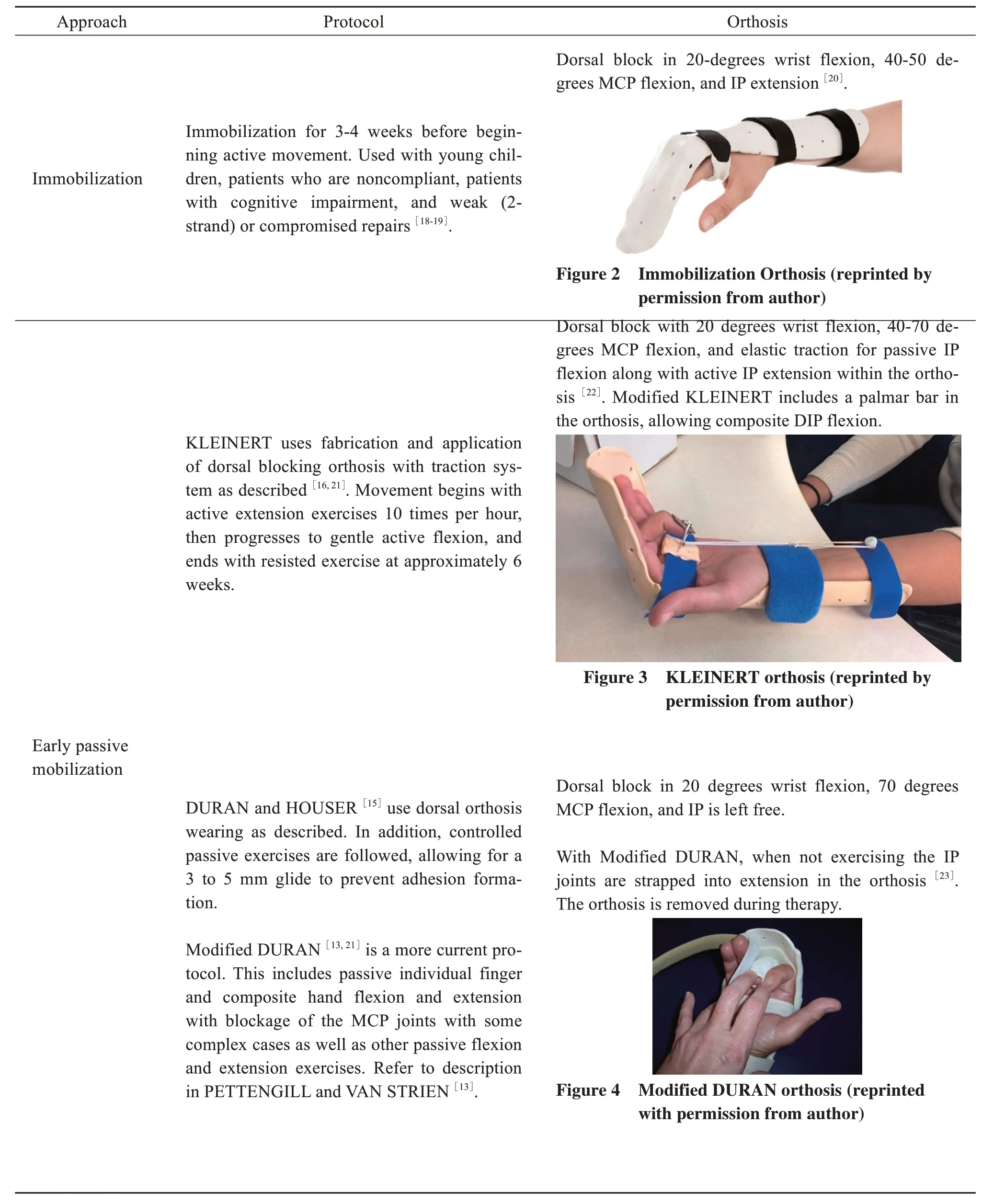
Table 1 Overview of clinical protocols and approaches for treatment of flexor tendon repair
With such variety of protocols for rehabilitation,agreement on management among surgeons and therapists remains controversial[17,27].Systematic reviews and other research can help guide approaches for intervention.STARR et al.[28]evaluated 34 studies which met inclusion criteria,exploring complications and ruptures among passive,active,and immobilization approaches.Investigators found that passive protocols,such as DURAN and KLEINERT,resulted in 4% rupture and 13% complications.Although the PROM protocols had a statistically significant decreased rupture rate,they had an enhanced possibility of decreased ROM.In comparison,active protocols resulted in 5% rupture and 11% complications.Successful use of these active protocols,however,was dependent upon surgical techniques and suture material.Finally,immobilization protocols resulted in 16%complications and 16% rupture rate,proving to be the least effective approach[28].This finding is consistent with a fundamental research study in which immobilization protocols were the least effective approach[29].
CHESNEY et al.[14],in their systematic review,analyzed the primary outcome of rupture rate and secondary outcomes of ROM and quality of life with FTR of zone 2 injuries.Fifteen studies that met their inclusion criteria were evaluated over a 7-year time period.Specifically,authors reviewed KLEINERT,DURAN,combined KLEINERT and DURAN,and active motion protocols.The combined KLEINERT and DURAN protocols had the lowest rupture rate,and the KLEINERT protocol had the highest rupture rate.However,the researchers suggest that the high rupture rate with the KLEINERT protocol might have been skewed by the result of one study's report.The combined KLEINERT and DURAN protocols and the early active motion protocols had good to excellent results with acceptable ROM scales.
NEIDUSKI and POWELL[27]identified nine intervention studies meeting criteria for their systematic review.They examined which exercise approach (early passive,place and hold,or active exercises) resulted in the best outcomes for safe and maximal range of motion.Place and hold exercises involve manually placing the injured finger in a flexed position and then having the person try to maintain the position.Findings of moderate to strong evidence were that place and hold exercises had better results than passive flexion protocols like DURAN and KLEINERT.Despite this,investigators concluded that there is not strong enough evidence to support a true active motion approach for rehabilitation
3 Case intervention planning
After reviewing the literature,the occupational therapist consulted with the surgeon to discuss the protocol and therapeutic approach appropriate for ZHANG's case.Given research evidence,the 2-strand surgical approach,and the therapist's lack of experience,the team chose to follow a combined DURAN and KLEINERT approach[14].Evidence of this treatment has resulted in good clinical outcomes and lower rupture rates[14],making it an appropriate choice for ZHANG's case.The combined DURAN and KLEINERT approach is based on early passive mobilization and combines elements of both passive motion protocols:passive flexion and active extension exercises(KLEINERT) and passive flexion and passive extension(DURAN)within a dorsal block orthosis.
In addition to exploring the literature related to intervention protocols,it is important that the occupational therapist understand and integrate biomechanical,rehabilitative,and tissue healing theories,along with research evidence,in order to organize their clinical reasoning and approach to evaluation and treatment.Along with this,a critical component of developing goals and objectives for ZHANG will be to discuss and consider his interests,abilities,and the environment in which he lives and works.Addressing these any concerns and issues related to movement and functional tasks and activities must be addressed as part of the therapeutic goals.Below is the therapist's review of occupational,tissue healing,and biomechanical theories which will impact ZHANG's plan of care.
4 Occupation-based theory
Using occupation-based theory to guide practice,including treatment of FTR,means ensuring that all evaluation and intervention focuses upon the individual's ability to engage in meaningful occupation.The occupational therapist should use the domain of practice to evaluate and understand ZHANG Wei's important occupations and roles,contexts and environments,client factors,and performance skills[6].Research has shown that hand injuries have a major impact on daily routines and quality of life,leading to experiences of depression and frustration[30].A study by KASKUTAS and POWELL[31]found that 59% of participants removed their orthoses to use their affected extremity to complete daily activities.Participants in the study reported that few therapists addressed the individuals' abilities to perform meaningful activities and participate in life roles during the time of tissue healing and restricted extremity use[31].A desire and need to complete daily activities with the extremity too soon after surgery can lead to potential injury,such as tendon rupture.Patient education should include specifying wearing schedule of the orthosis and correct movement,force,and grasp based on the stage of tissue healing,in alignment with the protocol being used.Thus,the therapist should combine these occupation-based concepts with an understanding and mastery of tissue healing and biomechanics to develop an effective intervention plan.
5 Tissue healing and biomechanics theory
A primary goal of rehabilitation following tendon repair is to achieve function and gliding but avoid rupture of the tendon[32].The body's response to injury or surgery is a dynamic series of events at a micro and macro level.Surgical procedures impact soft tissue structures,and healing is the body's attempt to repair and replace injured or damaged tissue,returning the involved structures to homeostasis and function.Abnormal or excessive wound healing can occur which can complicate the rehabilitation process.Examples include conditions such as fibrosis,adhesions,contractures,and inadequate wound healing[33].For ZHANG's occupational therapist,understanding the biophysiological response to therapeutic interventions and the impact on body systems and structures is critical in developing appropriate goals and therapeutic responses to musculoskeletal and orthopedic injuries.
A wound or surgical procedure can cause a pathological state with disruption of the normal anatomical tissue structures,resulting in subsequent loss of function.Healing involves a variety of repair mechanisms as the body attempts to compartmentalize the injury and restore damaged tissue function.Normal wound healing involves three successive but overlapping phases,including inflammatory phase,proliferative phase,and the maturation phase[34].Though these phases follow a general timeline,healing is determined by individual characteristics and can be negatively impacted or slowed due to comorbidities,aging,the presence of foreign objects,infection,poor nutrition,and medications[35].Surgical repair following a rupture or laceration of a tendon is necessary,with best results occurring with early repairs and clean lacerations[32].Successful outcomes are impacted by strength of sutures,level of injury,and other complications such as soft tissue damage,vascular supply,nerve injury,tendon gapping,adhesion,edema,and contracture[36].
The initial response to tissue or tendon injury is inflammation.The inflammatory stage consists of vascular and cellular components,lasting up to one week following injury[37].First,vasodilation flushes the area and removes foreign bodies and necrotic tissue to prevent infection.Vasoconstriction follows with aggregation of platelets,blood coagulation,and an encapsulation of the impacted area to compartmentalize and limit further damage.Fluid from the vascular system is released along with histochemicals such as histamine,prostaglandins,bradykinins,and growth factors,causing an increase in hydrostatic pressure and swelling,initiating repair[38].The inflammatory process is characterized with the classic signs of redness,heat,swelling,associated pain,and changes in skin color with red,blue,or purple tissue discoloration.Inflammation prepares the wound for the proliferative phase of healing.Prolonged inflammation can lead to the development of scar tissue and decreased range of motion,while too little inflammation can delay healing.The primary therapeutic goal during the inflammatory phase is to decrease or minimize factors which could prolong or prevent inflammation.
The proliferative phase of healing,which lasts approximately 3 weeks,overlaps with inflammation,epithelialization,fibroplasia,and angiogenesis.During the proliferative phase,fibroblasts synthesize collagen molecules,providing a matrix of cross-linked connective tissue which fills in the wound bed and begins to strengthen the tendon and soft tissue in a non-organized fashion[34].Though the tendon is strengthened,integrity is primarily maintained through the surgical sutures.Rupture is still a risk,and precautions must be taken in therapy to limit applying too much force to the healing structures.During this stage as tissue heals and strengthens,controlled motion can be initiated.
The maturation phase of healing begins at approximately 21 days post injury and continues for up to two years.During the maturation phase,the new tissue is modified as the collagen fibers reorient along the length of the tendon,resulting in gains in strength and flexibility.Collagen fibers mature to assume the characteristics of the tissues which they are replacing[34].As healing progresses beyond 6 weeks,resistance can be gradually added to the therapeutic protocol.However,if the patient has good active motion,care must be taken to avoid overuse and excessive resistance to prevent rupturing the repair.During this stage tensile strength,or the amount of force that a tendon can tolerate without rupture,continues to increase[19].During the maturation phase new tissue is fragile but slowly gains strength and flexibility through remodeling.When fully remodeled,the new tissue has approximately 80%of the tissue's pre-injured strength.At approximately 12 weeks post-surgical repair,the tendon will have enough tensile strength to complete most functional tasks and activities safely[19].The goal of rehabilitation during the maturation phase is to achieve function and gliding while continuing to avoid rupture of the tendon.In addition,therapists must manage post-surgical complications such as adhesion formation(scar tissue)and joint stiffness.
Repair with sutures helps strengthen the laceration site,decrease gap formation,and promote more effective healing[34].As such,surgeons consider various types and sizes of suture as well as number of strands within the repair in order to facilitate repair for functional use.In general,the greater the number of sutures placed,the stronger the tendon repair should be.As such,it is imperative that the treating occupational therapist review and understand the surgical approach as this impacts the clinical decision-making process for intervention and treatment.After repair,the primary focus of therapeutic intervention is to maintain integrity of the repair site,facilitate the healing process,and prevent infection with proper wound care.Clinical approaches should promote strengthening of the tendon while preventing scarring of surrounding structures which would limit function and range of motion.Therapeutic approaches work to balance healing,scarring,strengthening,and gliding[37].In considering the healing process,it can be understood why immobilization after repair of flexor tendons can lead to adhesions (scar tissue) and decreased function.Initial passive motion by applying established therapeutic protocols has instead been shown to improve function through understanding these wound healing and biomechanical principles[37].In summary,early controlled movement with consideration of surgical intervention and protocols facilitate functional return and structural integrity.
6 Case evaluation and intervention
Following surgery,ZHANG was initially casted.Upon removal of the cast,ZHANG was referred to occupational therapy for evaluation and treatment.The occupational therapist first developed an occupational profile to obtain further insight into ZHANG's background,perceptions,and priorities[6].From the occupational profile the occupational therapist determined that ZHANG is most worried about being able to return to work as soon as possible as well as take care of himself.His roommate also works and is unreliable help,so it is important to ZHANG to be independent in basic self-cares.ZHANG has limited time off from his job and requires income to pay his bills.It is also the busy season at work,and ZHANG worries that being off will negatively impact other co-workers.Understanding these factors are important for the occupational therapist to address in developing ZHANG's plan of care.
In the first therapy session,the occupational therapist fabricated an orthosis according to the selected Modified DURAN and KLEINERT protocols[13,21].This orthosis included a dorsal block with 20 degrees of wrist flexion,40-70 degrees of MCP flexion,and elastic traction for passive IP flexion along with active IP extension within the confines of the orthosis.Following the KLEINERT approach ZHANG performed active extension exercises with the traction system pulling his finger passively into flexion.ZHANG was further instructed in PROM exercises within the orthosis and active extension from a flexed position within the orthosis,according to the Modified DURAN protocol[21].The therapist showed ZHANG how to move his fingers passively and slowly,being certain to not provide any resistance until deemed appropriate by the surgeon and protocol.The therapeutic focus during these early intervention sessions was to protect the repaired tendon,provide patient education,care for the wound,control edema,and manage the scar[39].ZHANG was educated that light grip and strengthening do not begin until around 6-7 weeks based on the healing process,protocol,and surgeon clearance.The therapist spent extra time educating ZHANG about wound healing and the purpose of the protocol to aid in his understanding of the need for precaution with early movement to prevent tendon rupture.
The occupational therapist considered the integration of biomechanical,rehabilitative,and tissue healing theories and evidence to organize their clinical reasoning and approach to evaluation and treatment.A critical component of developing goals and objectives for ZHANG is to discuss and consider his interests,abilities,and the environment in which he lives and works.ZHANG is concerned about his ability to care for himself and return to work.Addressing these occupational concerns and issues related to movement and functional tasks and activities must be addressed in the therapeutic approach.
After orthosis fabrication and PROM instruction,the therapist discussed with ZHANG a need to modify and adapt his tasks,activities,occupations,environment,and habits to facilitate independence while maintaining safety and integrity of his healing hand[6].Goals were collaboratively set in accordance with ZHANG's priorities related to self-cares and work.Subsequent sessions will continue to focus on tissue healing and protocol advancement as well as therapeutic interventions for one-handed methods to complete self-cares,use of adaptive equipment,and exploration of modifications needed at work and home depending on the stage of healing[31].Conversations in the early stages of therapy can identify goals and objectives for safe and realistic activities which can be progressively included as the tissue heals.This direct communication and collaboration can be motivating for ZHANG.
Following these strategies,the therapist provided evaluation and intervention which utilized wound and tissue healing,rehabilitative,and biomechanical approaches and evidence to guide the therapeutic process to remediate ZHANG's injury.These activities and therapeutic exercises are organized with the goal to return ZHANG to prior function in self-care and work.Clinical experience,theory,and evidence guide use of compensatory and adaptive approaches to encourage early independence in meaningful and necessary tasks and activities while preventing rupture.
7 Conclusion
As a client-centered and science-driven profession,using theory and evidence to guide occupational therapy evaluation and therapeutic intervention is critical.Integrating clinical experience and theoretical concepts in combination with research evidence facilitates clinical reasoning to make informed decisions about treatment goals,objectives,and clinical interventions[1].In the case example,ZHANG experienced a flexor tendon laceration of zone 2,for which he underwent surgical repair.Theoretical underpinnings of occupational therapy,biomechanics,and tissue healing were considered and integrated throughout intervention.Identification of the research evidence and critical review of flexor tendon protocols highlighted the risks and benefits of each,guiding decision making and intervention for the therapist in this case.This process ensured that treatment was provided in a meaningful way,addressing the client's contextual concerns,goals,and objectives.Implementation of this process also ensured that appropriate tasks,activities,and therapeutic exercises were based on the stage of healing and integrity of the anatomical structures.This integration improved functional use of ZHANG's hand,providing a holistic,client-centered,and effective therapeutic approach and intervention.