Clinical characteristics and prognostic factors for visual outcome in 669 patients with intraocular foreign bodies
Yu-Zhu Gao, Yi-Fan Zhang, Ming Zhang, Han-Yue Xu, Xu-Rui Jin
1Department of Ophthalmology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
2Duke Global Health Research Institute, 310 Trent Drive,Durham, NC 27710, Box 905119, Durham, NC 27708, USA
Abstract
● KEYWORDS: intraocular foreign bodies; prognostic factors; visual outcome
INTRODUCTION
Intraocular foreign bodies (IOFBs) is one of the leading causes of ocular disorder and visual loss worldwide[1],which occurs mainly in young men at the working place[2-3].The IOFBs can both cause direct mechanical damage and lead to different intraocular pathology because of complicated nature, resulting in a wide range of complications, which poses complex challenges to the ophthalmologist in evaluation and management for patients.
Some previous studies have presented the characteristics of IOFBs as predictive factors, suggesting their association with visual outcome and management. However, most of them were conducted among the western population and with a limited sample size. Considering the high prevalence of IOFBs in China, it is essential to present the study about the current IOFBs situation.
In this study, we included 669 IOFBs cases from West China Hospital from June 2011 to September 2017 and investigated clinical characteristics of IOFBs and potential prognostic factors influencing the visual outcome.
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective study included 669 patients with IOFBs from West China Hospital between June 2011 and September 2017. This study was approved by Ethics Committee of West China Hospital of Sichuan University and conducted in compliance with guidelines of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.Patients were excluded with a history of prior diseaserelated vision loss, ocular disease or ocular trauma, leading to a final sample of 669 patients. The medical history and ophthalmologic examination of the patients were collected.Patients’ age, gender, mechanism of injury, entry site,characteristics of IOFBs, the time interval between injury and surgery, presenting and final best corrected visual acuities(BCVA) and complications were collected.
BCVA values were recorded using standard Snellen acuity chart and were converted to logarithm of the minimum angle of resolution (logMAR) scale for statistical analysis. The presenting BCVA was taken at patients’ first presenting to West China Hospital while the final BCVA was recorded during follow-up. The visual outcome was defined by the final BCVA(excellent visual outcome: final BCVA of 20/40 or better; poor visual outcome: final BCVA less than 20/200).
Characteristics of the IOFBs included size, location, and nature.The size of IOFBs was divided into three groups: small (less than 4 mm2), medium (4-16 mm2) and large (more than 16 mm2).Depending on the suspected location and nature of IOFBs,different ocular imaging including B-scan ultrasonography,computed tomography (CT), magnetic resonance imaging(MRI) was used for detection at the initial visit.
The Ocular Trauma Score (OTS)[4]was used in this study for patients >15 years of age, which was calculated by summing the raw points based on the following parts: initial vision(no light perception=60 raw points, light perception or hand motion perception=70 raw points, 1/200 to 19/200=80 raw points, 20/200 to 20/40=90 raw points, ≥20/40=100 raw points), and five injury related factors (rupture=minus 23 raw points; endophthalmitis=minus 17 raw points; perforating injury=minus 14 raw points; retinal detachment=minus 11 raw points; and afferent papillary defect (RAPD)=minus 10 raw points). For patients ≤15 years of age, since RAPD could not be evaluated in most of them, the pediatric Penetrating Ocular Trauma Score (POTS)[5]was calculated for evaluation, which includes four parts: initial visual acuity (no light perception=10 raw points, light perception or hand motion perception=20 raw points, counting fingers=30 raw points, 0.1-0.5=40 raw points, 0.6-1.0=50 raw points), age of the pediatric patients(0-5 years old=10 raw points, 6-10 years old=15 raw points,11-15 years old =25 raw points), wound location (zone I=25 raw points, zone II=15 raw points, zone III=10 raw points) and concomitant eye pathologies [iris prolapse=minus 5 raw points,hyphema=minus 5 raw points, organic/unclean injury=minus 5 raw points, delay of surgery (>48h)=minus 5 raw points,traumatic cataract= minus 10 raw points, vitreous hemorrhage=minus 20 raw points, retinal detachment=minus 20 raw points,endophthalmitis=minus 30 raw points]. For patients whose initial visual acuity was not obtained, the following equation was used for adjustment: 2×(age+zone)–corresponding pathologies. Three different groups were compared, which were categorized by final BCVA: Group I (189 eyes): final BCVA was equal to or better than 20/40 Snellen E; Group II(98 eyes): final BCVA was between 20/40 and 20/200 Snellen E;Group III (382 eyes): final BCVA was less than 20/200 Snellen E.Statistical AnalysisStatistical analysis of collected data was performed using IBM SPSS Statistics version 23 (SPSS Inc.,Chicago, IL, USA). Baseline characteristics were presented as a mean (continuous variables) or on a frequency distribution(categorical variables). ANOVA for continuous variables and Chi-square tests for categorical variables were applied to compare the differences among participants with IOFBs.Univariate and multivariate Logistics regression were applied to examine the associations between prognostic factors and visual outcome. A 2-tailedPvalue of less than 0.05 was considered statistically significant throughout the study.
RESULTS
Clinical Characteristics of the Patients with IOFBsTotally 669 patients (669 eyes) were included in this study. Baseline demographic and clinical characteristics for these patients and study eyes were presented in Table 1. The average age ranged from 1 to 79 years old (mean age, 34.8±12.7 SD) and there were more males (626, 93.6%) than females (43, 6.4%). The injuries occurred in 328 left eyes (49.0%) and 341 right eyes(51.0%). Hammering (383, 57.2%) was observed to be the most common cause of IOFBs. The entry sites were from cornea (441,65.9%), sclera (174, 26.0%) and limbus (54, 8.1%).
Totally 55 patients (8.2%) wore eye protection at the time of getting injury and there was significant difference in three groups (P=0.012). In Group I, 58 patients (30.7%) presented with the presenting BCVA better than 20/40, which was significantly more than 13 patients in Group II (13.3%) and 26 patients in Group III (6.8%). The complications were present in the majority of patients (77.3%), however, there was significant difference in the three groups: the complications were present in 74 patients in Group I (39.2%), while nearly in all patients in Group II (84.7%) and Group III (P<0.001).While the average time interval between injury and surgery was 26.4±322.3d (0-7300), it was significantly shorter in Group I (2.7±4.6) than in Group II (3.5±7.1) and Group III(P<0.001). Almost half of patients received surgeries within 24h (327, 48.9%) and most patients received surgeries within seven days (590, 88.2%).
● 联网共享。不仅是单一系统内的摄像机头数量激增,而且多个系统之间的图像信息也需要互通互用。特别是随着监控系统规模的扩大,用户业务需求日趋复杂,典型的如平安城市项目,要实现城市级的信息联网共享,将治安、卡口、电警和社会面监控等视频点统一接入管理,其联网需求、数据存储、业务应用都对管理平台提出了更高要求。
Characteristics of Intraocular Foreign BodiesThe characteristics of IOFBs were illustrated in Table 2, including size, location, and nature. The size of the IOFBs varied as follows: small (≤4 mm2), 25.7%; medium (4-16 mm2), 26.3%;large (>16 mm2), 29.8% and unclear size, 18.2%, where there was significant difference in three groups (P<0.001). TheIOFBs were located mostly in the retina in 165 eyes (24.7%),vitreous body in 144 eyes (21.5%) and cornea or sclera in 107 eyes (16.0%) while there was significant difference in three groups (P=0.001). The nature of the IOFBs showed a variety of properties, including metallic (85.7%) consisting of magnetic(74.7%) and nonmagnetic (11.0%) and nonmetallic (14.3%)comprising of glass (5.8%), wood (4.6%), plastic (2.4%) and stone (1.5%), where there was no significant difference in three groups (P=0.776).
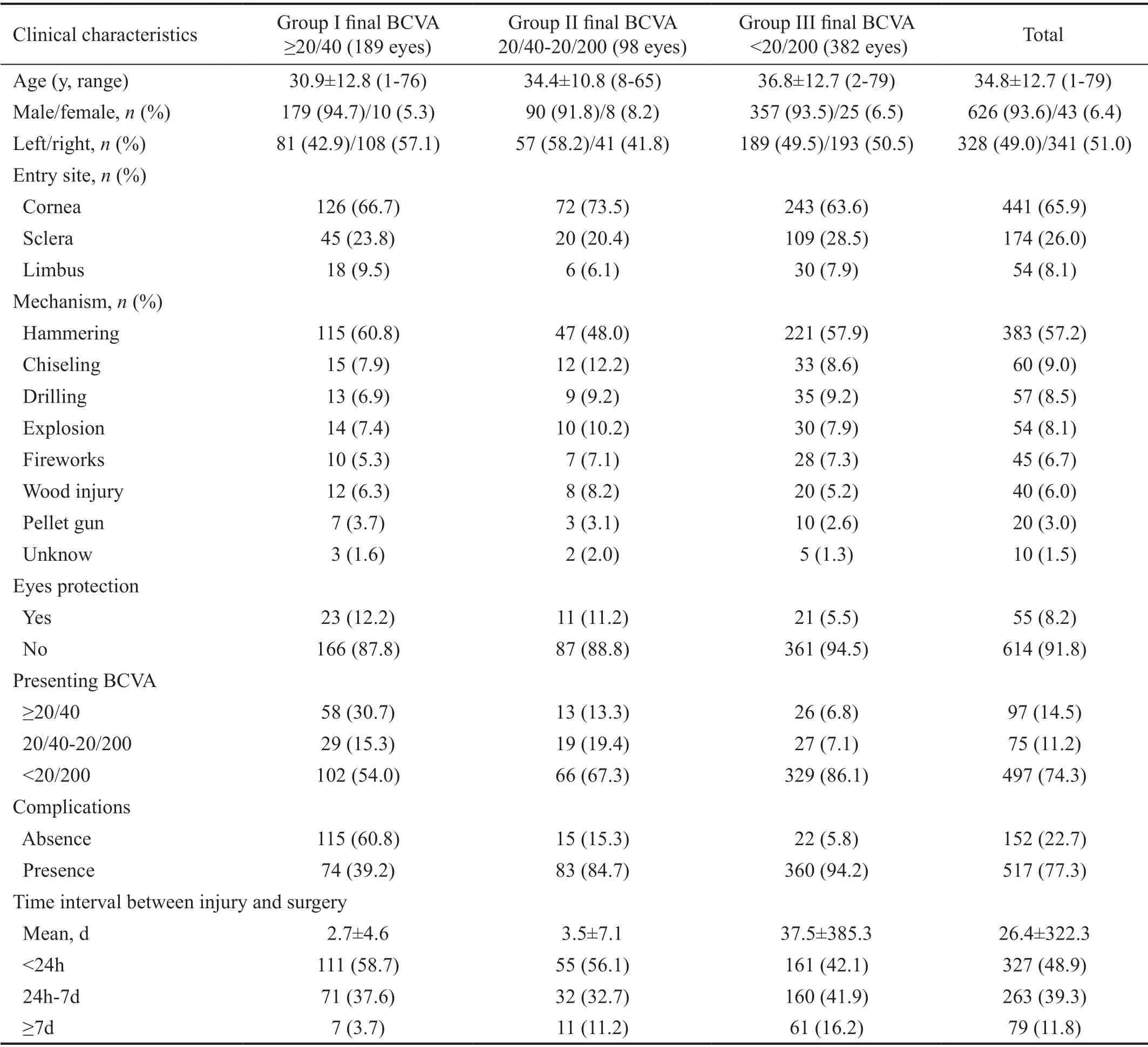
Table 1 Clinical characteristics of the patients with IOFBs
Final BCVA Based on the Ocular Trauma Score or Pediatric Penetrating Ocular Trauma ScoreThe final BCVA based on the OTS or pediatric POTS were shown in the Table 3. The POTS was used in 39 patients and the OTS was used in 630 patients. The patients were divided into five groups based on the sum of raw points: <45 points (149, 22.3%),45-64 points (318, 47.5%), 65-79 points (50, 7.5%), 80-89 points (46, 6.9%) and 90-100 points (106, 15.8%). There was significant difference among there groups (P<0.001).
ComplicationsThe complications of these patients with IOFBs were summarized (Table 4). Among those patients,more than one kind of complications occurred. Further analysis of the data showed a variety of complications: lens injury occurred in more than a half eyes, including cataract in 382 eyes (57.1%), lens subluxation in 12 eyes (1.8%) and lens dislocation in 5 eyes (0.7%). Other main complications included endophthalmitis in 195 eyes (29.1%), vitreous hemorrhage in 56 eyes (8.4%) and retinal injury consisting of retinal detachment in 39 eyes (5.8%), retinal break in 14 eyes(2.1%), siderosis bulbi in 7 eyes (1.0%), retinal contusion in 5 eyes (0.7%) and retinal hemorrhage in 4 eyes (0.6%).
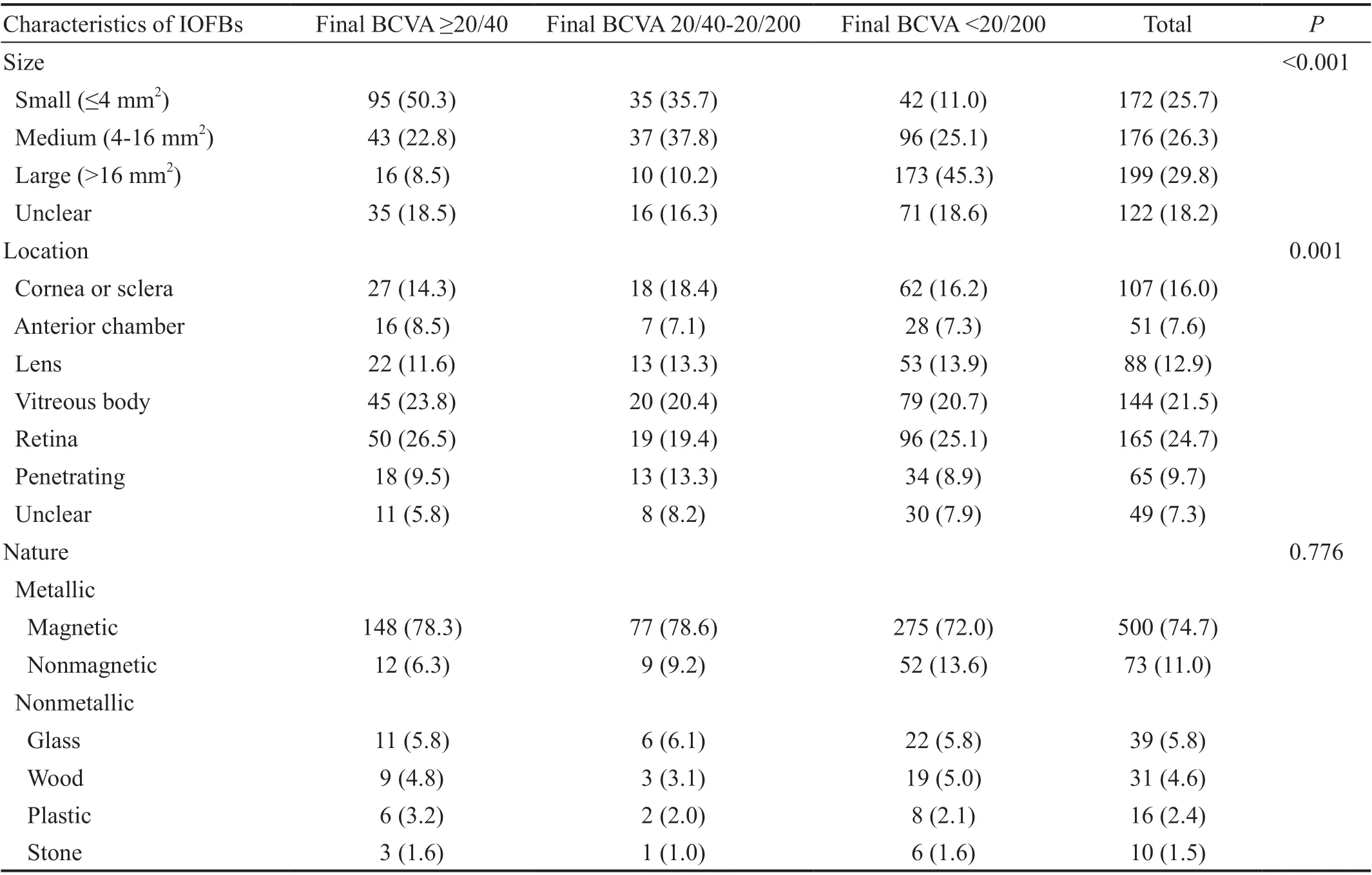
Table 2 Characteristics of IOFBs n (%)
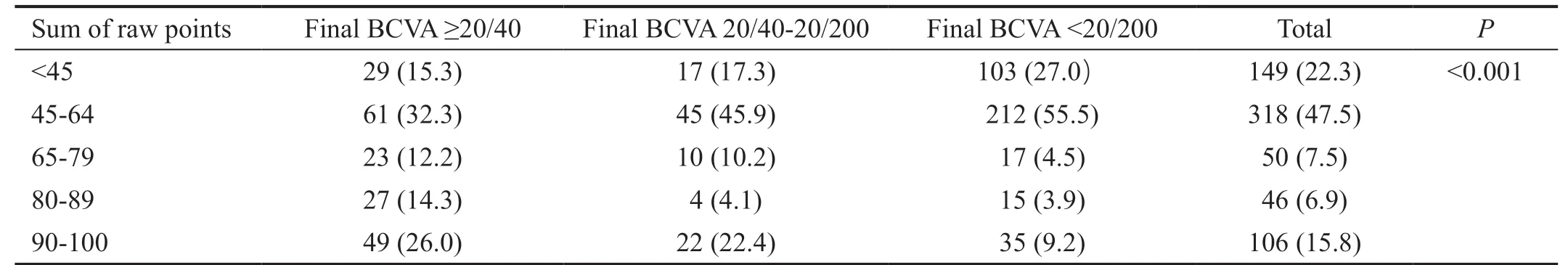
Table 3 Final BCVA based on OTS or POTS
Prognostic Factors for the Visual Outcome According to Univariate AnalysisUnivariate analysis was performed to detect the prognostic factors for the visual outcome. The result(Table 5) revealed that the poor visual outcome (final BCVA<20/200) was associated with older age (P<0.001), worse presenting BCVA (presenting BCVA<20/200;P<0.001), larger size of IOFBs (P<0.001), presence of complications (P<0.001),longer time interval from injury to surgery (P=0.004). For the excellent visual outcome (final BCVA >20/40), younger age(P<0.001), better presenting BCVA (presenting BCVA ≥20/40;P<0.001), the smaller size of IOFBs (P<0.001), absence of complications (P<0.001) and the shorter time interval from injury to surgery (P=0.021) were significantly prognostic factors (Table 6).
Prognostic Factors for the Visual Outcome According to Multivariate AnalysisMultivariate analysis was conducted to identify the prognostic factors influencing the visual outcome.The poor BCVA was associated with older age (P=0.013),worse presenting BCVA (P<0.001), the larger size of IOFBs(P<0.001) and presence of complications (P<0.001; Table 7). On the contrary, younger age (P=0.005), smaller size of IOFBs(P<0.001), absence of complications (P<0.001) and better presenting BCVA (P<0.001) were considered to relate to excellent BCVA (Table 8).
DISCUSSION
IOFBs injury is a significant, preventable health problem all over the world, especially in developing countries. It requires detailed evaluation and skillful management. In this retrospective study,we have provided comparably large and recent cases of the patients with IOFBs from West China Hospital and presented the clinical characteristics of these patients and potential prognostic factors associated with visual outcome.

Table 4 Complications

Table 5 Prognostic factors for poor visual outcome according to univariate analysis

Table 6 Prognostic factors for excellent visual outcome according to univariate analysis

Table 7 Prognostic factors for poor visual outcome according to multivariate analysis

Table 8 Prognostic factors for excellent visual outcome according to multivariate analysis
In addition, the time interval of IOFBs removal was recommended within 24h, which was founded to be associated with visual outcome in the previous studies[8,11]. Our study showed that almost half patients received surgeries within 24h and most patients received surgeries within seven days.In this study, the average time interval between injury and surgery seemed to be longer than that reported in previous studies. However, it depends on several factors. One of the main factors is that in normal conditions, most patients went to hospital nearby which lack of operating rooms and surgeons at the time of injury, which inevitably prolonged the time interval. As reported in previous studies, the availability of experienced surgeons and operating rooms play a significant role[12]. Jonaset al[11]suggested the surgery should be delayed until trained surgeons available in some clinical situation especially in patients with metallic IOFBs. What’s more, for some older patients, overall health status should be taken into consideration, if a patient is not in a good condition,the delaying of surgery is also recommended for a better prognosis.
Many studies considered the OTS and pediatric POTS as effective tools for evaluation and suggested that they were helpful in the prediction of final visual outcome[5,13-14]. In this study, the OTS system and the pediatric POTS system were also used for evaluation of patients with IOFBs and we also founded that in our 669 patients, the OTS and POTS were related to final BCVA.
ManagementOur study suggested that detailed history of patients with IOFBs should be the significant part in the management of IOFBs, if it is reliable, the patients’ perspective may thus be useful for further evaluation and decision making.Moreover, as one of the significant parts in the management of IOFBs, CT is a recommended method used in patients’examination and evaluation in previous studies[2]. Linet al[15]also reported that the sensitivity of the CT image was 90% in the detection of IOFBs and considered CT scan as an important tool in planning the surgical procedures. In our patients, ocular imaging was applied in the majority of the patients with IOFBs for diagnosis and management, and CT scan was the preferred method. Moreover, MRI was also performed in some of our patients when CT missed in the detection of some tiny ferromagnetic IOFBs.
Almost all the patients received surgeries for IOFBs removal and global repair. As shown in the previous study, the closure of the entry site, the removal of the IOFBs and the prevention treatment of endophthalmitis were considered to be on the priority during surgery[16]. Moreover, in some cases, additional surgeries were required for the reconstruction of eyeballs, such as cataract removal and intraocular lens (IOL) implantation when presence of lens injuries.
Prognostic FactorsIn our study, univariate and multivariate analyses revealed that several factors seemed to be related to visual outcome in patients with IOFBs. We found that age was related to visual outcome. Szijártóet al[17], Liuet al[8], and Yanget al[18]have reported that the lager IOFBs was considered to be associated with poor prognosis. We found that the larger size of IOFBs was a significant prognostic factor associated with poor visual outcome and the smaller size of IOFBs was related to excellent visual outcome. Clearly, the larger size of IOFBs suggests the possibility of increasing mass and velocity,proportional to the energy transmitted to eyes, leading to worse tissue damage and worse visual outcome.
Our finding that the presence of complications was significantly related to the visual outcome, which is similar to what reported previously[8]. Considering that the type of complications varies in patients with IOFBs, it is of great importance to clarify the various types during evaluation process. Previous studies suggested that some complications like endophthalmitis[8,19],proliferative vitreoretinopathy[17,20]and retinal detachment[20-21]were predictive of poor visual outcome. Nevertheless, Chiquetet al[21]have indicated hyphema and vitreous hemorrhage did not affect the prognosis in patients with IOFBs. A recent study by Maet al[22]has demonstrated that for patients with complications like traumatic cataract and vitreous hemorrhage,if the macula of them remained integrity, the visual acuity could be improved after IOFBs removal.
Previous studies have demonstrated the importance of presenting BCVA as a prognostic factor in patients with IOFBs[8,16,23]. In our study, better presenting BCVA were also considered to be a prognostic factor for the excellent visual outcome.
Limitations and AdvantagesOur study has further limitations. First, our patients were all from West China Hospital, hence, the situations may differ in other regions.Second, all data were collected through a retrospective review of medical records, leading to the limited information. The primary strength of this study is that the relatively large-scale and recent data were generated. Second, considerably complete data were used both in univariate and multivariate analyses to explore prognostic factors involved in the visual outcome. In addition, considering the significance of the improvement on self-protection and self-health awareness, we also performed a lack of eye protection, which was rarely reported by recent studies.
In this study, we found that multiple prognostic factors might influence the final visual outcome, including age, size of IOFBs, complications and presenting BCVA. Meanwhile,considering that visual outcome is directly related to patients’daily activities, further education and promotion on eye protection should be taken for improvement on self-protection and self-health awareness. Since the patients presenting with IOFBs injury are challengeable and sometimes complicated for the ophthalmologist, we also hope our experience could help them in further work in IOFBs.
ACKNOWLEDGEMENTS
Conflicts of Interest:Gao YZ,None;Zhang YF,None;Zhang M,None;Xu HY,None;Jin XR,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
