Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
Jian-Bo Mao, Cai-Yun Zhang, Chen-Yi Liu, Yun Zhang, Jing-Jing Lin, Zhao-Kai Xu,Yi-Qi Chen, Yuan-Yuan Fan, Shi-Xin Zhao, Li-Jun Shen
1Eye Hospital and School of Ophthalmology and Optometry,Wenzhou Medical University, Wenzhou 325027, Zhejiang Province, China
2Chicago College of Optometry, Midwestern University,Downers Grove, IL 60515, USA
Abstract
● KEYWORDS: central serous chorioretinopathy; conbercept;photodynamic therapy; subfoveal choroidal thickness
INTRODUCTION
Central serous chorioretinopathy (CSC) is a selflimiting condition characterized by localized serous detachment of the neurosensory retina as a result of hyperpermeability of the choroidal vasculature. Typical changes in the retinal pigment epithelium (RPE) can be also present[1-3].In some refractory cases, treatment may be warranted to subside progression or fasten recovery. Photodynamic therapy(PDT), laser photocoagulation, subthreshold micropulse laser,intravitreal anti-vascular endothelial growth factor (VEGF) and antagonists of mineralocorticoid receptors and glucocorticoid receptors may be applied in treating this disease[3].
Numerous studies have shown positive therapeutic effect of PDT in treating chronic CSC[4-6]. With PDT, a rapid resolution of subretinal fluid (SRF) and reduction in subfoveal choroidal thickness (SFCT) can be achieved by reducing choroidal exudation and choriocapillaris blood flow. Later, some complications have been recognized with the use of full-dose PDT such as choroidal capillary nonperfusion, secondary choroidal neovascularization and RPE atrophy[5]. It was then proposed that PDT parameters could be modified in half-dose or half-fluence PDT to improve safety while maintaining its therapeutic effectiveness[7].Intravitreal VEGF is the other treatment option for chronic CSC, owing to its anti-permeability properties[8-10]. The safety and efficacy of intravitreal bevacizumab and PDT has been studied and compared in several studies. Varying conclusions have been drawn. Semeraroet al[11]indicated no significant difference in the therapeutic effect between the two over a 9-month follow-up period. Baeet al[12], on the other hand,reported on an overall superiority in low-fluence PDT. Unlike monoclonal antibodies, conbercept is a recombinant protein which composed of VEGF receptor-1 and receptor-2 with the Fc segment of human immunoglobulin G1. It has been demonstrated effective in treating wet age-related macular degeneration, choroidal neovascularization and macular edema but not fully investigated in CSC[13]. The preliminary results in our prior research has shown potential therapeutic effects of conbercept in treating chronic CSC[14]. This study aimed to explore the safety and efficacy of conbercept in treating chronic CSC with the comparison to half-dose PDT in a period of 6mo.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted following the principles of the Declaration of Helsinki and got approval by the Ethics Committee at the Eye Hospital of Wenzhou Medical University (No.2019-030-K-29). Informed consent was obtained from all subjects.
SubjectsThe clinical data of chronic CSC patients who received intravitreal conbercept and half-dose PDT from January 2015 to August 2018 was retrospectively reviewed and enrolled following the criteria measures. Inclusion criteria included: 1) Male or non-pregnant women aged over 18;2) Presence of symptoms for longer than 6mo; 3) Presence of subfoveal SRF on optical coherence tomography (OCT;Spectralis, Heidelberg, Germany); 4) Presence of characteristics of chronic CSC on fundus fluorescein angiography (FFA) and indocyanine green angiography (ICGA): diffuse fluorescent leakage with dilation of the choriocapillaris; 5) Follow-up for at least 6mo post treatment. Exclusion criteria included presence of: 1) Detection of choroidal neovascularization at first or follow-up visit by FFA and ICGA; 2) Other concomitant diseases like age-related macular degeneration, polypoidal choroidal vasculopathy or serious systemic disease; 3) History of interventional treatment such as usage of other anti-VEGF agent, laser photocoagulation or ocular surgery; 4) Previous treatment of steroid before the onset of symptoms. If chronic CSC patients meet these criteria with binocular involvement,the eye with poorer vision was selected in this study.
TreatmentSubjects were grouped based on the treatment methods. In the half-dose PDT group, patients were treated with half-dose verteporfin infusion (3 mg/m2) over 10min following light application with a dose of 50 J/cm2(83s) on hyper-permeable lesion captured on FFA and ICGA with an extra 500 µm in diameter. In the conbercept group, 0.5 mg/0.05 mL of conbercept was injected into the vitreous cavity in a sterile operation room. This group was treated following the “1+pro re nata(1+PRN)” treatment regimens. Thus, reinjection could be administered as needed after initially injection. Reinjection of conbercept was performed based on the following criteria:1) best-corrected visual acuity (BCVA) loss of 0.2 logarithm of the minimum angle of resolution (logMAR) or more; 2)persistence of SRF one month after the last injection[12,15]. And half-dose PDT was not repeated within six months considering its action time. If SRF persisted six months after the initial treatment, or signs of aggravation were present, the opposite treatment modality can be applied for ethical considerations.That is, half-dose PDT was available for the conbercept group,conbercept injection for the half-dose PDT group.
Outcome Measures and Follow-up VisitsAt each visit, a comprehensive ocular exam was conducted which included visual acuity testing, refraction, anterior segment examination,intraocular pressure measurements, dilated fundus exam,enhanced depth imaging-OCT (EDI-OCT). The patients were followed up at 2wk, 1, 2, 3 and 6mo after treatment, and then every 3 to 6mo once the condition has become stable. Any ocular or systemic complications were documented. Changes in BCVA, central macular thickness (CMT), SFCT and SRF were collected and analyzed. The BCVA was expressed in the mean logMAR. CMT was measured from the RPE to the inner limiting membrane (ILM). SFCT was measured from the RPE to the inner surface of sclera at the fovea. All measurements represented the average of three replicates completed by a trained ophthalmologist (Mao JB).
Statistical AnalysisStatistical analysis were carried out using SPSS Statistics software version 19.0 (SPSS, Inc., Chicago,IL, USA). Continuous data were described by means±standard deviations. The comparison of outcome measures was conducted by repeated measures analysis of variance.Categorical variables were analyzed with Chi-squared test,and continuous variables were compared by independent samplet-test and one-way analysis of variance. AP<0.05 was considered statistically significant.
RESULTS
Ninety-four eyes in ninety-four patients with chronic CSC met the inclusion criteria. Thirty-seven patients (37 eyes)received conbercept intravitreal injection and another fiftyseven patients (57 eyes) received half-dose PDT. In addition,thirty-five healthy individuals (35 eyes) with matched age and sex were included as normal control group. The general demographics and clinical characteristics were summarized in Table 1. The mean number of required conbercept injections was 1.78±0.75 (range, 1-4) in 6mo. There was no statisticaldifference in age, gender, duration of symptoms, BCVA, CMT and SFCT at baseline between the two treatment groups (allP>0.05). And neither the conbercept group nor half-dose PDT group received ophthalmological treatments previously. There was statistical significance in CMT and SFCT between normal control group and two treatment groups.

Table 1 Baseline demographic and clinical characteristics
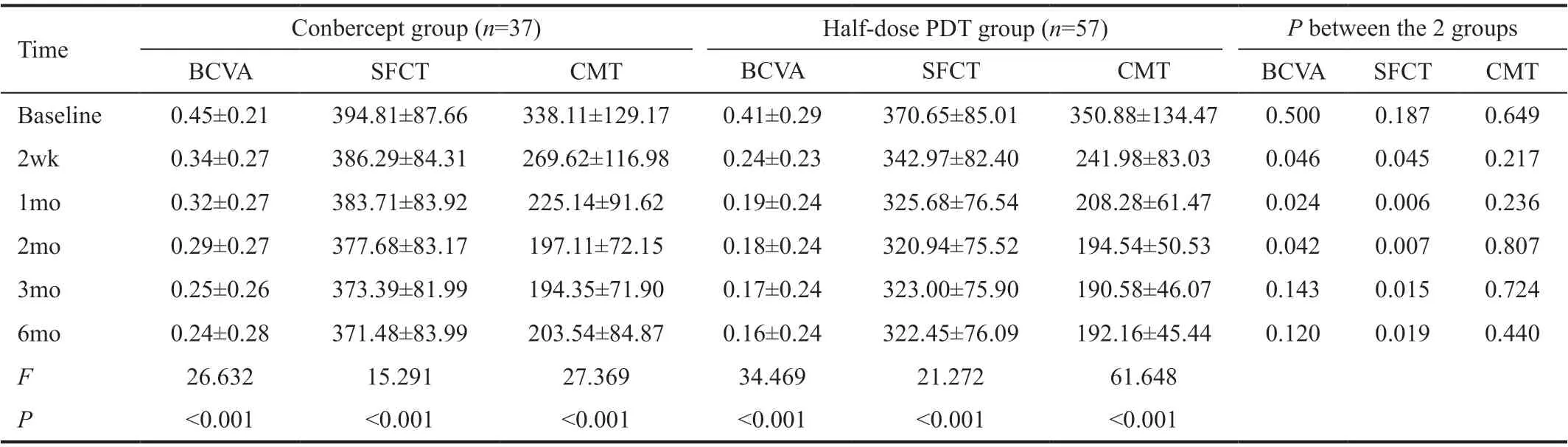
Table 2 Changes of BCVA, CMT and SFCT in the two treatment groups mean±SD, μm
SafetyThere were no severe ocular or systemic complications during the study period. Mild visual and ocular complications may be present, such as blurriness, conjunctival injection and superficial punctate keratitis. But all were temporary and recovered soon after procedures.
Best-Corrected Visual AcuityFigure 1 and Table 2 show results of BCVA in logMAR. Compared to baseline, the mean logMAR BCVA improved significantly in both groups at each follow-up (F=26.632,P<0.001 in the conbercept group andF=34.469,P<0.001 in the half-dose PDT group). BCVA of the half-dose PDT group was significantly better at 2wk, 1 and 2mo (t=2.02, 2.29, and 2.07, respectively;P=0.046, 0.024 and 0.042, respectively). At 3 and 6mo, the BCVA had no significant difference between the two groups (t=1.48 and 1.62,respectively;P=0.143 and 0.120 respectively).
Subfoveal Choroidal ThicknessThe mean SFCT in the conbercept group and half-dose PDT group was shown in Table 2. The difference was statistically significant before and after treatment in both groups (F=15.291,P<0.001 in the conbercept group;F=21.272,P<0.001 in the half-dose PDT group). Compared to the normal control group, the choroidal thickness was thicker in the two treatment despite change after treatment as displayed in Figure 2. As shown in Figure 3, the half-dose PDT group had significant better outcome compared to the conbercept group at any follow-up period (t=2.05, 2.85,2.81, 2.51, and 2.41, respectively;P=0.045, 0.006, 0.007,0.015, and 0.019, respectively).
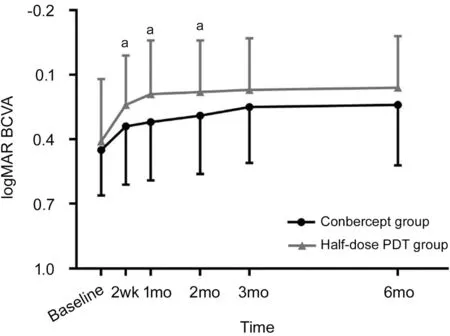
Figure 1 logMAR BCVA aStatistically significant difference between the groups.
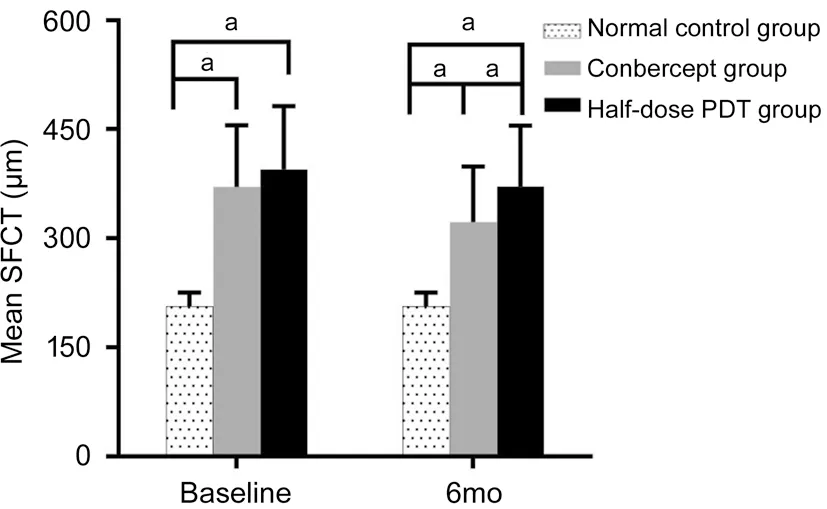
Figure 2 Mean SFCT before and after treatment aStatistically significant difference between the groups.

Figure 3 SFCT: conbercept vs half-dose PDT A: SFCT change from baseline in the two groups at each visit; B: SFCT reduction in the two groups at each visit. aStatistically significant difference between the groups.
Central Macular ThicknessTable 2 shows results of the mean CMT in the two treatment groups. In the conbercept group, CMT reduction was 68.49±70.77, 112.97±115.92,141.00±121.57, 143.76±125.10, and 134.57±135.88 μm at 2wk, 1, 2, 3 and 6mo after initial treatment. In the halfdose PDT group, CMT reduction was 108.89±105.98,144.42±131.67, 156.86±132.93, 160.82±135.75, and 159.16±134.23 μm at 2wk, 1, 2, 3, and 6mo.As shown in Figure 4, compared to the normal control group, the CMT in the two treatment groups were both significantly higher at baseline and reduced significantly at each follow-up. At 6mo after initial treatment, there was no statistical difference among the three groups. Between the two treatment groups, the mean CMT did not significantly differ at any follow-up period (t=1.25, 1.19, 0.25, 0.36, and 0.78, respectively;P=0.217, 0.236, 0.807, 0.724, and 0.440,respectively; Figure 5A). The CMT reduction was greater in the half-dose PDT group although the difference was only statistically significant at the 2-week follow-up (t=2.22, 1.19,0.58, 0.61 and 0.86, respectively;P=0.029, 0.239, 0.561,0.541, and 0.390, respectively; Figure 5B).
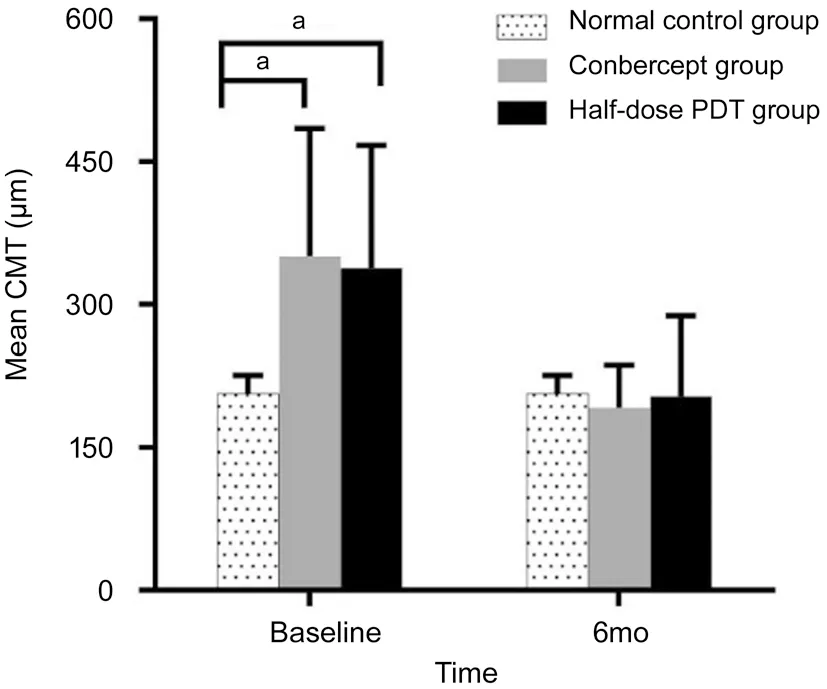
Figure 4 Mean CMT before and after treatment aStatistically significant difference between the groups.

Figure 5 CMT: conbercept vs half-dose PDT A: CMT change from baseline in the two groups at each visit; B: CMT reduction in the two groups at each visit. aStatistically significant difference between the groups.
Subretinal FluidIn the conbercept group, full resolution of SRF was achieved in 10.8% (4/37) eyes at 2wk, 29.7% (11/37)eyes at 1mo, 54.1% (20/37) eyes at 2mo, 67.6% (25/37) eyes at 3mo and 70.3% (26/37) eyes at 6mo. In the half-dose PDT group, full resolution of SRF was achieved in 33.3% (19/57)eyes at 2wk, 59.6% (34/57) eyes at 1mo, 78.9% (45/57)eyes at 2mo, 87.7% (50/57) eyes at 3mo and 94.7% (54/57)eyes at 6mo. Overall, the half-dose PDT group had more complete resolution than the conbercept group at each followup (χ2=6.158, 8.048, 6.517, 5.650, and 5.224, respectively;P=0.013, 0.005, 0.011, 0.017, and 0.022, respectively).Comparing Figures 5B and 6, it can be seen that the change in SRF resembled that in CMT (t=2.51, 1.86, 0.89, 0.79, and 1.14, respectively;P=0.014, 0.066, 0.377, 0.432, and 0.257,respectively).
DISCUSSION
To date, the exact pathogenesis of CSC has not been well identified. The clinical treatment strategy is still to be unified.Several plausible assumptions have been proposed, including choroidal hyper-permeability, congestion of choroidal vessels,increased choroidal thickness, and impairment of the barrier effect of RPE which leads to accumulation of fluid under the retina[1-2]. A number of studies have shown the effect of halfdose PDT and other anti-VEGF agents such as bevacizumab or ranibizumab in treating chronic CSC[4-12,16]. The therapeutic effectiveness of intravitreal injection of conbercept, especially in comparison to PDT, is yet unclear.
In this study, both treatment methods were safe and can be efficacious in the treatment of chronic CSC with slight difference. The success rate of conbercept and half-dose PDT at the end of 6-month follow-up was 70.3% and 94.7%, which was consistent with those ranging from 40% to 80% and 83% to 100% reported in the previous studies[4-12]. Our study found more complete SRF resolution achieved with the halfdose PDT and an overall more rapid anatomic restoration and clinical healing.
While both methods are effective in vision improvement, visual acuity recovery was faster with the half-dose PDT during the first 2mo. The vision recovery rate and degree were similar in the two groups in later stage. The potential explanation for this is the faster SRF absorption with PDT, given that SRF is one of the primary reasons for vision loss in CSC[17-18]. Similarly, Baeet al[12]observed a faster improvement in visual acuity with low-fluence PDT in comparison to ranibizumab within the first 3mo with following sustained superiority without a significant difference. On the contrast, Semeraroet al[11]reported similar results between intravitreal bevacizumab injection and lowfluence PDT after 9mo of follow-up, however without a comparison during early phase.

Figure 6 SRF reduction in the two groups at each visit aStatistically significant difference between the groups.
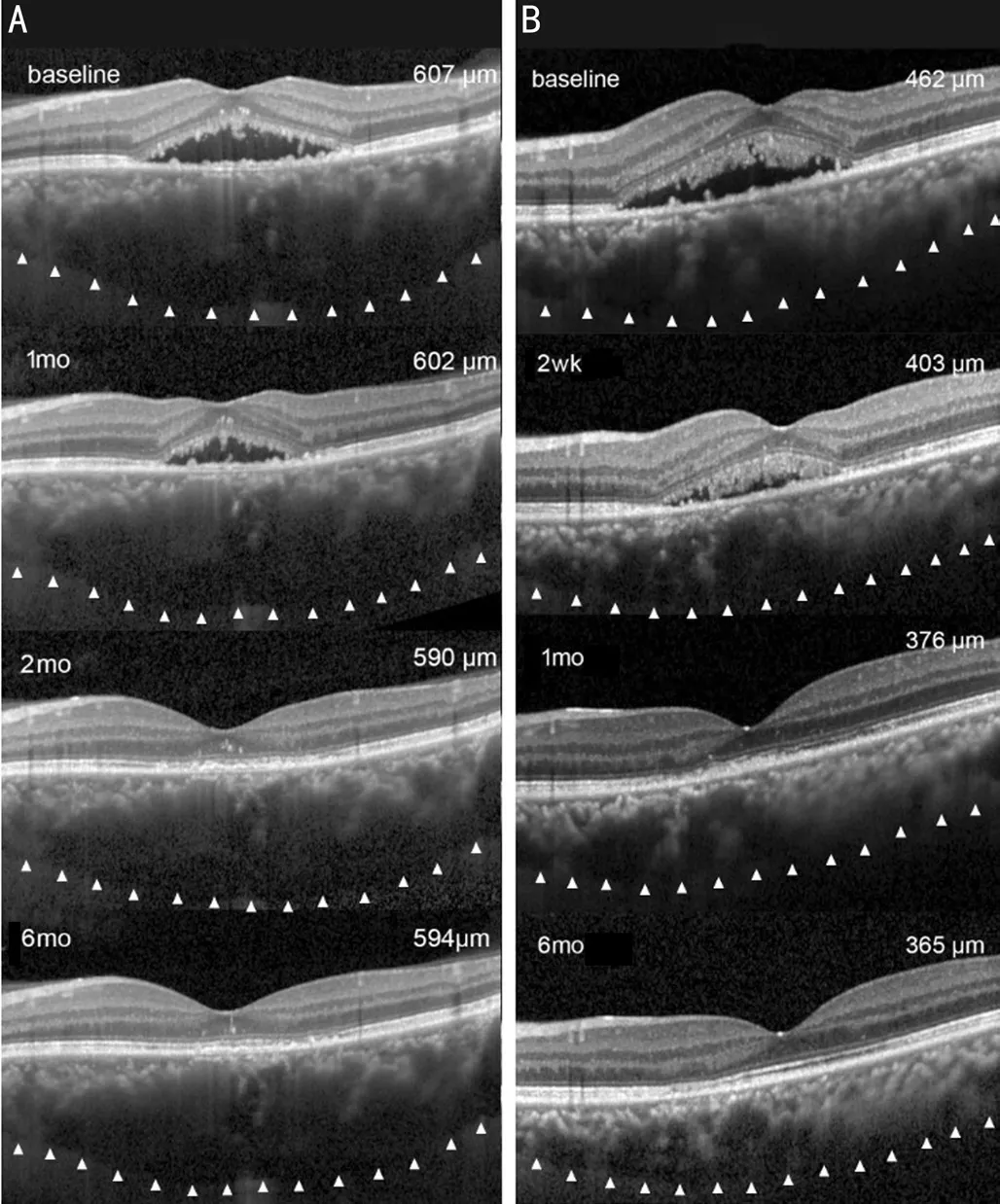
Figure 7 SFCT changes after treatment A: A 54-year-old female patient with chronic CSC in the left eye underwent intravitreal injections of conbercept. The SFCT was 607 μm at baseline, 602 μm at 1mo, 590 μm at 2mo and 594 μm at 6mo. B: A 40-year-old male patient with chronic CSC in the left eye underwent half-dose PDT.The SFCT was 462 μm at baseline, reduced to 403 μm at 2wk, 376 μm at 1mo and 365 μm at 6mo.
It is important to note that the choroidal thickness after both treatments was still thicker than that of the normal eyes.Typical examples were shown in Figure 7. It has been reported that the choroidal thickness was positively correlated with the choroidal vascular hyper-permeability, which can be a potential reason for the recurrence of CSC[18-20]. Thus, the choroidal thickness after treatment may be an indicator to the future recurrence of CSC[21]. While there was no significant difference between the intravitreal bevacizumab group and half-fluence PDT group in one study above, our study found that half-dose PDT led to a greater degree of reduction in choroidal thickness.The reason may be due to the differences in population and PDT parameters. Different from the half-fluence PDT, the half-dose PDT may induce a faster SRF reabsorption and a longer-lasting effect[7]. In our study, there was no statistically significant difference in the recurrence rate between the two groups. Only 2 eyes (5.4%) in the conbercept group and 1 eye (1.8%) in the half-dose group suffered a relapse after complete resolution of SRF. This is likely due to the short follow-up period. A longer follow-up period is necessary to fully investigate the correlation between recurrence rate and treatment modalities.This study was retrospective and has its limitation in a small sample size, a relatively short follow-up period and lack of randomization. The short follow-up has an effect on recurrence rate and complication analysis between study arms. Further prospective studies with a large sample and a longer study period are expected to confirm the comparison results between the two treatment methods.
In conclusion, our study demonstrated that both conbercept intravitreal injection and half-dose PDT can improve visual acuity and macular structure in chronic CSC patients. While the therapeutic effect of half-dose PDT was superior at initial phase of treatment, it was indicated that both therapeutic approaches can be safe, effective and feasible in treating chronic CSC.
ACKNOWLEDGEMENTS
Foundations:Supported by Wenzhou Municipal Science and Technology Bureau (No.Y20180728); Wenzhou Municipal Science and Technology Bureau (No.Y20190635); Wenzhou Municipal Science and Technology Bureau (No.2019Y0592).
Conflicts of Interest: Mao JB,None;Zhang CY,None;Liu CY,None;Zhang Y,None;Lin JJ,None;Xu ZK,None;Chen YQ,None;Fan YY,None;Zhao SX,None;Shen LJ,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Protective effects of upregulated HO-1 gene against the apoptosis of human retinal pigment epithelial cells in vitro
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
