Via pars plana anterior iris enclavation lOL fixation
Tomaso Caporossi, Ruggero Tartaro, Giancarlo Albani, Francesco Barca, Fabrizio Giansanti,Stanislao Rizzo,2
1Department of Surgical and Translational Medicine,Eye Clinic, University of Florence, Azienda Ospedaliera Universitaria Careggi, Florence 50139, Italy
2Department of Ophthalmology, Catholic University of Sacred-Heart Foundation “Policlinico Universitario A. Gemelli”IRCCS, Rome 00168, Italy
Abstract
● KEYWORDS: IOL luxation; via pars plana vitrectomy;cystoid macular edema; iris enclavation IOL
INTRODUCTION
Aphakia, with a non-sufficient capsular support may be spontaneous, the consequence of complicated cataract surgery, trauma or pseudoexfoliation syndrome[1]. Many techniques for intraocular lens (IOL) secondary implant have been described[2-5]. Iris claw IOLs are useful in the case of aphakia although in vitrectomised eyes their positioning is challenging because of the lack of vitreous support during the enclavation. Sometimes even the most experienced surgeons struggle to fix these IOLs using anterior chamber manoeuvres,in vitrectomised eyes. In this article we describe a usefulviapars plana anterior chamber iris enclavation IOL fixation technique that can be used in vitrectomised eyes as the first choice or in the case of unsuccessful implant.
SUBJECTS AND METHODS
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the local Ethic Committee and with the Declaration of Helsinki. Informed consent was obtained from all subjects.
The procedures were performed both under local (30 cases)and general anaesthesia (5 cases). The 25-gauge pars plana vitrectomy (PPV; Alcon surgical Inc., USA) 3 ports set was mounted, and the retina was examined. Additional vitreous shaving was carried out if needed. A sclero-corneal 5.5 mm tunnel was performed (2-3 mm from the limbus) using a 30°blade for the scleral pre-cut, crescent blade to perform the scleral tunnel and a 5.4 blade to enter the anterior chamber.The iris claw lens was introduced through the scleral tunnel.Once the IOL plate was stabilised using the iris claw forceps,a 30-gauge needle was bent 45 degrees, inserted through the pars plana at 3.5 mm from the limbus, at 3 and 9 o’clock,and directed anteriorly towards the claw to trap the iris into it(Figure 1). The same procedure was repeated for the opposite claw. Basic salt solution (BSS) was left in the vitreous chamber. Vicryl 7/0 (Ethicon, USA) was used to suture the sclerotomies. No suture was applied to the scleral tunnel. The conjunctiva was repositioned over the scleral incision and fixated using diathermy (Video 1, online supplementary).
RESULTS
Thirty-five eyes of 35 consecutive patients were included in this retrospective non-comparative consecutive case series study (Table 1).
Mean age was 71.12±10.12y. The mean follow-up was 6.4mo. The mean preoperative best corrected visual acuity(BCVA) was 0.11±0.14 logMAR, the mean postoperative BCVA was 0.07±0.11 logMAR. The preoperative mean spherical equivalent was 7.22 D. The final mean spherical PXF: Pseudoexfoliation; SD: Standard deviation; IOP: Intraocular pressure; EC: Endotelial count.equivalent was -0.25±0.15 D (Table 2). None of the eyes had endophthalmitis, hypotony, retinal or choroidal detachment.
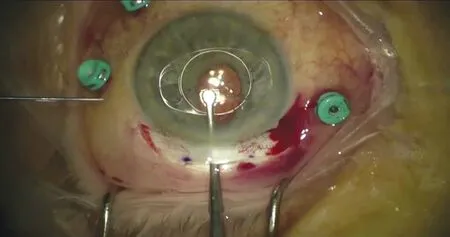
Figure 1 Once the IOL plate was stabilised using the iris claw forceps, a 30-gauge needle was inserted through the pars plana, at 3 and 9 o’clock, and directed anteriorly towards the claw to trap the iris on it.

Table 1 Preoperative findings n (%)
DISCUSSION
In this retrospective study, we have included cases of aphakia or luxated IOLs where we performed aviapars plana anterior iris enclavation IOL implant.
In this paper we were not focused on the postoperative refractive results, which have already been discussed and confirmed by many authors. Our aim is to validate the effectiveness of this surgical technique that is performed using fast and safe intraoperative maneuvers and showed a low incidence postoperative complication.
A conventional agreement on the gold standard to correct aphakia in absence a capsule support has not been postulated[1]. Currently, the main possibilities for secondary IOL implantation are: trans-scleral sutured posterior chamber IOLs[6], angle-supported anterior chamber IOLs[4], iris-fixated IOLs introducedviascleral tunnel[5,7], and the flanged IOL operation by Yamaneet al[8].
Nevertheless, iris-fixated IOLs are popular because they produce a quicker and better BCVA increase. In addition, the surgical time is relatively shorter[9]and some studies reported low complication rates with iris-fixated IOLs[10-11].
The drawbacks of both antero-pupillary or retro-pupillary iris claw IOL’s are that they need a 5.5 large incision which results in postoperative astigmatism.
We did not have significant complications and the patients had a positive refractive outcome with low residual astigmatism.Similarly to these group of authors[7], we performed a scleral self-sealing incision. Contrarily, Touriño Peralbaet al[12]and Toroet al[5]preferred a wide limbal corneal incision sutured with 10-0 nylon to manage postoperative astigmatism.
This technique is relatively easy and repeatable, and it is our first choice in the case of anterior iris enclavation IOL’s.
This group of authors[1]showed an iris-claw IOL postoperative subluxation in 6% of the patients. They argued that this was due to the not-flexible claws that characterised the previous versions of iris-fixated IOL’s models.
Toroet al[5]observed a dislocation in 2 patients (one patient had an anterior-fixated iris-claw IOL and one patient had a posterior-fixated iris-claw IOL.)
In our series we reported only one case of postoperative IOL dislocation (2.8% of the cases).
Using our technique, excessive iris manipulation is avoided and therefore it may be possible to reduce pigmentary dispersion and intraocular inflammation. However, because of the manipulation through the pars plana, it may theoretically induce intra-operative bleeding, that was not observed in our casuistry. Conversely, Toroet al[5]reported 5 cases of hyphema after iris-claw fixation.
In addition, we did not find and any endothelial decompensation which could complicate an anterior iris enclavation IOL implant in the postoperative follow up.
There are two main factors for endothelial cell loss after irisclaws IOL’s implantation[13]: a reduced anterior chamber and a small space between the central and peripheral IOL margin to the posterior corneal face. According to these findings we performed a complete vitrectomy to deepen the anterior chamber. Baykaraet al[7]suggested that implanting an iris claw IOLviaa scleral tunnel causes refuced endothelial loss thanviaa clear corneal tunnel. However, Toroet al[5]performing a corneal incision, did not reported any corneal decompensation or endothelial cell loss.
Another possible complication is the cystoid macular edema(CME) which, in our casuistry affected only two patients(5.7%), one had a complicated cataract operation, and one is a diabetic patient, although it was resolved after two months of non-steroidal anti-inflammatory drops (NSAID) in both cases.Our postoperative CME rate is similar with the one (range 4.1%-4.8%) presented in other studies with iris-claw IOLs inserting[14-15]. A retinal detachment risk (range 6.3%-8.2%)and a choroidal bleeding chance of 3.2% after the insertion of a scleral-sutured posterior chamber IOLs were presented by these group of authors[16-17].
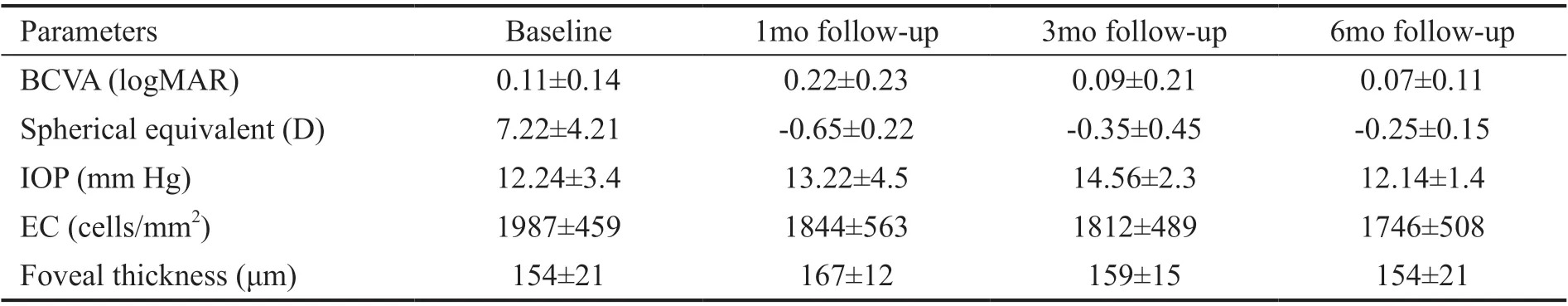
Table 2 The postoperative outcomes mean±SD
We did not report any retinal detachment complication in our case series. The accurate vitreous base shaving performed in all the cases may avoided retinal complications.
Occasionally, even the most experienced surgeons struggle to fix an anterior iris enclavation IOLviathe anterior chamber.Therefore, our technique could be also used in the case where the anterior chamber enclavation is not successful, even though it has become our first approach. The disadvantage of this technique is that the retinal periphery should be checked after the IOL enclavation, though in our casuistry we did not find any bleeding or iatrogenic tears.
In conclusion, thisviapars plana anterior chamber iris enclavation IOL fixation technique could be useful in the case of unsuccessful anterior chamber enclavation. In addition,it could be used successfully as the first choice because it is quick, repeatable, and reduces iris manipulation.
ACKNOWLEDGEMENTS
Conflicts of Interest:Caporossi T,None;Tartaro R,None;Albani G,None;Barca F,None;Giansanti F,None;Rizzo S,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
- lris manipulation during phacoemulsification: intraoperative and postoperative complications
