Better Than You Think—Appropriate Use of Implantable Cardioverter-Def ibrillators at a Single Academic Center:A Retrospective Review
Nikhil H.Shah,MD,Steven J.Ross,MD,Steve A.Noutong Njapo,MD,Justin Merritt,MD,A ndrew Kolarich,MD,Michael Kaufmann,MD,William M.Miles,MD,David E.Winchester,MD,Thomas A.Burkart,MD and Matthew McKillop,MD
1 UF Division of Cardiovascular Medicine,1600 SW Archer Rd,PO Box 100277,Gainesville,FL 32610,USA
2 UVA Division of Cardiovascular Medicine,PO Box 800158 1215 Lee St.Charlottesville,VA 22908-0158,USA
3 The Johns Hopkins Hospital Department of Radiology,601 N Caroline St,Baltimore,MD 21287,USA
4 The Heart Center,930 Franklin Street SE,Huntsville,AL,358015,USA
5 Intermountain Medical Center,1380 E Medical Center Dr,Ste 1500,St.George,UT 847906,USA
6 Carolina Cardiology Consultants,Prisma Health,1005 Grove Road,Greenville,SC 29605,USA
Abstract Background:Implantable cardioverter-def brillators (ICDs) can be life-saving devices,although they are expensive and may cause complications.In 2013,several professional societies published joint appropriate use criteria (AUC)assessing indications for ICD implantation.Data evaluating the clinical application of AUC are limited.Previous registry-based studies estimated that 22.5% of primary prevention ICD implantations were “ non-evidence-based” implantations.On the basis of AUC,we aimed to determine the prevalence of “ rarely appropriate ” ICD implantation at our institution for comparison with previous estimates.Methods:We reviewed 286 patients who underwent ICD implantation between 2013 and 2016.Appropriateness of each ICD implantation was assessed by independent review and rated on the basis of AUC.Results:Of 286 ICD implantations,two independent reviewers found that 89.5% and 89.2%,respectively,were appropriate,5.6% and 7.3% may be appropriate,and 1.8% and 2.1% were rarely appropriate.No AUC indication was found for 3.5% and 3.4% of ICD implantations,respectively.Secondary prevention ICD implantations were more likely rarely appropriate (2.6% vs.1.2% and 3.6% vs.1.1%) or unrated (6.0% vs.1.2% and 2.7% vs.0.6%).T he reviewers found 3.5% and 3.4% of ICD implantations,respectively,were non-evidence-based implantations.The difference in rates between reviewers was not statistically signif cant.Conclusion: Compared with prior reports,our prevalence of rarely appropriate ICD implantation was very low.The high appropriate use rate could be explained by the fact thaAt UC are based on current clinical practice.T he AUC could benef t from additional secondary prevention indications.Most importantly,clinical judgement and individualized care should determine which patients receive ICDs irrespective of guidelines or criteria.
Keywords:Appropriate use;appropriate use criteria;implantable cardioverter-def brillator
Background
Implantable cardioverter-def brillators (ICDs) can be life-saving devices.They can be implanted in patients who have experienced sudden cardiac death or those who may be at elevated risk of sudden cardiac death.Despite their life-saving potential,they are expensive and carry the risk of serious complications,such as pneumothorax,lead displacement,infection,and inappropriate device therapies [1].
In 2013,the American College of Cardiology,the Heart Rhythm Society,and the American Heart Association published joint appropriate use criteria(AUC) outlining clinical scenarios in which ICDs are indicated.The criteria were decided upon by an expert panel who rated clinical scenarios on a scale from 1 to 9 as rarely appropriate (1–3),may be appropriate (4–6),and appropriate (7–9).Clinical scenarios are assigned an appropriateness score(from 1 to 9),which was determined by a consensus of the AUC authors [2].
Prior investigators have discussed that certain clinical scenarios in the AUC are not currently covered by the Medicare national coverage deter -mination.Consequently,submitting such ICDs for reimbursement may be construed as fraudulent despite their being clinically indicated and appropriate [3].The inability to receive indicated ICD implantation due to coverage and funding discrepancies could be the difference between life and death.
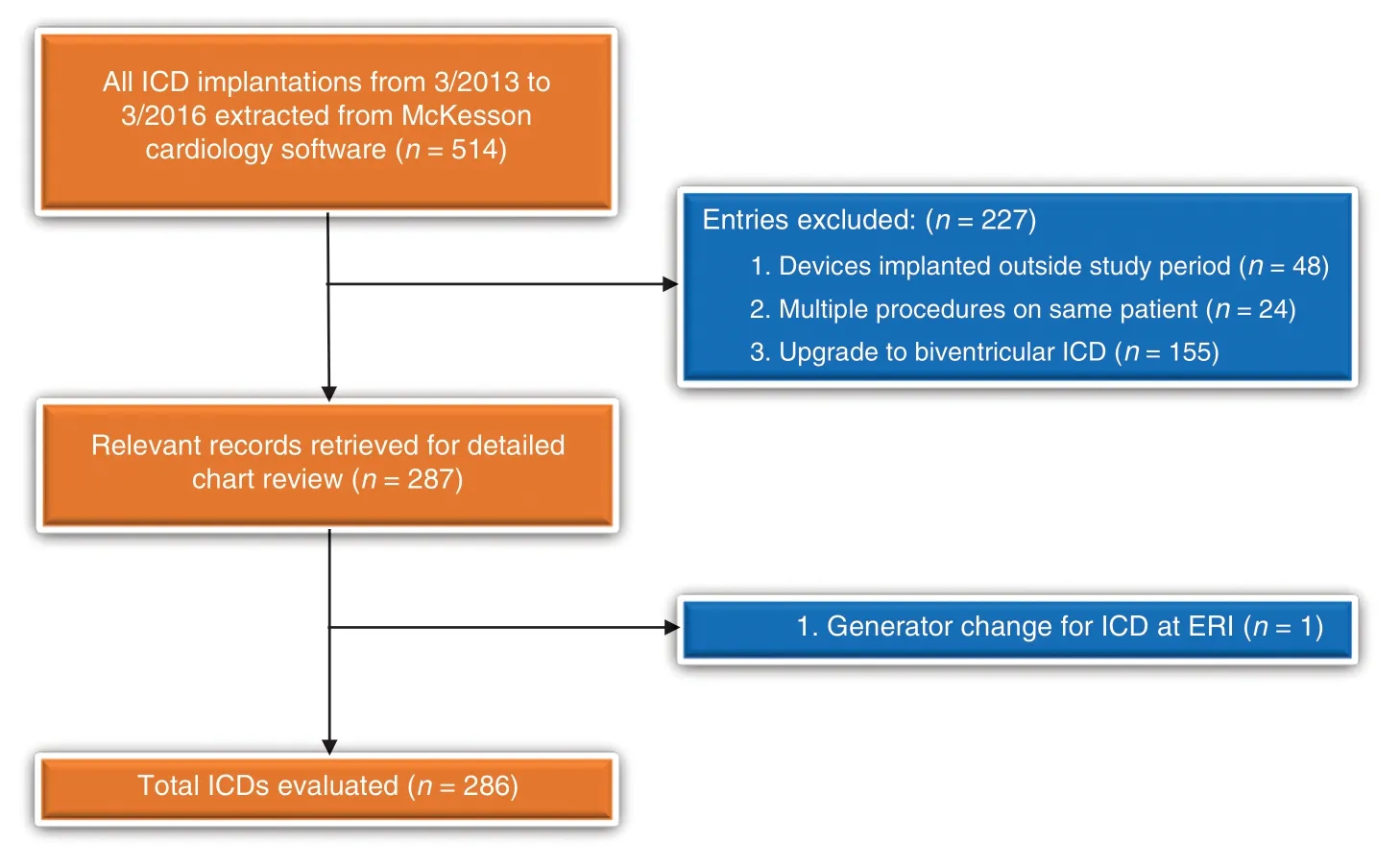
Figure1:Search and Exclusion Criteria.
Previous registry-based studies used various criteria to assess appropriateness of ICD implantation.One study found that 22.5% of primary prevention ICD implantations were non-evidence-based implantations if they met any of four criteria:New York Heart Association class IV symptoms,myocardial infarction within 40 days,revascularization within 3 months,or newly diagnosed heart failure at the time of implantation [4].A later study found that 86% of all primary prevention ICD implantations met the inclusion criteria of major ICD trials [5].Generally,although the criteria were published in 2013,clinical data evaluating the real-world application of AUC are sparse.
We aimed to determine the prevalence of AUCdeemed rarely appropriate ICD implantation at our facility and then compare these data with previously published estimates,such as those by Al-Khatib et al.[4] and Kaiser et al.[5].We hypothesized that we would have a high rate of appropriate ICD implantations,with very few rarely appropriate ICD implantations.Furthermore,as reimbursement is often based on clinical guidelines,we aimed to assess the validity of the AUC should these be a determination of reimbursement in the future.
Methods
We performed an Institutional Review Board–approved retrospective medical record review of 286 patients (Figure1) at our institution.Patients were identif ed through the McKesson Cardiology system (McKesson Corporation,Las Colinas,TX,USA),which is used in the electrophysiology laboratory.Patients aged at least 18 years with single-chamber or dual-chamber ICDs implanted at our institution in the 3 years following publication of the AUC (March 2013 to March 2016) were evaluated.Patients who were identif ed as having biventricular ICD upgrades in the McKesson Cardiology system and those who only underwent generator change were excluded.Data collection was super -vised by a staf f electrophysiologist,and data were entered by several resident physicians and a medical student into an institutional research electronic data capture (REDCap) database [6].
Two physicians independently reviewed and assessed the appropriateness of all 286 ICD implantations on the basis of the AUC and were blinded to the other physician ’ s assessments.Deidentif ed data were exported into an Excel spreadsheet,and were then sorted by indication and appropriateness of each ICD implantation for tallying.
Statistical analysis was performed by a chi-square analysis to compare the appropriateness rates by each reviewer.
Results
Baseline demographics are reported in Table1.The patient population included approximately 70%males with a mean age of 58 years.Seventy per -cent were white,2.8% had a myocardial infarction within 40 days,72% had heart failure at implantation,and the average ejection fraction was 31%.Most patients had NewY ork Heart Association class I symptoms (26%) or class II symptoms (34%).The indications for which ICDs were implanted are listed in Table2.
The reviewers (reviewer 1 and reviewer 2,respectively) determined that 89.5% (n=2 56) and 89.2% (n=255) of implantations were appropriate,5.6% (n=1 6) and 7.3% (n=2 1) may be appropriate,and 1.8% (n=5) and 2.1% (n=6) were rarely appropriate.For the remaining 3.2% (n=9) and 1.4% (n=4),respectively,there was no ICD indication listed in the AUC (Figure2,Table3) (P=0.44 by chi-square analysis for all comparisons).
Of the total 286 ICD implantations,the reviewers(reviewer 1 and reviewer 2,respectively) deemed 170 and 176 ICDs to be implanted for primaryprevention.They found that 89.4% (n=1 52) and 88.6% (n=88.6%) of implantations were appropriate,8.2% (n=1 4) and 9.7% (n=1 7) may be appropriate,1.2% (n=2) and 1.1% (n=2) were rarely appropriate.For 1.2% (n=2) and 0.6%(n=1) of ICD implantations,the reviewers were unable to f nd any ICD indication in the AUC document (Figure3,Table4).Per the criteria of Al-Khatib et al.[4]f or “ non-evidence-based ”IC D implantation,the reviewers found that only 3.5%(n=6) and 3.4% (n=6) were “ non-evidencedbased” i mplantations (P=0.90 by chi-square analysis for all comparisons).
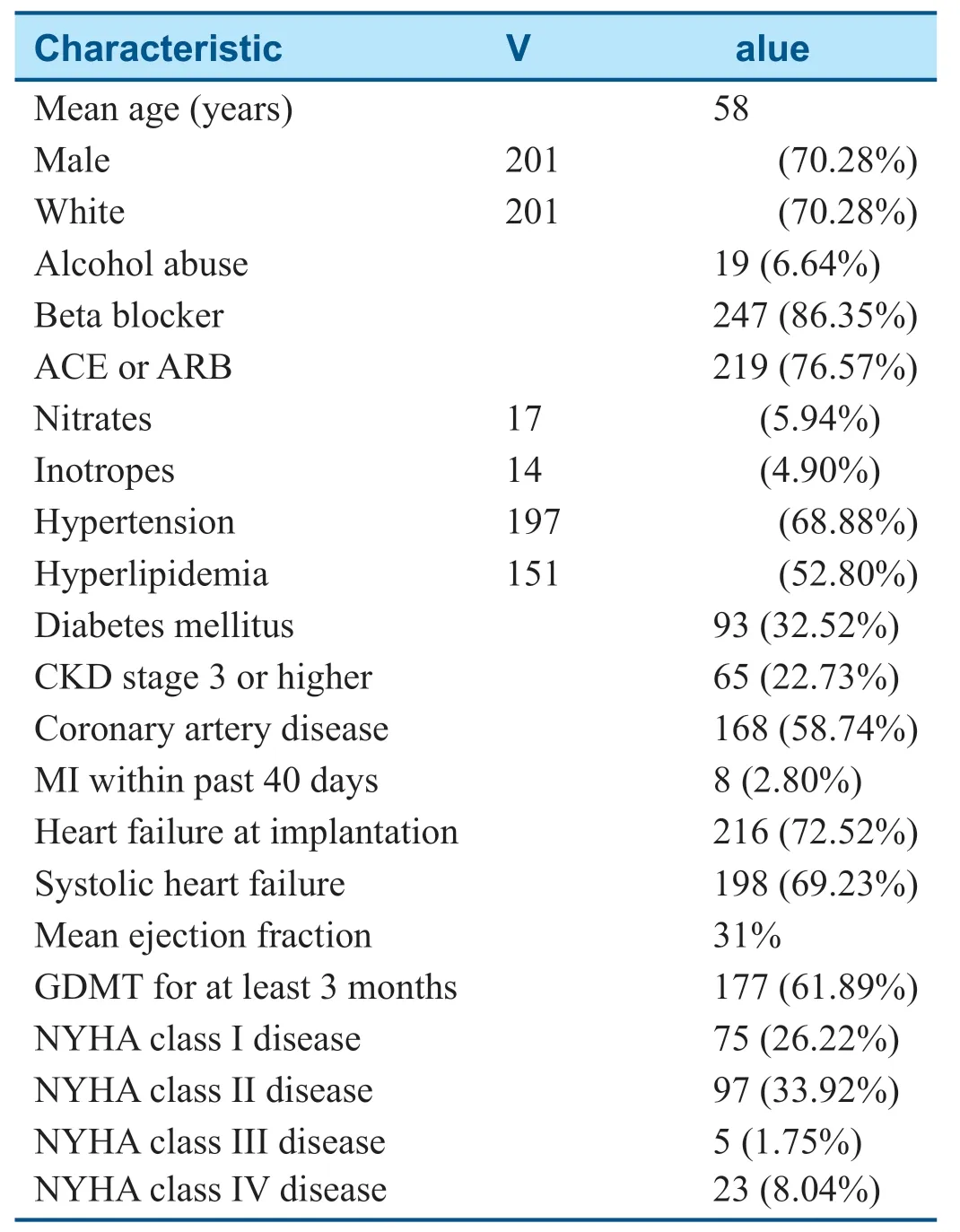
Table1 Baseline Characteristics of Patients.
The reviewers (reviewer 1 and reviewer 2,respectively) deemed 116 and 110 ICDs to be implanted for secondary prevention.They found 89.7%(n=1 04) and 90.0% (n=9 9) of implantations to be appropriate,1.7% (n=2) and 3.6% (n=4) may be appropriate,and 2.6% (n=3) and 3.6% (n=4)were rarely appropriate.Six percent (n=7) and 2.7% (n=3) had no listed indication in the AUC document (Figure4,Table5) (P=0.50 by chisquare analysis for all comparisons).
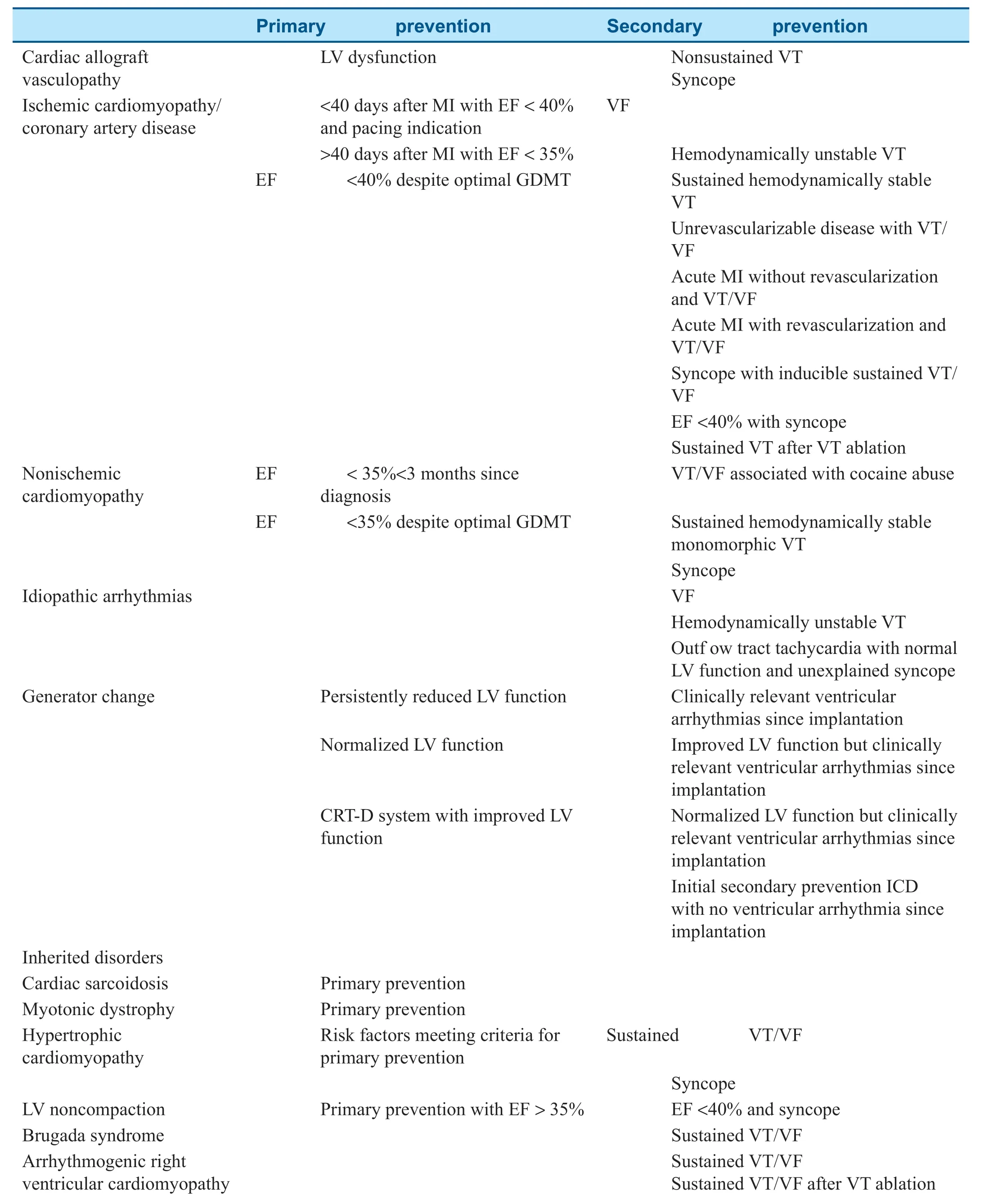
Table2 Implantable Cardioverter-Def brillator (ICD) Indications.
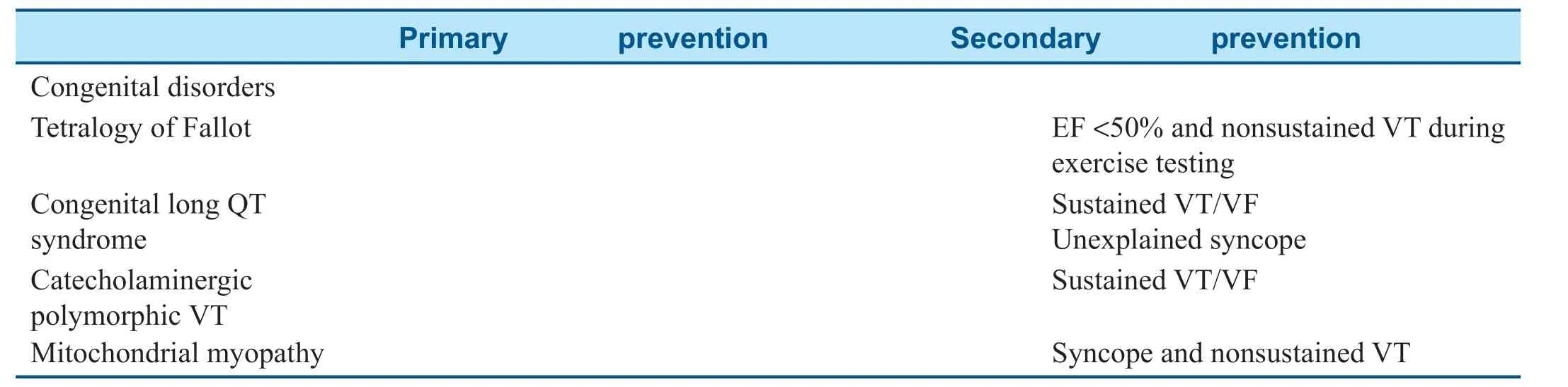
Table2(continued)
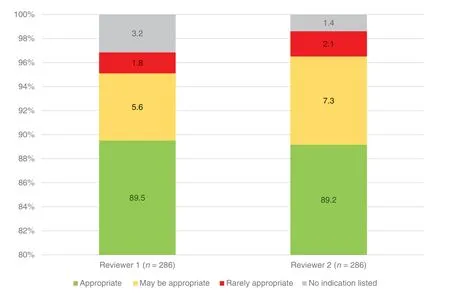
Figure2:Appropriateness of All Implantable Cardioverter-Def brillator Implantations (n=286).
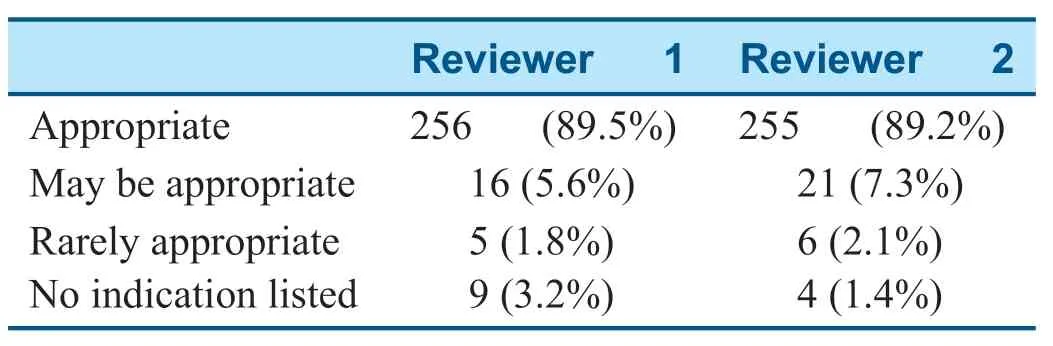
Table3 Appropriateness of All Implantable Cardioverter-Def brillator Implantations.
There was some interreviewer variability in appropriateness.In 5.24% of cases (n=15),the reviewers disagreed on the level of appropriateness of the ICD indication.In 2.80% of cases (n=8),one reviewer deemed an ICD implantation appropriate and the other deemed it rarely appropriate.
Discussion
There was a high proportion of appropriately implanted ICDs and a very low proportion of rarely appropriate ICD implantations for both primary and secondary prevention indications.Our high appropriate implantation rate suggests that the AUC accurately ref ect current clinical practice.
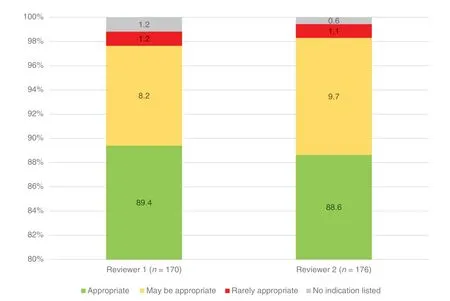
Figure3:Appropriateness of Primary Prevention Implantable Cardioverter-Def brillator Implantations.
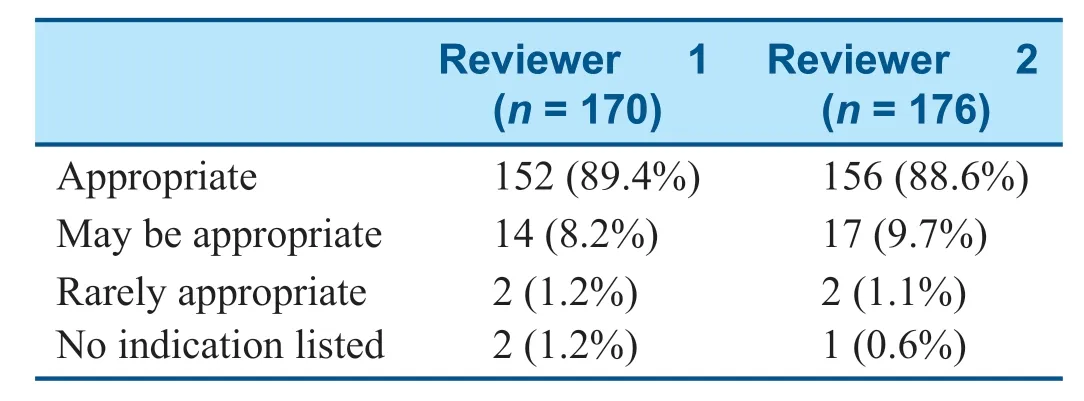
Table4 Appropriateness of Primary Prevention Implantable Cardioverter-Def brillator Implantations.
Comparing these data with data from prior studies (Table6),we found an average of 89.4% of ICD implantations in this study were appropriate compared with 86% from a study that assessed ICD implantation on the basis of major ICD trial inclusion criteria [5].Per the criteria of Al-Khatib et al.,only 3–4% of ICD implantations for primary prevention in our study were “ non-evidence-based”implantations compared with 22.5% in their study[4].One drastic difference is that the previous studies were registry analyses with more than 100,000 patients in all practice settings,compared with 286 patients in this study.Furthermore,all ICDs in our study were implanted by electrophysiologists in a university academic center,and thus the familiar -ity of the implanters with current evidence and guidelines likely contributed to the high appropriateness rate.
The low rarely appropriate implantation rate(1.2% and 1.1%) of primary preventions is likely due to clear primary prevention indications.Secondary prevention ICDs may have had a higher rate of rarely appropriate implantations (2.6% and 3.6%) as the AUC may not fully ref ect complex clinical scenarios often seen at university centers,such as patients with transplant vasculopathy,rare genetic disorders,or congenital heart disease.
The relatively high number of unrated secondary prevention implantations (6.0% and 2.7%)indicates that there are gaps in the AUC.Specif c examples include patients with hemodynamically unstable ventricular tachycardia without syncope in a structurally normal heart,as well as cardiac arrest in patients too unstable to undergo ischemic evaluation.In addition,the AUC do not address whether patients with a newly discovered cardiomyopathy who require permanent pacing should also receive an ICD at the time of device implantation,although for these clinical scenarios most clinicians would likely consider ICD implantation as the benef t likely outweighs the risk in this circumstance.
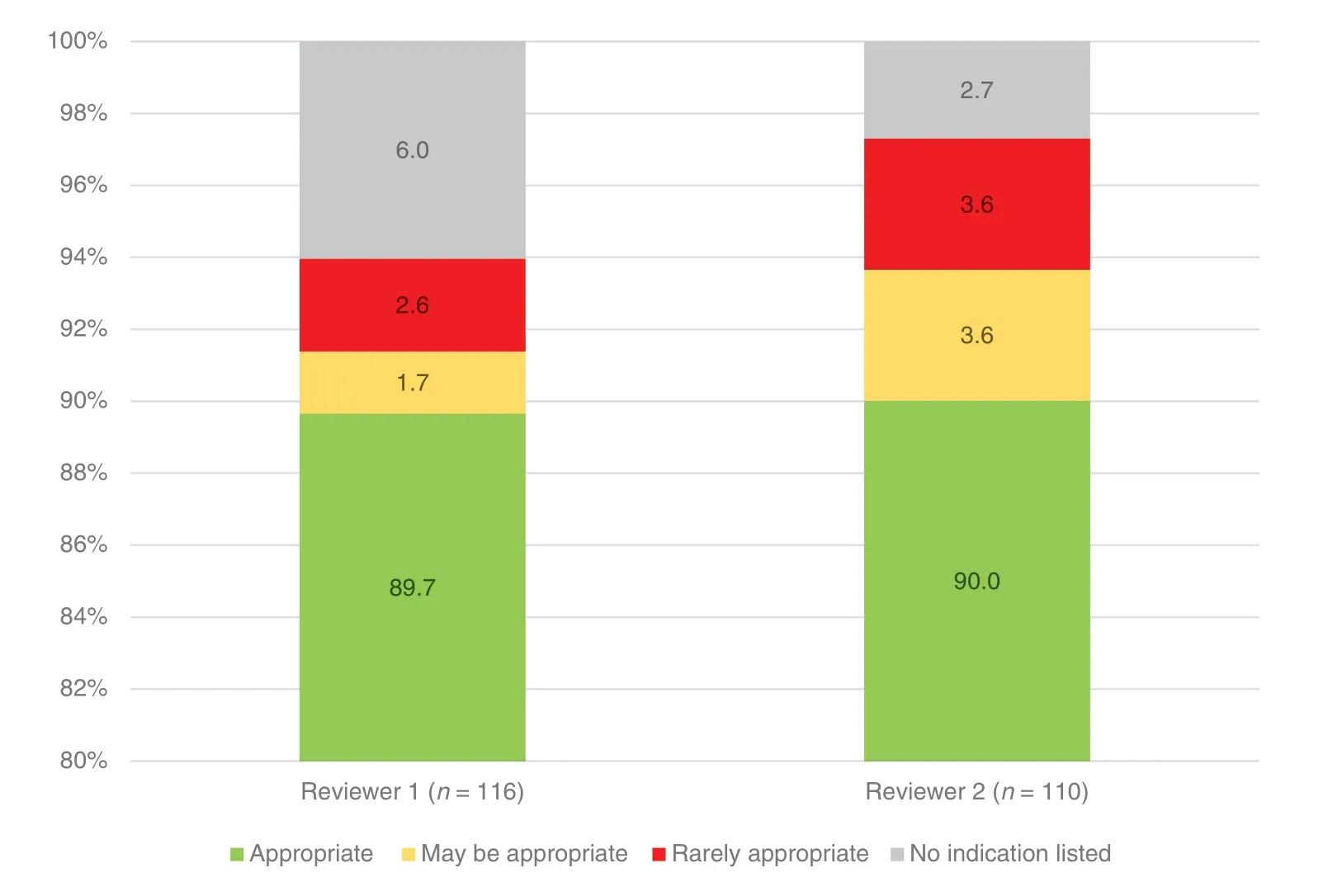
Figure4:Appropriateness of Secondary Prevention Implantable Cardioverter-Def brillator Implantations.
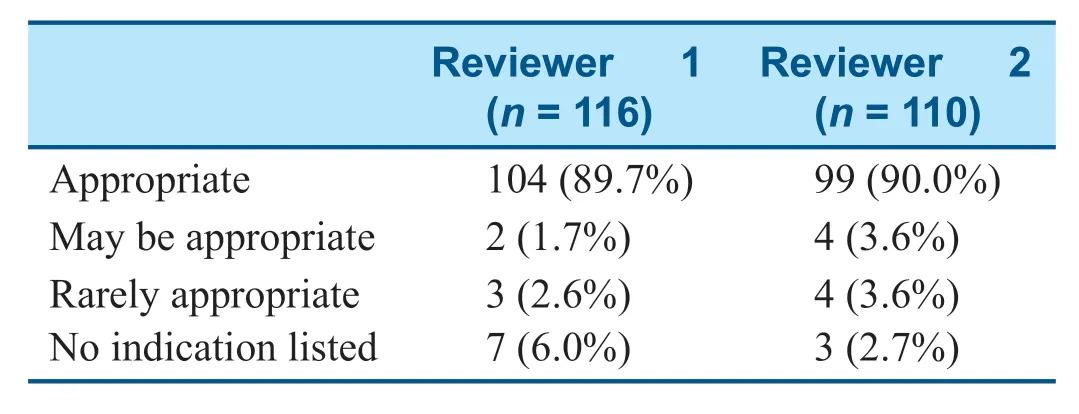
Table5 Appropriateness of Secondary Prevention Implantable Cardioverter-Def brillator Implantations.
The greatest limitation of this study is the small sample size (n=286) and the subsequent limitation in power,which may limit generalizability.Baseline demographics were similar to those of other major ICD trials [7–9].Furthermore,as this study examined ICD implantation in a university setting in which ICDs are implanted only by electrophysiologists,it may not represent clinical practice in settings in which ICDs may be implanted by nonelectrophysiologists,such as general cardiologists and thoracic surgeons [4,5].
Some patients had ICDs implanted for secondary prevention,but if there were no clear or appropriate secondary prevention indications,the reviewers may have instead listed a primary prevention indication,which would falsely decrease the rate of rarely appropriate or unrated secondary prevention ICD implantation.Similarly,the differences in appropriateness rates between reviewers may have been due to differences in how strictly each reviewer interpreted the AUC.For example,the reviewers disagreed on whether class IV symptoms were a contraindication,regardless of whether the patient was listed for transplantation.Of note,the most recent ICD guidelines [10],which were published in 2018 after the reviewers had assessed appropriateness for this study,recommend ICD implantation in patients who are candidates for transplantation or ventricular assist device implantation;however,this recommendation was not included in prior guidelines [1 1].The updated guidelines also expand recommendations for ICD implantation in patients with genetic,neuromuscular,and congenital heart disorders [10],some of which were not included in the AUC [2].
Lastly,given that the reviewers were physicians at the academic center studied,there may have been a degree of observer bias involved in rating appropriateness.The differences in appropriateness rates between reviewers were not statistically signif cant,with P=0.44 for all ICD implantations,P=0.90 for primary prevention ICD implantations,and P=0.50 for secondary prevention ICD implantations.
The Medicare national coverage determination determines reimbursement for ICDs based on indication.It is based on major ICD trial criteria from MADIT,MADIT II,MUSTT,and SCD-HeFT [3],although indications were last added in 2005 [12].Should the Medicare national coverage determination be based on AUC in the future,any gaps orinadequacies of the AUC would negatively impact patients,clinicians,and hospitals if clinically indicated ICDs are not reimbursable.

Table6 Comparison with Prior Registry-Based Studies.
When one is considering the application of these f ndings to clinical practice,it is important that each patient receive individualized care,irrespective of the guidelines.Although the AUC may aid clinical practice and decision-making,they cannot provide guidance in every scenario for every patient.If an indication is not listed or rarely appropriate,clinical judgment must determine whether a specif c patient would benef t from ICD implantation.
Conclusion
Compared with prior registry data reports,the prevalence of rarely appropriate ICD implantation at our facility was very low.Our high appropriate use rate could be explained by appropriate clinical practice or by the AUC being evidence based and ref ecting clinical practice.The AUC have gaps and could benef t from additional indications regarding secondary prevention.Most importantly,clinical judgement and individualized care should deter -mine which patients receive ICDs irrespective of guidelines or criteria.
Acknowledgements
None.
Ethics Approval and Consent to Participate
This study was approved by the University of Florida Institutional Review Board (ID no.IRB201600095).Given the deidentif ed data used in this study,patient consent was not required.
Consent for Publication
Not applicable.
Availability of Data and Material
The datasets generated and/or analyzed during the current study are not publicly available as they were extracted from University of Florida Health electronic medical records and entered into a REDCap database.Deidentif ed data were used for subsequent analysis but are available from the corresponding author on reasonable request.
Conf ilcts of lnterest
The authors declare that they have no conf icts of interest.
Funding
None.
Author Contributions
The implantable cardioverter -def brillators studied were implanted by MK,TAB,WMM,and MM.NHS,DEW,and MM were responsible for study design.NHS,SJR,SANN,JM,and AK were responsible for data collection,which was supervised by MM.NHS analyzed the f nal dataset.DEW was responsible for statistical analysis.NHS was responsible for drafting the manuscript,and SJR,DEW,TAB,and MM were involved in editing the manuscript.All authors read and approved the f nal manuscript.
 Cardiovascular Innovations and Applications2021年2期
Cardiovascular Innovations and Applications2021年2期
- Cardiovascular Innovations and Applications的其它文章
- Progress in the Study of the Left Atrial Function lndex in Cardiovascular Disease:A Literature Review
- A Nomogram to Predict Patients with Obstructive Coronary Artery Disease:Development and Validation
- Calcium-Sensing Receptor of lmmune Cells and Diseases
- The Relationship between Abnormal Circadian Blood Pressure Rhythm and Risk of Readmission in Patients with Heart Failure with Preserved Ejection Fraction
- Comparison of Diagnostic Effects of T2-Weighted lmaging,DWl,SWl,and DTl in Acute Cerebral lnfarction
- A Case of Pediatric Heart Failure Caused by Anomalous Origin of the Left Coronary Artery from the Pulmonary Artery:Case Report and Literature Review
