Endothelial keratoplasty combined with scleral fixation intraocular lens
Mariantonia Ferrara, Danilo Iannetta, Luca Pagano, Kunal A Gadhvi, Vito Romano,5
1Newcastle Eye Centre, Royal Victoria Infirmary, Newcastle upon Tyne NE1 4LP, United Kingdom
2Arcispedale Santa Maria Nuova, Reggio Emilia 42123, Italy
3Department of Corneal and External Eye Diseases, St Paul’s Eye Unit, Royal Liverpool University Hospital, Liverpool L7 8XP, United Kingdom
4Department of Biomedical Science, Humanitas University, Pieve Emanuele-Milano 20090, Italy
5Department of Eye and Vision Science, University of Liverpool, Liverpool L7 8TX, United Kingdom
Dear Editor,
We describe, for the first time, the surgical management of two aphakic patients with corneal decompensation treated with concomitant ultrathin-Descemet stripping automated endothelial keratoplasty (UT-DSAEK) and implantation of two different scleral-fixated (SF) intraocular lenses (IOLs), namely sutureless SF (SSF) Carlevale IOL (Soleko, Italy; Figure 1) or Morcher Type 90L IOL (Morcher GmbH, Germany; Figure 2). Both IOLs are hydrophilic acrylic. The Carlevale IOL is 13.2 mm long with a 6.5 mm optic plate, foldable and injectable through a 2.2 mm corneal tunnel. A T-shaped harpoon protrudes oあ the closed haptics and is designed to be externalized underneath a partial thickness scleral flap (Figure 1). The Morcher Type 90L IOL is 15 mm long with a 6.5 mm optic plate. The two C-loop haptics have an eyelet for the passage of the sutures for the scleral fixation (Figure 2).
Vision impairment resulting from aphakia in absence of capsular support may be effectively managed with the implantation of a variety of IOLs including anterior chamber (AC), iris-fixated and scleral-fixated IOLs[1]. In cases of concomitant corneal decompensation, the combination of corneal transplant with IOL scleral fixation has been proposed as a safe and eあective option to address issues with both the cornea and the lens leading to a faster visual rehabilitation[2-4].Moreover, modern endothelial keratoplasty (EK) and new generation foldable SF IOLs allow to perform minimally invasive procedures to be undertaken.
Two patientswith corneal decompensation and aphakia were referred to the corneal service in the Royal Liverpool University Hospital, for evaluation of secondary IOL implant and corneal transplant. Patients were properly informed about their inclusion and signed an informed consent form. The study complied with the principles of the Declaration of Helsinki, and was approved by the Clinic Ethics Committee.
CASE 1
A 79-year-old man presented with pain and reduction of vision due to aphakia and corneal decompensation in his right eye. He had a history of complicated cataract surgery with dropped nuclear fragments followed by pars plana vitrectomy (PPV) and iris-claw Artisan IOL implantation. His initial surgery was complicated by postoperative persistent cystoid macular oedema for 8mo later and he had undergone subsequent Artisan IOL removal complicated by aphakic corneal endothelial decompensation. At presentation, ophthalmic examination of the right eye demonstrated best corrected visual acuity (BCVA) of counting fingers (CF), intraocular pressure (IOP) 16 mm Hg, corneal edema, Descemet’s folds, aphakia and absence of capsular support. Fundus examination demonstrated attached retina and absence of cystoid macular edema on optical coherence tomography scans. Endothelial cell density (ECD) was not measurable. The patient underwent to combined Carlevale IOL SSF implantation and UT-DSAEK.

Figure 1 Schematic diagram of the Carlevale IOL and representation of surgical of implantation A: Carlevale IOL; B: Temporal and nasal scleral flap at 0°-180°, temporal corneal wound and nasal paracentesis; C: The leading harpoon is externalized; D: Final position of Carlevale IOL once also the trailing harpoon is externalized.

Figure 2 Schematic diagram of the Morcher Type 90L IOL and representation of surgical of implantation A: Morcher Type 90L IOL; B: Each IOL haptic are locked by a looped 10-0 polypropylene suture. The loops are externalized through partial-thickness sclera at 2 and 8 o’clock; C: After cutting one string of the externalized looped suture, the armed end is passed through partial-thickness sclera for about 0.5 mm. D: Creation of two knots, on in correspondence of the scleral bite and the second one 4-5 mm away from it. E: Creation of a half-thickness scleral tunnel of about 2-3 mm using the needle. F: Suture ends are buried into the tunnel.
Surgical TechniqueThe surgery was performed under peribulbar anesthesia. The technique used for SSF Carlevale IOL implantation was that described by Barcaet al[5]. Two limbus landmarks were marked along the horizontal meridian at 0°-180° degrees. After two limited conjunctival peritomies, two scleral flap of 4×4 mm2and two sclerotomies 1.5 mm away from the limbus were performed at 0°-180°. This was followed by the creation of a temporal corneal wound of 2.75 mm and a nasal paracentesis. Concomitantly to the injection of the Carlevale IOL through the corneal incision, 25 G forceps were inserted through the nasal sclerotomy to grasp the leading T-shaped harpoon. Once the leading harpoon was externalized, the trailing harpoon was grasped with the first 25 G forceps inserted through the paracentesis and passed to other 25 G forceps inserted through the temporal sclerotomy using the handshaking technique. The second T-shaped harpoon was externalized without any further manoeuvres on the IOL (Figure 1). After the suture of the scleral flaps, an AC maintainer was inserted through a paracentesis, and a descemetorhexis was performed. Using the iGlide a preloaded ultrathin DSAEK was delivered through the main paracentesis using 25 G forceps (pull through technique). Once delivery was completed, the tissue was held with forceps until it was unfolded and attached. An air bubble was injected into AC to secure the graft to the corneal stroma. Finally, the corneal incision was sutured with 10-0 nylon and the conjunctiva with 8-0 vicryl. The patient was positioned supine for 36h. No intraoperative complications occurred.

Figure 3 IOL tilt angle of Carlevale IOL A: Horizontal plan; B: Vertical plan.
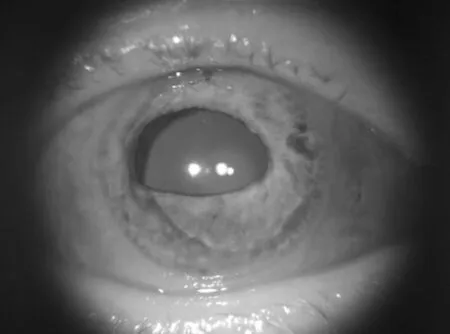
Figure 4 Anterior segment picture of the right eye of the patient who underwent combined Carlevale IOL SSF implantation and UT-DSAEK at 9-month follow-up.
Postoperative therapeutic regimen included chloramphenicol 0.3% for 2wk and dexamethasone phosphate 0.1% every 2h for 1wk, then 4 times a day for 4mo then twice a day long term.
Follow-upThe BCVA progressively improved from CF to 20/80 at 9-month follow-up. The IOP remained within normal limits. The corneal graft appeared well apposed, clear and centred, the IOL in place and the retina secure. The mean IOL tilt was 1.9°, calculated by averaging the IOL tilt angle on the vertical plane (0.3°) and the horizontal plane (3.5°; Figures 3, 4). As proposed by Yamaneet al[6], the IOL tilt was considered the angle between the IOL horizontal axis and a straight reference line between the iridocorneal angles of each side. No postoperative complication was noted during the follow-up (FU).
CASE 2
Fifteen months prior to presenting in the clinic, a 56-yearold man was treated with PPV, silicone oil (SO) tamponade and inferior iris suture with no IOL implantation in the left eye for partial aniridia, dropped crystalline lens and retinal detachment following ocular trauma. Three months after, the SO was removed and the patient developed progressive corneal edema. At presentation, the left eye had BCVA of CF, IOP 21 mm Hg, corneal edema, Descemet’s folds, inferior iris suture with residual superotemporal iris defect and aphakia with no capsular support, retina apparently flat. The central corneal thickness was 784 μm and ECD not measurable. The patient underwent combined UT-DSAEK and implantation of SF Morcher Type 90L IOL.
Surgical TechniqueThe surgery was performed under peribulbar anesthesia. The technique used for SF was that described by Kiret al[7], without any scleral flap. Briefly, two limbus landmarks were marked at 2 and 8 o’clock. The eyelet of each IOL haptic was engaged and locked by a looped 10-0 polypropylene suture. The curved needles were externalized 1 mm away from the limbus passing through the ciliary sulcus. After the injection of the IOL in the ciliary sulcus, the externalized loop was cut and the armed end passed through partial-thickness sclera for about 0.5 mm. Two knots were created, the first in correspondence of the partial-thickness scleral bite and the second 4-5 mm away from the first. The needle was then used to create a half-thickness scleral tunnel of about 2-3 mm and, after cutting the second knot, the suture ends were buried into the tunnel (Figure 2). Then, a corneal wound of 2.75 mm at 90° was created and the UT-DSAEK was performed as in patient 1. No intraoperative complications occurred. Postoperative management was the same as received by patient 1.
Follow-upAt 2-month postoperative FU, left IOP was 28 mm Hg; therefore dexamethasone phosphate 0.1% was switched to loteprednol etabonate 0.5% and the combination of bimatoprost (0.3 mg/mL) and timolol (5 mg/mL) once a day was started. At last FU, 8mo after surgery, BCVA was 20/100, IOP well controlled, the corneal graft clear and well attached, the IOL well centered with mean IOL tilt of 9.75° (Figures 5, 6).
DISCUSSION
Bullous keratopathy can accompany aphakia following complicated cataract surgery or ocular trauma resulting in severe visual impairment[2]. Modern UT-DSAEK has been demonstrated to provide fast, reproducible and effective rehabilitation of corneal endothelial disease[8]. Recently, DSAEK has been successfully combined with iris clipped, glued and flanged intrascleral IOLs for the management of aphakic bullous keratopathy[2-4,9-10]. Combined surgeries offer several significant advantages, such as optimization of surgical time, avoiding multiple sequential surgeries and faster visual rehabilitation[2-3]. Moreover, in aphakic eyes treated with endothelial transplant, concomitant IOL implantation can reduce the risk of migration of the graft into the vitreous chamber and support graft attachment helping to maintain the bubble of air in the AC[10].

Figure 5 IOL tilt angle of Morcher Type 90L IOL A: Horizontal plan; B: Vertical plan.
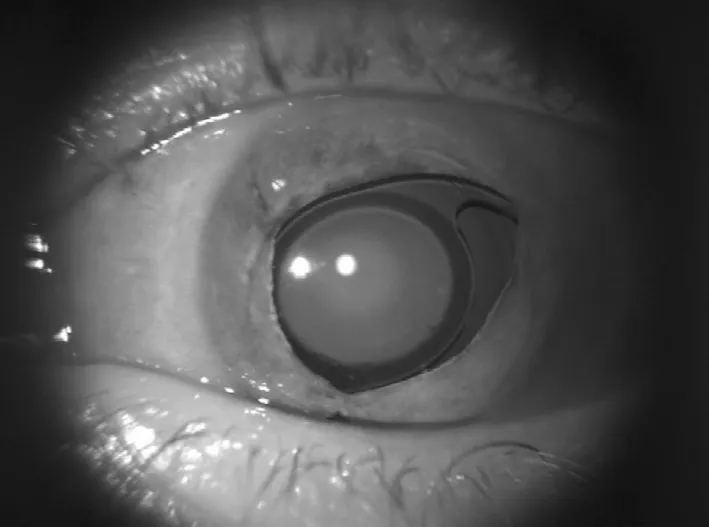
Figure 6 Anterior segment picture of the left eye of the patient who underwent combined UT-DSAEK and implantation of SF Morcher Type 90L IOL at 8-month follow-up.
Compared with AC-IOLs and iris-fixated IOLs, scleral-fixated IOLs could be favored due to the absence of corneal and angle trauma with potentially reduced endothelial cell loss, decreased risk of pupillary block and secondary glaucoma, minimal or no contact with the iris and smaller corneal incision due to their foldability[1]. We present two cases of DSAEK combined, for the first time, with SSF Carlevale IOL implantation in one eye and SF of Morcher Type 90L IOL in the second eye, demonstrating the feasibility and eあectiveness of these procedures. The scleral fixation of IOLs is a valuable procedure in aphakic eyes and has been traditionally performed using 10-0 polypropylene sutures[11]. However, several concerns exist over suture-related complications, such as knot erosion, infection, IOL tilt and suture slippage or degradation with consequent long term IOL instability[4,12]. In particular, IOL tilt can impact significantly on the vision even in case of successful surgery; indeed, an IOL tilt of about 5° can cause additional refractive error, whereas higher-order aberrations not correctable with spectacles can be induced by IOL tilt >15°[13]. In combination with EK, this potential complication can also be more relevant considering that the EK itself has been associated with a potential mild hyperopic shift[7]. In our report, visual acuity markedly improved in both patients but the tilt angle of Carlevale IOL was significantly smaller than that of Morcher IOL. This is consistent with previous case series highlighting the ease of implantation and stability of Carlevale IOL[5,14]. Barcaet al[5]suggested that the low tilt degree of Carlevale IOLs may be related to the presence of a harpoon instead of the haptic, as the former could tolerate better the stress of the surgical manipulation without deforming.
In conclusion, the combination of UT-DSAEK with both SSF of Carlevale IOL and SF Morcher Type 90L IOL appeared to be an eあective and safe option for the surgical management of corneal decompensation in aphakic patients resulting in good visual and anatomical outcomes. However, Carlevale IOL was easier to handle and resulted in a smaller IOL tilt angle, overcoming potential complications related to sutured SF, such as pseudophaco-donesis, IOL instability, IOL tilt, haptic erosion and suture lysis.
ACKNOWLEDGEMENTS
The authors thank Hannah Levis for proofreading this paper.
Authors’ contribution:Ferrara M and Romano V designed the work; Iannetta D, Pagano L and Gadhvi KA acquired and analysed the data; Ferrara M, Iannetta D, Pagano L and Gadhvi KA drafted the work, Romano V revised critically the work. All authors approved the submitted version and agreed to be accountable for all aspects of the submitted work.
Conflicts of Interest:Ferrara M,None;Iannetta D,None;Pagano L,None;Gadhvi KA,None;Romano V,None.
 International Journal of Ophthalmology2021年1期
International Journal of Ophthalmology2021年1期
- International Journal of Ophthalmology的其它文章
- Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid
- Preliminary studies of constructing a tissue-engineered lamellar corneal graft by culturing mesenchymal stem cells onto decellularized corneal matrix
- Therapeutic potential of Rho-associated kinase inhibitor Y27632 in corneal endothelial dysfunction: an in vitro and in vivo study
- Changes of matrix metalloproteinases in the stroma after corneal cross-linking in rabbits
- A multi-omics study on cutaneous and uveal melanoma
- Eあects of quercetin on diabetic retinopathy and its association with NLRP3 inflammasome and autophagy
