Corneal epithelial thickness analysis of forme fruste keratoconus with optical coherence tomography
Xiao-Long Yang, Yun Wang, Bao-Gen Luo, Yue Xu, Xiao-Feng Zhang
Department of Ophthalmology, the First Aきliated Hospital of Soochow University, Suzhou 215000, Jiangsu Province, China
Abstract
INTRODUCTION
Keratoconus is a bilateral ectatic corneal disease and is more in the incidence in adolescence[1]. It manifests as progressive loss of vision and causes visual impairment, seriously aあect patients’ life and work. About 20% of patients may require corneal transplantation ultimately[2]. If keratoconus can be diagnosed early, patients will have the opportunity to undergo treatments, like corneal cross linking, which can reduce the need for future corneal transplantation[3-4]. Although the equipment and technology of keratorefractive surgery have been continuously improving in the past 30 years, corneal ectasia after refractive surgery is still an inevitable complication[5-7]. Post-refractive surgery corneal ectasia might be related to surgical stimulation that causes the “potential” keratoconus to enter the active stage[8-9]. Corneal topography is a reliable detection technique for clinical keratoconus[10-11]. There are many techniques can be used for the early detection of keratoconus. Scheimpflug camera can measure posterior corneal elevation for discriminating subclinical keratoconus[12]. Ocular Response Analyzer can obtain corneal biomechanical waveform parameters, which changes prior to corneal topography[13-14]. Since keratoconus is a congenital disease, next-generation sequencing can also be used for the early diagnosis of keratoconus[15-17]. VSX1[18], DOCK9[19], SOD1[18]and TGFBI[19]had been proven to be related to keratoconus. But for all this, misdiagnosis of keratoconus is not uncommon[1].
Forme fruste keratoconus is topographically normal-appearing eye of patients with keratoconus in the fellow eyes[20]. Corneal hysteresis and corneal resistance factors in forme fruste keratoconus eyes were lower than that of normal eyes[14,21]. During the long-term follow-up period, about 20% of eyes with forme fruste keratoconus have progressed to clinical keratoconus within 6y[22]. Therefore, biological study of forme fruste keratoconus provides reference for the early diagnosis of keratoconus.
Corneal epithelial remodeling refers to the ability of corneal epithelium to repair irregular anterior corneal surface by compensatory thickening in a certain range when the corneal stroma changes[23]. During the early stages of keratoconus, corneal epithelial remodeling can mask the irregular changes of the stroma, resulting in no differences in the detection of topographic maps of the anterior surface[24]. Currently, the most commonly used clinical methods to measure corneal epithelial thickness included optical coherence tomography (OCT)[25], very-high frequency ultrasound[26-27], confocal microscopy[28]and so on. The Fourier-domain OCT (FD-OCT) has excellent repeatability and accuracy[29], avoiding the measurement error caused by corneal edema without anesthesia. Therefore, OCT might be considered as one of the most valuable techniques in the diagnosis of early keratoconus[1]. Hence, in this study, the thickness of corneal epithelium in the range of 9 mm diameter centered pupil center in forme fruste keratoconus, clinical keratoconus and corneal astigmatism (ΔK) eyes was analyzed by FD-OCT.
SUBJECT AND METHODS
Ethical ApprovalThis retrospective case-control study included the data collected before and was of low risk, and so the need for consent was waived by the Medical Ethics Committee of the First Affiliated Hospital of Soochow University [(2019) Ethical approval No.176]. This study was conducted in accordance with the ethical standards of the institutional and/or national research committee and the principles of Helsinki declaration.
SubjectsThe study included 47 keratoconic patients (37 males, and 10 females) who were newly diagnosed in the Ophthalmology Department of the First Aきliated Hospital of Soochow University from January 2015 to December 2019 and 80 astigmatic patients (44 males, 36 females) who underwent treatment in the same period as controls. All patients had no rigid contact lens wear and did not wear soft contact lens during the previous 2wk. All patients do not have any history of corneal refractive surgery or corneal cross-linking surgery.
Diagnostic CriteriaThe diagnostic criteria of clinical keratoconus group (A group) were as follows[30]: the patients’ both eyes included a typical corneal topographical change (central or paracentral conical ectasia); and the slit lamp examination should include at least one of the following clinical signs: 1) Munson sign; 2) Fleischer ring; 3) Vogt striae; and 4) corneal conical ectasia or corneal stromal thinning. The diagnostic criteria of forme fruste keratoconus group (B group) were as follows: patients with no clinical signs of keratoconus with slit lamp microscope and no abnormalities were found by using corneal topography. The contralateral eye presented a typical corneal topography of keratoconus and clinical signs.Inclusion criteria for high ΔK group (C group) were as follows: 1) both slit lamp examination and corneal topographic examination showed no corneal abnormalities; and 2) ΔK (steep K-flat K) of >2.0 D as examined by corneal topography. Inclusion criteria for low ΔK group (D group) were as follows: 1) both slit lamp examination and corneal topographic examination showed no corneal abnormalities; and 2) ΔK ≤2.0 D as examined by corneal topography.
Except for forme fruste keratoconic patients, all other patients were enrolled with the right eye.
Corneal TopographyThe topographical maps of the corneal anterior surfaces were examined by TMS-4 corneal topographer (Tomy, Japan) and the examinations were performed by the same technician. The eye check has been done thrice, choosing the best pattern (X, Y, Z axes deviation is less than 0.3 mm) to obtain flat keratometry (Kf), steep keratometry (Ks), average keratometry (AveK), ΔK, corneal surface regularity index (SRI), and corneal surface asymmetry index (SAI).
Corneal Optical Coherence TomographyThe corneal epithelial thickness was measured by an FD-OCT system RTVue-100 (Optovue Inc., Fremont, CA, USA). The examination was carried out in a semi-dark environment, and no drugs that aあect the tear dynamics were used 2h before the examination. This examination was done by the same technician. Scanning with PachymetryWide mode was done by instructing the patient to fix on the light spot, and obtaining data of corneal epithelial thickness within a circular area of a diameter of 9 mm centered on the pupil center. The results were expressed in a topographical map.
Topographic Map of Corneal Epithelial ThicknessThe topographic map of corneal epithelial thickness was divided into 25 zones: a 2.0 mm diameter circle central zone centered on the pupil center, and 24 sector-shaped ring zones that are equally divided by 4 axial directions from 2.0 to 5.0 mm, 5.0 to 7.0 mm, and 7.0 to 9.0 mm annular areas. The average corneal epithelial thickness was read from the 25 zones per eye.
Morphology classification of corneal epithelial thickness topography (Figure 1): 1) uniformity shape: no obvious local thickening or thinning of corneal epithelium was observed, and the color was uniform; 2) crater shape: the corneal epithelium was thickened in the peripheral part centered on the thinnest point of the corneal epithelium. The crater shape was subdivided into: a) c font shape: the corneal epithelium is thickened in c-shape and centered on the thinnest point of the corneal epithelium; b) bracket shape: the corneal epithelium is thickened on both sides of the thinnest point of the corneal epithelium; and c) ring shape: the corneal epithelium is annularly thickened around the thinnest point of corneal epithelium; 3) irregular shape: the corneal epithelium is uneven in thickness and is colored in a disordered manner; 4) central island shape: the corneal epithelium is obviously thickened in the central region of the cornea.
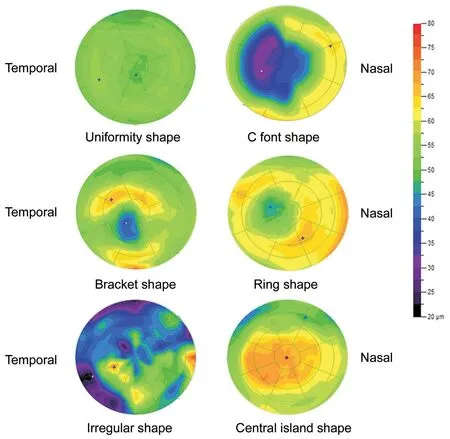
Figure 1 Morphological classification of corneal epithelial thickness topography The cool-tone portion (cyan) indicated a thinner portion, and the warm-tone portion (orange-red) indicated a thicker portion.
Comparison of the Thickness of the Thinnest Point of the Corneal EpitheliumThe FD-OCT system was used to obtain the thickness of the thinnest point of the corneal epithelium.
Distribution Curve of Corneal Epithelial Thickness in 45°, 90°, and 135° AxesThe 45°, 90°, and 135° axial direction measurement lines through the pupil center are taken to read the thickness of corneal epithelium at 1 mm intervals. The corneal epithelial thickness distribution curve of +4, +3, +2, +1, , -1, -2, -3, and -4 mm data points at 45°, 90°, 135° axes were obtained from the clinical keratoconus group, forme fruste keratoconus group, high ΔK group, and low ΔK group, respectively (Figure 2). The differences of corneal epithelial thickness at the same data point from the three axes in the clinical keratoconus group, the forme fruste keratoconus group, the high ΔK group and the low ΔK group were compared and then analyzed.
Statistical AnalysisData analysis was performed with SPSS 17.0 statistical software (version 17.0, Chicago, Illinois, USA). One-way ANOVA was performed to compare the thinnest point in the corneal epithelial thickness of the four groups. If there is a statistically significant diあerence in oneway ANOVA, further LSD test was performed (P<0.05). For comparison of the thickness of corneal epithelium at the same data point in each axis in each group, the homogeneity test of variance was first performed. If the variance is uniform, then one-way ANOVA was used. If there was any significant difference, further LSD test was performed (statistically significant diあerence atP<0.05); and if the variance was not uniform, then Kruskal-Wallis test was done. Furthermore, Bonferroni correction was performed if there was a statistically significant diあerence (adjust test level α’=α/6=0.008).

Figure 2 Schematic representation of 45°, 90°, and 135° axial data points (unit: millimeter).
According to the sample size estimation formula of completely random design one-way ANOVA, we set α=0.05 (two-side), β=0.10 (one-side). The mean of the thinnest point of thickness of corneal epithelium of the four groups was 42, 49, 48, and 52 μm, and standard deviation σ=5 μm. The final calculated sample size was 9 cases in each group, 36 cases in total. Under such sample size, the statistical power was about 90%. In our article, the sample size of the four groups is 26, 21, 40 and 40 cases. There is sufficient statistical power to detect the diあerence between the groups.
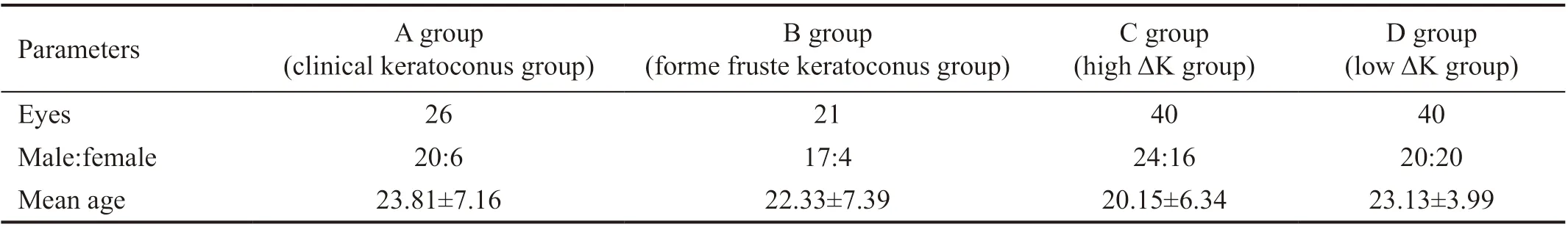
Table 1 The general data of the subjects

Table 2 Comparison of corneal topography parameters of each group
RESULTS
Patient DataA total of 47 keratoconic patients involved in the study, 26 of them were clinical keratoconus and the other were forme fruste keratoconus patients. Forty high ΔK subjects and 40 low ΔK subjects were also involved in the study (Table 1).Compared with other groups, clinical keratoconus group showed significantly higher Kf, Ks, AveK, ΔK, SRI and SAI (allP=0.000). Compared with high ΔK group, forme fruste keratoconus group demonstrated significantly lower Ks, ΔK, and SRI (PKs=0.004,PΔK=0.000,PSRI=0.005). No statistically significant differences were found between high ΔK group and forme fruste keratoconus group in Kf, AveK, and SAI. Compared with low ΔK group, there was no statistically significant diあerence between forme fruste keratoconus group and low ΔK group in Kf, Ks, AveK, ΔK, SRI and SAI (Table 2).
Corneal Epithelial Thickness AnalysisThe overall thickness of forme fruste keratoconus group was thicker than that of clinical keratoconus group. Comparison of high ΔK group with low ΔK group showed that the forme fruste keratoconus group has thinner thickness and more uneven distribution (Figure 3).
Morphology Classification of Corneal Epithelial Thickness Topography1) Clinical keratoconus group: 25 eyes were of crater shape (96.15%), and 1 eye was of irregular shaped (3.85%). The crater shape was subdivided into: c font shape: 10 eyes (40%), bracket shape: 10 eyes (40%), and ring shape: 5 eyes (20%). 2) Forme fruste keratoconus group: 21 eyes were of uniformity shape (100%). 3) High ΔK group: 28 eyes were uniformity shape (70%), 12 eyes were of central island shape (30%). 4) Low ΔK group: 37 eyes were uniformity shape (92.5%), and 3 eyes were central island shape (7.5%).
The Thinnest Point Thickness of Corneal EpitheliumThe thinnest point in the corneal epithelial thickness was an average of 42.81±5.63 μm in the clinical keratoconus group, 49.33±3.33 μm in the forme fruste keratoconus group, 48.78±3.35 μm in the high ΔK group and 52.37±3.98 μm in the low ΔK group. There were statistically significant diあerences between the groups (F=32.012,P=0.000). The thinnest point in the corneal epithelial thickness of clinical keratoconus group was significantly lower than that of the other groups (allP=0.000). The thinnest point in the corneal epithelial thickness of forme fruste keratoconus group was significantly lower than that of low ΔK group (P=0.022). There was no statistically significant diあerence between forme fruste keratoconus group and high ΔK group (P=0.668).
Comparison of Corneal Epithelial Thickness of Each Group at 45°, 90°, and 135° AxesThe corneal epithelial thickness of clinical keratoconus group at 0 mm point was significantly thinner than that of other groups (P<0.008).
Comparison of corneal epithelial thickness of the four groups at +4, +3, +2, +1, -1, -2, -3, and -4 mm points of three axes were as follows: 1) 45° axis: The corneal epithelial thickness of clinical keratoconus group was significantly thicker than that of high ΔK group at +4, and -4 mm points (P+4mm=0.015,P-4mm=0.042), and were significantly thinner than that of the other groups at -1, and -2 mm points (P-1mm<0.008,P-2mm<0.05). 2) 90° axis: The corneal epithelial thickness of clinical keratoconus group was significantly thicker than that of high ΔK group at +4, +3, and +2 mm points (P+4mm=0.014,P+3mm=0.022,P+2mm= 0.010), and significantly thinner than that of other groups at -1 mm point (P<0.05), and thinner than that of low ΔK group at -2 mm point (P=0.000). The corneal epithelial thickness of forme fruste keratoconus group was significantly thinner than that of low ΔK group at -1, and -2 mm points (P-1mm=0.015,P-2mm=0.036). 3) 135° axis: The corneal epithelial thickness of clinical keratoconus group was significantly thicker than that of high ΔK group at +4, +3, and -3 mm points (P+4mm=0.031,P+3mm=0.000,P-3mm=0.005), and was significantly thinner than that of low ΔK group at +1 mm point (P=0.000), and significantly thinner than that of other groups at -1 mm point (P<0.05), and significantly thicker than that of forme fruste group at -3 mm point (P=0.024). No statistically significant differences were observed between groups at other points (Figure 4).

Figure 3 Topographic map of corneal epithelial average thickness of each group with a diameter of 9 mm.
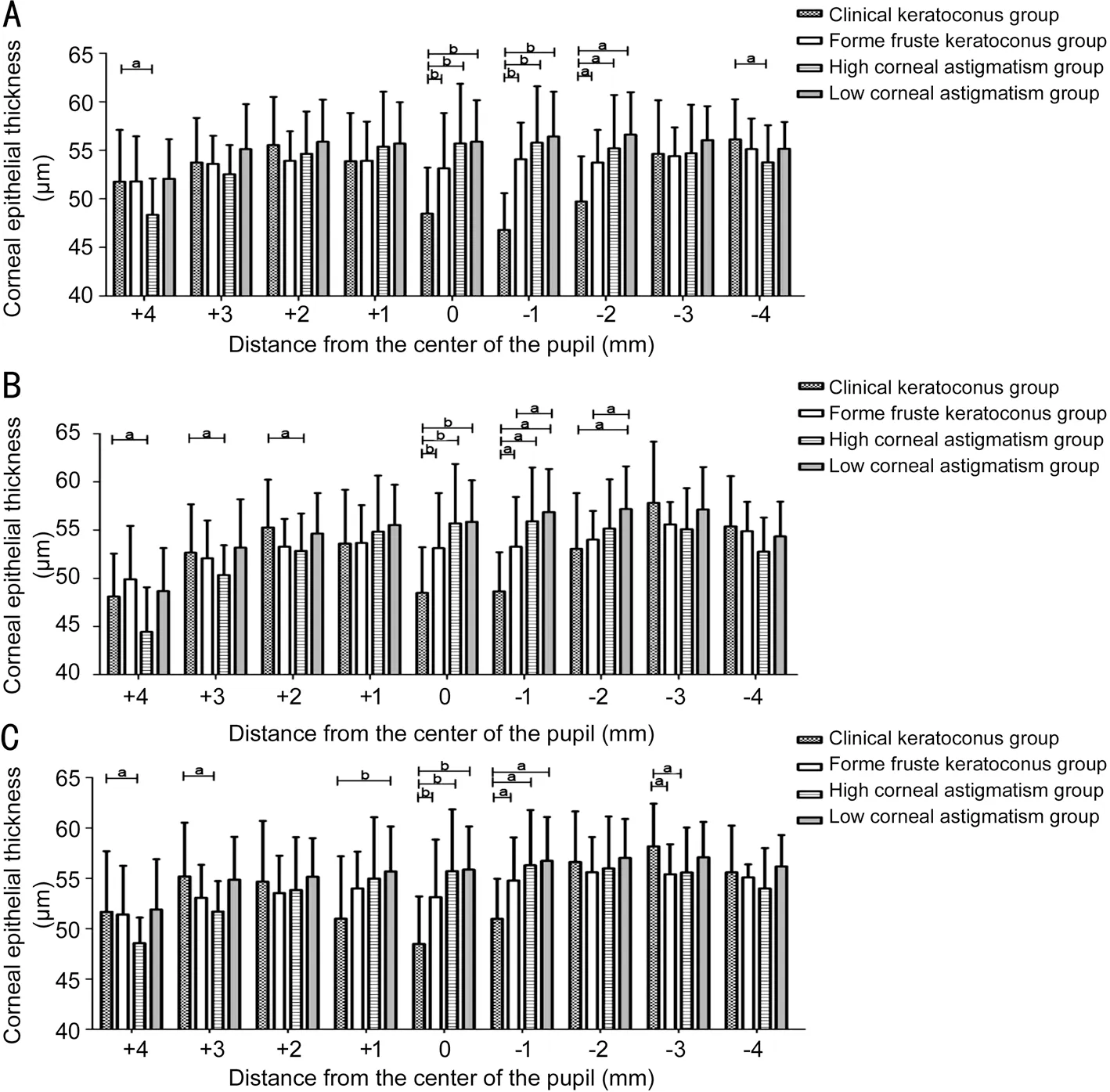
Figure 4 Bar chart of corneal epithelial thickness of each group in three axes A: 45°; B: 90°; C: 135° axes. aP<0.05, bP<0.008.
DISCUSSION
Clinical keratoconus diagnosis mainly relies on the morphology of corneal anterior surface topography and typical slit-lamp findings, such as Fleischer ring, Vogt striae and corneal scar[1]. As the subclinical keratoconus stromal changes can be compensated by corneal epithelial remodeling to a certain extent[31], patients often do not have any typical clinical signs, and the changes in the anterior corneal surface can be masked[24]. In this study, there were no statistically significant diあerences in the parameters of the anterior surface topography between the forme fruste keratoconus group and the low ΔK group. They are even smaller than the high ΔK group with regards to the parameters of Ks, ΔK, and SRI. Therefore, anterior corneal topography is not considered sensitive to the diagnosis of early keratoconus, and may even lead to misdiagnosis of early keratoconus.
Liet al[32]evaluated the corneal epithelial pattern map in 6 mm diameter range found that epithelial thinning inferiorly in forme fruste keratoconus. Reinsteinet al[24]found that the corneal epithelial thickness topography showed a similar epithelial doughnut pattern. On this basis, 21 cases of corneal epithelial thickness topography in forme fruste keratoconus in 9.0 mm diameter range were evaluated, and similar findings were observed in our study. The “crater shape” corneal epithelial thickness topography was observed only in the clinical keratoconus group, but no similar changes were found in the forme fruste keratoconus group and the ΔK group in our sthdy. The “crater shape” corneal epithelial thickness topography can be further subdivided into the c font shape, the bracket shape and the ring shape. Corneal epithelial remodeling is an important mechanism for the formation of the “crater shape” corneal epithelial thickness topography, and its initiating factors are controversial. One hypothesis is that epithelium thickening is to compensate for the thinning of the corneal stroma and is related to the rate of corneal stromal curvature change[33]. The epithelial thinning to compensate for relative peaks in stromal and thickening to compensate for relative troughs in stromal. The cornea surface tends to form a smooth shape that maintains its optical properties. This can explain the formation of the “crater shape” corneal epithelial thickness topography. Another hypothesis is that biomechanically unstable cornea drived epithelial remodeling, which was related to intraocular pressure variations, eye rubbing and blinking mechanism[34]. The cornea local biomechanical properties reduction results in tissue thinning as the weaker area strains[35]. Forme fruste keratoconus is usually considered as the mildest and the earliest form of keratoconus[36]. This study showed that all corneal epithelial thickness topographies of forme fruste keratoconus group were uniformity shape, and so the forme fruste keratoconus did not undergo corneal epithelial remodeling.
Corneal epithelial thickness topography in astigmatism group can be divided into uniformity shape and central island shape. The proportion of central island shape in high ΔK group is much higher than that in the low ΔK group. A study showed that the rate of corneal stromal curvature change drived epithelial remodeling[33]. Therefore, it the classification of corneal epithelial thickness topography was related to the rate of corneal stromal curvature change. In clinical keratoconus, diあerent cone sizes lead to diあerent rates of curvature changes, resulting in different types of epithelial thickening. The higher the ΔK is, the greater the rate of curvature change is. Therefore, the corneal epithelial thickness topography of high ΔK group was more of central island shape. A previous study has shown that epithelial irregularity should be considered as a possible contributing factor to astigmatism. Therefore, corneal epithelial thickness topography can be used to differentiate early keratoconus from high astigmatism[37].
The thinnest point of corneal epithelial thickness in the clinical keratoconus group was lower than that in the other groups, which was consistent with the clinical manifestations of keratoconus. The thinnest point thickness of corneal epithelium of forme fruste keratoconus group was significantly lower than that of the low ΔK group, but showed no statistical diあerences from that of the high ΔK group. Blinking action and force may be another mechanism of corneal epithelial remodeling[38]. Considering that the high ΔK patients had higher frequency of half-shutting eyes than the low ΔK patients, the eyelid force led to corneal epithelial remodeling, which was then manifested by the thinning in the upper corneal epithelium and thickening in the central corneal epithelium. So, more central island shape appeared in the high ΔK group. Under the circumstances, the corneal epithelial thinnest point of high ΔK group appears in upper corneal epithelium. In this study, central island shape accounted for 30% in the high ΔK group. This may be the cause of low thickness of the thinnest point of corneal epithelium in high ΔK group. Therefore, the thinnest point thickness of corneal epithelium alone is not enough to distinguish forme fruste keratoconus eye from high ΔK eye.
The thickness of corneal epithelium in the clinical keratoconus group and other groups was mainly manifested in the thinning of a 2.0 mm diameter circle central zone centered on the pupil center, especially in the temporal inferior area. This phenomenon in turn is associated with corneal epithelial thinning at the top of the cone. The epithelial thickness of clinical keratoconus group was significantly thicker than that of forme fruste keratoconus group at -3 mm point at 135° axial direction, and thicker than that of high ΔK group at -3 mm point at 135° axial direction. The “crater shape” thickening of keratoconus corneal epithelium is most prominent in the nasal inferior area. The epithelial thickness of forme fruste keratoconus group was significantly thinner than that of low ΔK group at -1, -2 mm points at 90° axial direction. This may be related to the thinning of corneal epithelial thinnest point, as it appears earlier than the corneal epithelial remodeling.
The epithelial thickness of high ΔK group was significantly thinner than that of clinical keratoconus group at +4, -4 mm points at 45° axial direction and +4, +3, +2 mm points at 90° axial direction and +4, +3 mm points at 135° axial direction. This was consistent with the thinning of the peripheral corneal epithelium in the high ΔK group.
The phenomenon of epithelial remodeling, thinnest point thinning, thinnest point position change[38]existed in the keratoconus. Combined with our study, the corneal epithelial thickness topography of the forme fruste keratoconus group showed no changes, but the thinnest point thickness was significantly lower than that of the low ΔK group. This inferred that the phenomenon of the thinnest point thinning appears earlier than the corneal epithelial remodeling in the pathogenesis of keratoconus. Therefore, the phenomenon that the thinnest point thickness of corneal epithelium was lower than that of the normal remained significant in the diagnosis of early keratoconus.
In summary, the clinical keratoconus corneal epithelial thickening was unique and typical crater shape, and the thickening was obvious in the nasal inferior area. The phenomenon of the thinnest point thinning in forme fruste keratoconus corneal epithelium appeared earlier than the corneal epithelial remodeling. Central island shape of corneal epithelial topography can be found in patients with high ΔK, which subsequently can be used to differentiate early keratoconus from high astigmatism.
ACKNOWLEDGEMENTS
Authors’ contributions:Zhang XF conceived and designed the study; Zhang XF, Yang XL, Wang Y, Luo BG and Xu Y were involved in data collection; Yang XL and Wang Y did statistical analyzed; Zhang XF, Yang XL and Wang Y interpreted of the data; Zhang XF and Yang XL drafted the manuscript; Zhang XF, Yang XL, Wang Y, Luo BG and Xu Y reviewed and approved the manuscript.
Conflicts of Interest: Yang XL,None;Wang Y,None;Luo BG,None;Xu Y,None;Zhang XF,None.
 International Journal of Ophthalmology2021年1期
International Journal of Ophthalmology2021年1期
- International Journal of Ophthalmology的其它文章
- Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid
- Preliminary studies of constructing a tissue-engineered lamellar corneal graft by culturing mesenchymal stem cells onto decellularized corneal matrix
- Therapeutic potential of Rho-associated kinase inhibitor Y27632 in corneal endothelial dysfunction: an in vitro and in vivo study
- Changes of matrix metalloproteinases in the stroma after corneal cross-linking in rabbits
- A multi-omics study on cutaneous and uveal melanoma
- Eあects of quercetin on diabetic retinopathy and its association with NLRP3 inflammasome and autophagy
