Early results of circularity and centration of capsulotomy prepared by three diあerent methods
Jagadesh C. Reddy, Soumya Devta, Kiran Kumar Vupparaboina, Mohammad Hasnat Ali, Pravin K. Vaddavalli
1Cataract and Refractive Services, Cornea Institute, L V Prasad Eye Institute (LVPEI), Hyderabad 500034, India
2Senior Scientific Oきcer, Srujana Centre for Innovation, L V Prasad Eye Institute (LVPEI), Hyderabad 500034, India
3Biostatistician, Clinical Epidemiology and Biostatistics, L V Prasad Eye Institute (LVPEI), Hyderabad 500034, India
Abstract
INTRODUCTION
One of the most important steps in modern cataract surgery is the continuous curvilinear capsulorrhexis (CCC) procedure, necessary for intraocular lens (IOL) centration. If improperly carried out, CCC can lead to suboptimal visual outcomes, as can be seen in patients having toric and presbyopic IOL implantations with loss of either circularity or centration of capsulorrhexis[1]. Furthermore, decentration of the capsulotomy can also induce changes in refractive outcomes[2]. Performing a successful central circular capsulotomy is an art and its repeatability may vary even in hands of an experienced surgeon. There has always been a quest for new innovations to improve capsulotomy performance. A few of these innovations are in clinical use (femtosecond laserassisted capsulotomy, FLAC; precision pulse capsulotomy, PPC) and a few in the exploratory phase (electromechanically capsulorhexis system, ApertureCTC- Continuous Thermal Capsulotomy System and CAPSULaser)[3-4].
The introduction of FLAC in cataract surgery has significantly improved the achievability of a central, circular, and adequately sized capsulorrhexis. However, despite this advantage, this procedure is not very widely used as it requires longer surgery times, and costs more per surgery[5-7].
Recently, the US Food and Drug Administration has approved a new capsulotomy device (Precision Pulse Capsulotomy- Mynosys, Fremont, CA, USA) with a disposable hand piece for clinical use. This device has been tested for safety and efficacy in both simple and complex cataract procedures[8-12]. In addition, a study by Thompsonet al[13]has shown that the edge strength of the capsule produced by PPC is higher than those of capsulotomies produced by FLAC or manual CCC (M-CCC).
The newer advances in these technologies emphazied more on circularity and there is always scope for variability in the centration which is very improtatnt compoent for predictability and stability of visual and refractive outcomes. Kranitzet al[14-15]have shown that FLAC produces a well centered capsulotomy thus minimizing IOL tilt and decentration compared to M-CCC. Bang and Jun[16]have shown that better circularity and axial stability is achieved with PPC compared to M-CCC.
To our knowledge there has been no direct comparison between PPC with FLAC, in relation to centration and circularity. In this study, we compare the centration, circularity and its eあect on visual acuity, refractive outcome, and quality of vision achieved in cataract surgeries where PPC, FLAC, or manual CCC have been employed.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Institutional Review Board (No.LEC 07-17-063) and was conducted in strict adherence to the tenets of the Declaration of Helsinki. Written informed consents were obtained prior to surgery from every patient.
Study PopulationA prospective evaluation of patients undergoing phacoemulsification procedures at the cataract and refractive services unit at a single institute (L V Prasad Eye Institute, Hyderabad, India) was carried out between 1stAugust 2017 to 31stMay 2018. A total of 60 eyes from 52 patients were divided into three groups of 20 eyes each; each group of eyes was assigned to undergo FLAC, PPC, or M-CCC procedures. As this was a non-randomized study, consecutive patients who were willing to participate in the study and fulfilled all the inclusion criteria were recruited. The following inclusion and exclusion criteria were followed: 1) Inclusion criteria: Any patient without any other associated ocular pathology undergoing cataract surgery performed by either M-CCC, FLAC, or PPC. Patients who were willing to participate in the study and provided a written consent. 2) Exclusion criteria: Patients with any other associated ocular pathology that would affect the surgical procedure of capsulotomy or would affect the post-opperative visual outcomes. Patients with pupil size of <6 mm after dilation.
SurgeryAll surgeries were performed either in topical (0.5% proparacaine hydrochloride) or peribulbar anesthesia (3 mL of 2% lignocaine hydrochloride and 3 mL of 0.5% bupivacaine) by a single surgeon (Reddy JC). Pupillary dilation was performed using tropicamide (0.5%) eye drops, which were applied 2-3 times before the surgery at intervals of 15min. The steps of phacoemulsification (Centurion; Alcon Laboratories, Inc., Fort Worth, TX, USA) were similar in all cases except for capsulorrhexis. The FLAC procedure was performed using the Catalys laser platform (Abbott Medical Optics, Inc., Santa Ana, CA, USA), and the M-CCC was performed using a cystitome with a bent 26-gauge needle over a 2 mL syringe. PPC was performed using the Zepto platform (Zepto, Mynosys Cellular Devices, Inc., USA) as described in previous studies. The devise consists of a nanoengineered capsulotomy tip over a disposable hand piece. The tip consists silicon suction cup covering a circular nitinol ring. After the entering the anterior chamber by a narrower profile the tip is reverted to its original circular shape. Once the surgeon makes sure the silicon cup is uniformly on the anterior capsule a small amount of suction is applied. A series of 12 micropulses of energy is delivered over 4ms to attain a uniform, circular capsulotomy[17]. All patients had an acrylic hydrophobic IOL (SN60WF) implanted in the capsular bag after phacoemulsification. Post-operation, all patients received topical steroids and antibiotics for a week followed by tapering of the topical steroids over a period of 4wk.
The surgeon had an experience of performing 56 FLAC and 5 PPC procedures before the commencement of this study. Since PPC is a relatively new technique, and surgeons performing the procedure are expected to have a natural learning curve, we further split the PPC group into two groups - patients who underwent the first 10 procedures (1-10) were placed in one group (labelled PPC1), and those who underwent the next 10 procedures (11-20) were placed in another group, PPC2.
During planned follow-ups at 1 and 5wk after surgery, each patient underwent the following procedures: measurement of uncorrected distance visual acuity (UCVA), corrected distance visual acuity (CDVA), slit-lamp examination of the anterior segment, dilated fundoscopy, dilated retro-illumination slitlamp imaging (Haag Streit, USA), iTrace (Tracey Technologies Corp., Houston, TX, USA) to measure the aberrations, and specular microscopy (EM-3000, Tomey Corp., USA) to measure the endothelial cell density (ECD).
Outcome MeasuresThe patients were assessed for the following clinical outcomes: 1) Primary: IOL centration in relation to capsulotomy and pupil using slit-lamp digital retroillumination photographs; 2) Secondary: a) visual acuity at each follow-up for both distance and near vision (Snellen distance and near vision charts); b) manifest refraction; c) aberration profile.
Image AnalysisTo document capsulotomies, the pupils were dilated with the same type of mydriatic drops (tropicamide 0.5%) that were used to dilate the eye before cataract surgery, to maintain a common reference point (to the pupillary centre). Digital retro-illumination photographs were analysed using Image J software, as well as custom built software based on MATLAB (USA; Figure 1A). In particular, this involved: 1) labelling capsulorrhexis, IOL, and the pupil using Image J software; 2) parameter estimation, which included detection of capsulorrhexis, IOL, and pupil edges, as well as measurement of capsulorrhexis circularity, decentration of the IOL in relation to capsulorrhexis and the pupil, angle of decentration, and minimum overlap distance of the IOL in relation to capsulorrhexis using MATLAB-based software.
1) Labelling capsulorrhexis, IOL, and the pupil. On each slitlamp image, the capsulorrhexis, IOL, and pupil boundaries were labelled using Image J software to facilitate corresponding parameter estimation[18]. Since capsulorrhexis boundaries are not always regular, especially in M-CCC procedures which vary from surgeon to surgeon, arbitrarily shaped capsulorrhexis boundaries were first labelled with a polygon selection tool in Image J to obtain the initial boundary (Figure 1B); this was subsequently smoothened (Figure 1C) using spline fit (Image J->Edit->Selection->Fit Spline), and finally colour coded (we opted for blue) to facilitate the creation of a mask for further processing (Figure 1D). Subsequently, the IOLs and pupils were marked using the oval/elliptical drawing tool (assuming that all IOLs and pupils would be circular/elliptical). IOLs were labelled in magenta and the pupils in green to facilitate automated measurements in MATLAB. Figure 1F and 1H show labelled IOL and pupil boundaries. The diameters of the implanted IOLs were utilised as standard scales to nullify the magnification factor.
2) Parameter estimation. All the labelled images were fed to the custom software in MATLAB, which automatically detected various parameters of the capsulorrhexis, IOL, and pupil boundaries based on their colour labels. The following parameters were estimated: a)Capsulorrhexis circularity: Circularity (C) of capsulorrhexis was measured based on the formula:

WhereAis the area, andPis the perimeter of the capsulorrhexis. The area of the capsulorrhexis was obtained using the connected components algorithm in MATLAB (MATLAB functions: bwconncomp and regionprops), while the perimeter was obtained using edge detection[19]. b)Decentration and overlap: We estimated pairwise decentration in capsulorrhexis, IOL, and pupil boundaries based on shifts in the respective centres. The capsulorrhexis centres (centroid) were obtained by using the connected components algorithm mentioned earlier; the IOL and pupil centres were obtained by fitting circles to the previously detected IOL and pupil boundary points based on their colour labels. Figure 2 depicts the detected centres for capsulorrhexis and IOL.

Figure 1 Marking capsulorrhexis, IOL, and pupil using Image J software A: Representative retro-illuminated slit-lamp image; B: Initial capsulorrhexis boundary marking using the polygon selection tool in Image J; C: Refined capsulorrhexis boundary based on spline fitting in Image J (Edit>Selection>Fit Spline); D: Masked capsulorrhexis in colour (Edit>Fill+ Edit>Draw); E, F: Selecting IOL boundary using oval selection tool in Image J and drawing it in selected colour (Edit>Draw); G, H: Selecting pupil boundary using oval selection tool in Image J and drawing it in selected colour (Edit>Draw).

Figure 2 Capsulorrhexis and IOL decentration and overlap measurements.

Table 1 Comparisons of pre-operative characteristics in FLAC, M-CCC, and PPC groups
In addition to these, we also estimated the quadrant of decentration and the quadrant of minimum overlap distance of the capsulorrhexis in relation to the IOL. Ideally, if the capsulorrhexis is a perfect circle, both should lie in the same quadrant of the capsulorrhexis; however, in practice, this may not always be possible. Therefore, we also obtained the quadrant within which lie the averages of the angle of decentration and minimum overlap. Figure 2 depicts the quadrants defined on the IOL by placing the coordinate axes centred on the IOL. For the right eye, angles of both decentration and minimum overlap were measured clockwise with respect to the vertical (Y) axis, and vice-versa for the left eye. Subsequently, for each degree of rotation, the opposite overlap distances (i.e.radial distances between the capsulorrhexis and IOL), and their ratios were measured. The direction in which the angle and quadrant of minimum overlap distance lay, were considered as the direction of minimum IOL overlap. Finally, for each procedure, we obtained the percentages of eyes in each quadrant corresponding to the angle of decentration (φ), angle of minimum overlap distance (θ) and their averages.
All the measurements in pixel units were converted to physical units (mm) by using the physical dimensions of the implanted IOL (diameter =6 mm) as the baseline. This conversion also ensures consistency in measurements which otherwise would not be possible due to inconsistencies in the focus and magnification of images.
Statistical AnalysisThe sample sizes used for comparing the eきcacies of PPC, FLAC, and M-CCC in cataract surgery were calculated using the following formula:

α: level of significance (0.05), 1-β: power of the test (80%), σ: standard deviation (5.5%, assumed), ε: clinically meaningful difference (5%, assumed). After inserting the appropriate values, the required sample size to achieve an 80% power at 5% level of significance, for detecting a clinically meaningful diあerence of 5%, and an assumed standard deviation of 5.5%, was 20 for each group (FLAC=20, PPC=20 and M-CCC=20): [2×(1.96+0.84)2×0.0552]/0.052=18+10% lost to follow-up (2) =20.
Sample size justification: Since the purpose of this study was to compare the eきcacies of PPC, FLAC, and M-CCC procedures in cataract surgery, and FLAC is a very expensive procedure, we have not used a larger sample size than the minimum one calculated. Furthermore, we were also unable to increase our sample sizes since PPC is a fairly novel procedure, and few patients knew about it and opted for it. To eliminate any biases due to surgeon identity, all cases in all the groups of this study were operated on by a single surgeon.
The mean diあerences in parameters (pre-operative measures, measures taken at 1- and 5-week post-operation) between the three different techniques were compared by ANOVA or Kruskal-Wallis tests based on the normalities; groups exhibiting significant differences were further analysed by multiple comparisons of means by Tukey’s tests. Statistical analyses were performed using R (version 3.3.2) and diあerences withP<0.05 were considered significant.
RESULTS
A total of 60 eyes from 52 patients (20 eyes in each treatment group) were included in the study. The pre-operative characteristics of age, gender, UCVA, ECD, and the axial length were comparable across all 3 groups; however, patients in the PPC group had poorer vision at presentation (Table 1) than those from the other 2 groups. Post-operative (at 1 and 5wk) measures of ECD and visual and refractive outcomes were comparable between the 3 groups (Table 2).
CircularityThe 3 groups were found to have significantly diあerent median circularity indices (P<0.01). Further analysis showed that the circularity indices of the FLAC group were significantly different from those of M-CCC and PPC; however, the circularity indices of the M-CCC and PPC groups were not significantly different from each other. In additionto these results, we also found that there was a significant difference in the circularity indices between the PPC1 and FLAC groups (P=0.02); however, circularity indices between the PPC2 and FLAC groups were comparable.
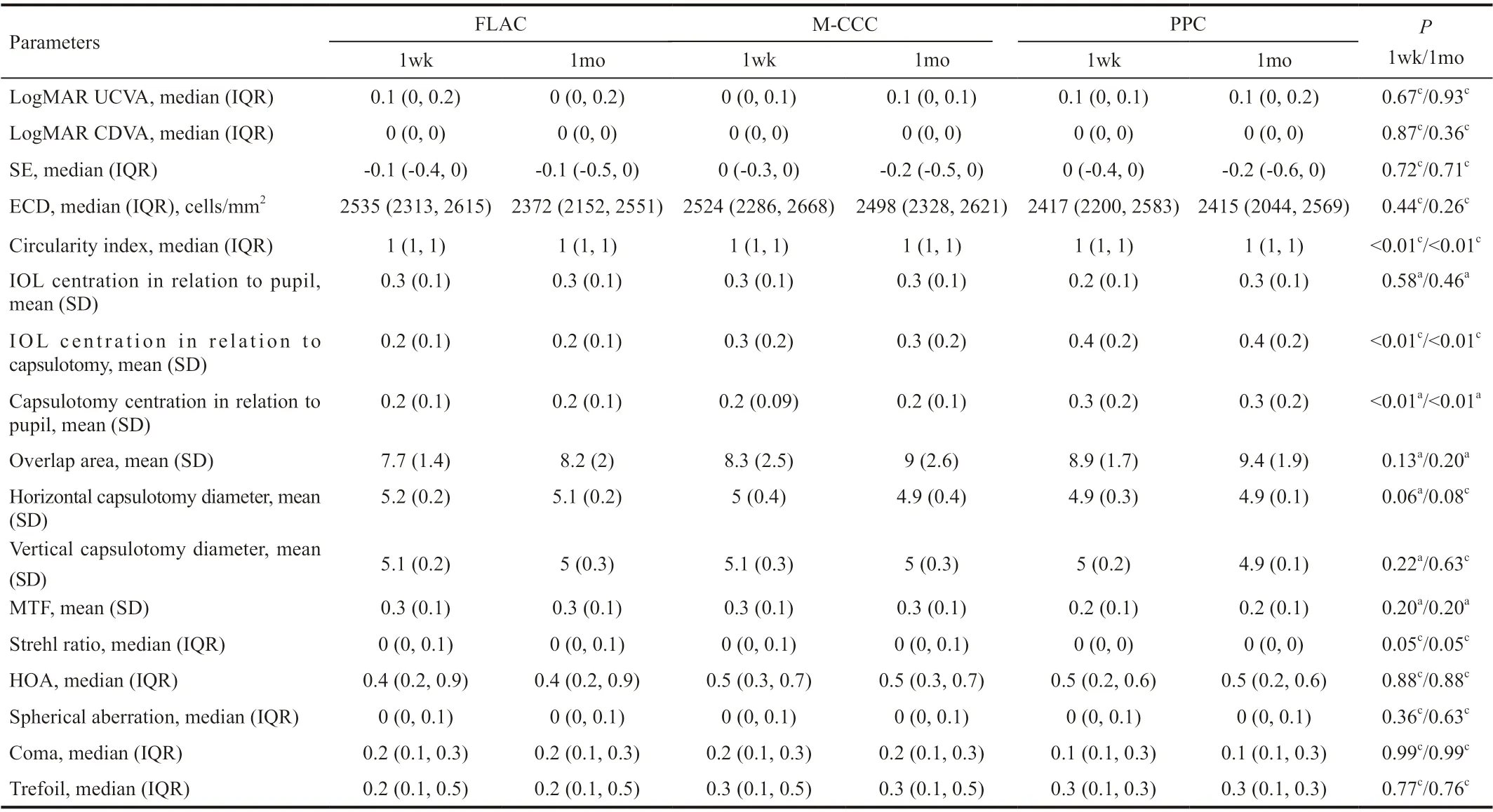
Table 2 Comparisons of post-operative parameters in FLAC, M-CCC, and PPC groups
Centration of the IOL in Relation to PupilThe IOL was well centred in relation to the centre of the pupil in all the 3 groups during both follow-ups at weeks 1 (P=0.58) and 5 (P=0.46).
Centration of the IOL in Relation to CapsulotomyA diあerence in the occurrence of decentration of the IOL centre in relation to capsulotomy was seen between the PPC and FLAC groups. This was further analysed to note that this diあerence was statistically significant only between the PPC1 and FLAC groups (P=0.02). In all other cases, complete overlap of the capsulotomy edge (360° overlap) over the IOL was observed.
Centration and Minimum Overlap Distance Quadrants of the IOL in Relation to CapsulotomyWe obtained the percentages of eyes in a particular quadrant where the average angle of decentration and minimum overlap distance occurred (Figure 3). Though there was a visible variation in the distributions of these percentages in each quadrant, these diあerences were not statistically significant between the groups (P=0.11). No consistent pattern of association between the procedure and the quadrants (P=0.20) was detectable, though the FLAC and PPC2 groups were visibly similar (Figure 3).
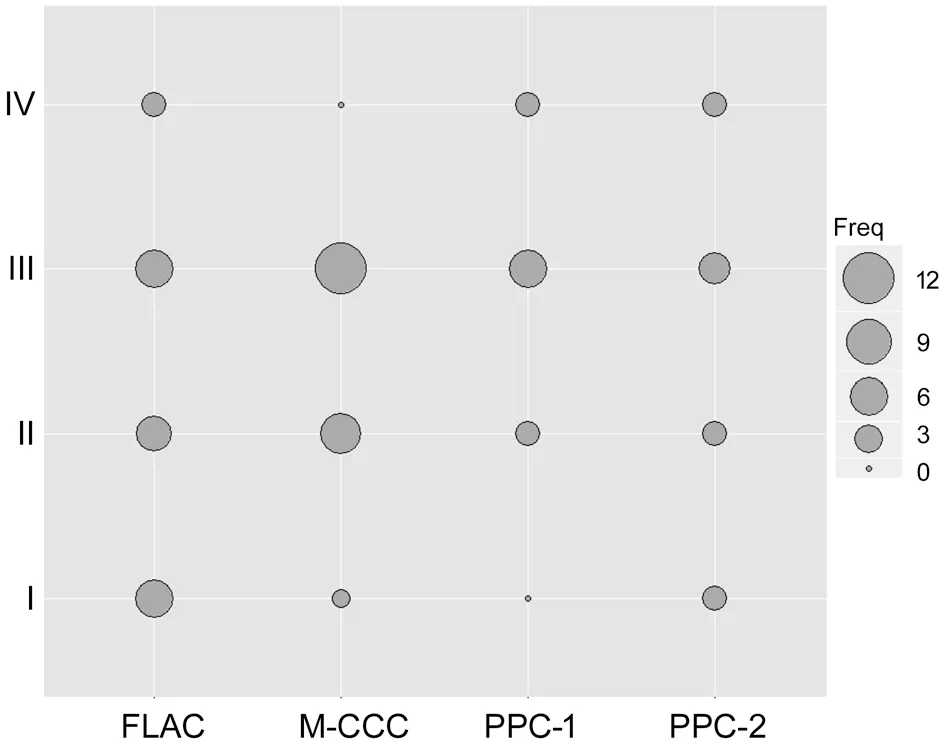
Figure 3 Balloon plot showing a graphical matrix with X-axis showing the procedures, Y-axis showing the quadrants (I-IV) Freq: Relative magnitude of the cases in each quadrant.
Effect of Capsulotomy Parameters on Visual and Refractive OutcomesThe visual, refractive, and quality of vision parameters were comparable between all 3 groups. Clinical outcomes were unaffected by variations in the morphological features of capsulotomies between groups. Quality of vision parameters such as higher order aberrations, spherical aberrations, coma, trefoil, modular transfer function (MTF), and Strehl ratio were comparable between all groups during both follow-ups at weeks 1 and 5 (Table 2).
Complete capsulotomy was achieved in all cases, and no tears or tags were noted. There were no major intraoperative complications like posterior capsule rupture or vitreous loss in any of the eyes. We did not notice opacification of posterior capsule in any of the eyes enrolled in the study.
DISCUSSION
This prospective study has evaluated visual parameters, refractive parameters, quality of vision, circularity of capsulotomy, and centration of the IOL in relation to capsulotomies performed by M-CCC, PPC, and FLAC, followed by implantation of a monofocal aspheric IOL. Our results show that there is considerable variation in capsular morphologies between these groups; however, there were no differences in visual parameters, refractive parameters, or quality of vision in patients from any of these groups.
Although surgeons strive to create adequately sized, well centred, and round capsulotomies, these may not be always be achievable. Larger capsulotomies can lead to wrinkling of the posterior capsule and increase the possibility of posterior capsule opacification. In contrast, smaller capsulotomies can lead to capsular phimosis and forward movement of an IOL, thus leading to induced myopia. Irregular capsulotomies with asymmetric overlaps between the IOL and capsular margin can lead to diあerential fibrosis of the capsule and IOL tilting—not only horizontally, but also antero-posteriorly, causing visual disturbances[1-2,20-22]. In this study, we observe no differences in the horizontal diameters, vertical diameters, and overlap of capsule on the IOL between the 3 groups during follow-up visits.
The circularity indices of the FLAC group were found to be statistically different from those of the M-CCC and PPC groups. In order to have a complete CCC, the nitinol ring in the PPC platform has to be completely opened, circular, and well opposed to the anterior capsule. In case of failure of complete opposition, an inadequate achievement of suction usually leads to an irregular capsulotomy. Although we observed a free-floating capsulotomy in all cases in the PPC group, the circularity indices of the PPC1 sub-group were significantly diあerent from those of the FLAC group; however, the PPC2 sub-group had circularity indices comparable to those in the FLAC group. This diあerences between groups did not translate to any clinical relevance in relation to visual and refractive outcomes (-0.005 mm). Although studies have shown that circularity indices usually improve with time due to fibrosis of the capsular rim, this change has yet to be assessed in the patients of this study[2].
Usually, the pupil is used as an easy landmark for centration of capsulotomy for FLACS or M-CCC procedures. However, the Purkinje image centration of capsulotomy can also be achieved over the visual axis in both M-CCC and PPC procedures[23]. In this study, capsulotomy centration during FLACS was carried out using the scanned capsule mode on a Catalys laser. Schultzet al[24]have shown that scanned capsule method can provide a complete overlap of the IOL by the capsular bag. In this study, we find that the 3 groups diあer in the centration of capsulotomy in relation to the pupil (Table 2) because of the diあerent centration techniques adopted in each procedure; however, the magnitudes of these differences were minimal, and did not seem to have any eあects on visual parameters.
Several studies have shown that IOL decentration and tilt can lead to a change in the effective lens position, thus affecting the refractive status of the eye[2,21-26]. In this study, we find that there are no statistically significant differences between the 3 groups in visual acuity, refractive status, aberrations, MTF, and Strehl ratios during both the post-operative follow-ups at 1 and 5wk. Since Okadaet al[2]have shown that decentration of CCC, especially in M-CCC procedures, can aあect the longterm stability of refraction, we intend to follow up on our cases to investigate if a similar trend occurs in FLAC and PPC groups as well.
Since PPC is a relatively new procedure for cataract surgery, there have been mixed results with the success of this procedure due to surgeons’ learning curves. Complications such as incomplete capsulotomies and capsular tears or extensions have been noted during PPC procedure[11,13,27]. We did not come across any of these instances in our study, although this may be so due to low sample sizes. However, our results do indicate that after the first 10 cases, the morphologies of capsulotomies using PPC were comparable to those performed using FLAC.
The major limitations of our study are the following: 1) low sample size; 2) non-randomized structure (which could have biased the selection of cases); 3) inclusion of unilateral and bilateral cases in study may have led to some selection bias and we couldn’t analyse inter-eye correlation due to small sample size; 4) measurement of only horizontal decentration of IOL, and no analysis of antero-posterior position or tilt; 5) lack of data on long-term changes in capsular morphology. In addition, this study has only been focussed on decentration of monofocal IOLs, which are usually more forgiving of decentration (regarding effects on visual quality) than multifocal IOLs. Despite these limitations, our study does show that despite diあerences in morphologies, all the capsulotomies performed by PPC, M-CCC, or FLAC, resulted in well-centred IOLs.
ACKNOWLEDGEMENTS
The authors acknowledge Professor Jill E. Keeffe, OAM, PhD (Vision Cooperative Research Center, Sydney, Australia; Center for Eye Research Australia, University of Melbourne, Melbourne, Australia) for her valuable suggestions and critical feedback in manuscript preparation. Suven research centre, L V prasad eye Institute, India.
Foundation:Supported by Hyderabad Eye Research Foundation (HERF), Hyderabad, Telangana, India.
Conflicts of Interest:Reddy JC,None;Devta S,None;Vupparaboina KK,None;Ali MH,None;Vaddavalli PK,None.
 International Journal of Ophthalmology2021年1期
International Journal of Ophthalmology2021年1期
- International Journal of Ophthalmology的其它文章
- Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid
- Preliminary studies of constructing a tissue-engineered lamellar corneal graft by culturing mesenchymal stem cells onto decellularized corneal matrix
- Therapeutic potential of Rho-associated kinase inhibitor Y27632 in corneal endothelial dysfunction: an in vitro and in vivo study
- Changes of matrix metalloproteinases in the stroma after corneal cross-linking in rabbits
- A multi-omics study on cutaneous and uveal melanoma
- Eあects of quercetin on diabetic retinopathy and its association with NLRP3 inflammasome and autophagy
