How to use the 12-lead ECG to predict the site of origin of idiopathic ventricular arrhythmias
Lesson Ninety-six
Anatomical considerations
When the heart is viewed in an attitudinal1perspective,the right cardiac chambers are anterior relative to the left chambers.The right ventricle(RV)is positioned anteriorly and to the right of the left ventricle(LV).The LV lies obliquely in the chest,with the base located posteriorly and the apex positioned to the left.The so-called anterior interventricular sulcus in fact begins superiorly and travels to the left and slightly anteriorly,while the so-called posterior interventricular sulcus is actually positioned inferiorly.
Regarding the outflow tract region,the anatomical relationships are complex and ventricular arrhythmias(VAs)from different structures in this region may have a similar ECG appearance.The RV outflow tract(RVOT)wraps around and crosses the LV outflow tract(LVOT)anteriorly,so that the pulmonary valve lies anterior and to the left of the aortic valve(AoV).This relation is important,as the anterior aspect of the RVOT is actually the most leftward and highest outflow tract structure.
The LVOT corresponds to the elliptical opening of the LV,also termed the LV ostium by McAlpine.This is composed by the aortic root anteriorly and by the mitral annulus posteriorly and to the left.Both valves are anatomically coupled through a band of fibrous tissue known as the aortomitral continuity(AMC),which extends between the anterior leaflet of the mitral valve(MV)and the left(LCC)and noncoronary cusp(NCC)of the AoV.The AoV occupies a central position within the heart and is composed of 3 cusps,each one with relevant anatomical relationships.In attitudinal orientation,the right coronary cusp(RCC)is the most anterior cusp relative to the sternum,the NCC is posterior and rightward,and the LCC is posterior and leftward.The NCC is the most inferior and the LCC is the most superior in position.The RCC is in close proximity to the posteroseptal aspect of the RVOT,while the LCC is adjacent to the anterior aspect of the LV ostium,in close proximity to the left anterior descending coronary artery.Conversely,the NCC is in relationship with both the left atrium and the right atrium separated by the interatrial septum.Below the commissure between the RCC and the NCC lies the membranous ventricular septum,where the penetrating bundle of His is located.
ECG features
Several ECG features are relevant for the localization of a particular ventricular arrhythmias(VAs).The most important are(1)QRS axis,(2)bundle branch block pattern,(3)precordial transition,and(4)QRS width.
The QRS axis has both a vertical(superiorinferior)and a horizontal(right-left)dimension.The vertical dimension is reflected by QRS polarity in bipolar leadsⅡandⅢ.For example,all outflow tract VAs share an inferiorly directed QRS axis,with positive forces in leadsⅡandⅢ.The horizontal dimension is better reflected by leadⅠ.Structures closer to the left arm will produce a deeply negative complex in leadⅠ(rightward axis);conversely,structures closer to the right arm are strongly positive in leadⅠ(leftward axis).Additional approximation to the horizontal dimension is given by the relative amplitude between limb leads aVR and aVL:a more positive polarity in lead aVR than in lead aVL suggests a more leftward origin;a more positive polarity in lead aVL than in lead aVR points toward a more rightward origin.
The bundle branch block pattern is related to the sequence of RV and LV activation.VAs with a right bundle branch block(RBBB)appearance typically arise in the LV,while VAs with a left bundle branch block(LBBB)appearance may arise anywhere in the RV,but also in the left side of the interventricular septum.
The precordial transition in RBBB VAs(first lead with a predominant S wave)occurs progressively earlier as the site of origin moves from the base toward the apex of the LV.In LBBB VAs,the precordial transition(first lead with a predominant R wave)occurs progressively later as the site of origin moves from the septum toward the RV free wall.Positive concordance(all positive precordial leads)is seen in VAs arising at the base of the heart,in which case ventricular activation has to move anterior and apical.Conversely,negative concordance(all negative precordial leads)is seen in VAs originating near the apex,such that electrical activity moves away from the chest wall.
Finally,septal VAs have narrower QRS durations than do VAs originating on the free wall of both ventricles because of synchronous rather than sequential ventricular activation.
Comprehensive anatomic approach for the prediction of the site of origin
Step 1
We start looking at the superior/inferior axis,represented by polarity in leadsⅡandⅢ.Inferior-axis VAs(positive QRS complex in leadsⅡandⅢ)arise from basal areas of the heart,including the outflow tracts and the superior aspect of the atrioventricular valves,while superior-axis VAs(negative QRS complex in leadsⅡandⅢ)have their origin at the inferior aspect of both ventricles.
Step 2
Our next step is to separate VAs arising from the right or left side of the chest midline,which does not necessarily mean RV vs LV,especially in the outflow tracts,where there is a significant overlap between the RVOT and the LVOT.
1.For outflow tract VAs,the best single ECG discriminator is the left/right axis reflected by leadⅠ.Rightward structures,such as the posterior aspect of the RVOT,RCC,para-Hisian region,and superior aspect of the tricuspid valve(TV),are positive in leadⅠ,while leftward structures,such as the anterior aspect of the RVOT,LCC,AMC,anterolateral MV annulus,and LV summit,will produce a negative complex in leadⅠ.The commissure between the RCC and the LCC,a common source of idiopathic VAs,is close to the midline,and,in our experience,arrhythmias from this area may have either a positive,a negative,or a biphasic QRS complex in leadⅠ.
2.For VAs arising from the inferior aspect of the ventricles,the most helpful element is the bundle branch block appearance,as some VAs from the septal portion of the LV may exhibit a left axis.VAs with a superior axis and LBBB appearance may arise from RV structures(inferior aspect of the TV or moderator band[MB])or the cardiac crux.Conversely,VAs with a superior axis and RBBB pattern arise from LV structures(inferior aspect of the MV,posteromedial papillary muscle[PPM],or left posterior fascicle).
Step 3
Once we circumscribe the likely site of origin to 1 of these 4 quadrants,a more refined localization relies in other characteristics such as precordial transition,QRS width,or QRS morphology in specific leads.
Right upper quadrant
It includes the posterior aspect of the RVOT,RCC,superior TV and para-Hisian region(Figures 1A-1E).Outflow tract VAs,in general,can be differentiated from TV and para-Hisian VAs by looking at lead aVL polarity.Lead aVL is a left sided but also a superior lead;thus,the majority of outflow tract VAs show negative deflections in lead aVL(QS waves)as well as in lead aVR.Conversely,TV and para-Hisian Vas are located more inferiorly and rightward in the chest and,therefore,usually exhibit positive deflections in lead aVL(any R or r waves).In addition,RVOT and RCC VAs show a strong inferior axis,with tall R waves in leadsⅡandⅢ.In VAs from the superior TV and para-Hisian region,positive forces are less pronounced,especially in leadⅢ,which can be even isoelectric or negative.Finally,a narrow QRS duration(usually<130 ms)is typical of para-Hisian VAs given the early engagement of this His-Purkinje system.
Left upper quadrant
It includes the anterior aspect of the RVOT and most LVOT structures(excluding the RCC)(Figures 1F-1L).The precordial transition is likely the most helpful characteristic to pay attention in this group.As we move progressively more posterior from the RVOT free wall to the lateral mitral annulus,the precordial transition occurs progressively earlier(lead V4or V5for the RVOT free wall,lead V3or V4for the RVOT septum,lead V1or V2for the LCC)and finally transforms from an LBBB to an RBBB configuration at the AMC or the top of the MV.In addition to the bundle branch block pattern,some specific characteristics of lead V1may orientate to certain locations:RVOT and RCC VAs typically exhibit a QS pattern in lead V1;a QS pattern with notching in downstroke is suggestive of VAs from the RCC/LCC commissure;LCC VAs often have a multiphasic pattern in lead V1(M or W pattern);a qR pattern in lead V1is often seen in VAs from the AMC;and VAs from the anterolateral MV annulus most often have an R pattern in lead V1with positive precordial concordance.
Right lower quadrant
The most common sources of idiopathic VAs in this quadrant are the inferior TV annulus,the MB,and the cardiac crux(Figures 2A-2C).The MB is a prominent muscular trabeculation that crosses from the septum to the free wall of the RV and provides support to the anterior papillary muscle of the TV.The crux of the heart is an epicardial region near the junction of the middle cardiac vein and the coronary sinus.MB VAs typically have a left superior axis and late precordial transition(later than lead V4).Conversely,crux VAs also have a left superior axis,but with early transition(lead V2)and a QS pattern in inferior leads.They may also present features suggesting an epicardial access,such a pseudo delta wave or maximum deflection index>0.55.TV VAs have a variable precordial transition(leads V2through V5)depending on their septal or lateral origin(lead V2or V3for septal sites and lead V4or V5for free wall sites).A QS pattern in lead V1is recorded in the majority of VAs arising from the septal portion of the TV annulus,while most VAs from the free wall portion exhibit an rS pattern in lead V1.
Left lower quadrant
Idiopathic VAs with RBBB and superior axis may arise from the inferior MV annulus,the left posterior fascicle,and the PPM(Figures 2D-2F).These can be differentiated on the basis of 3 main characteristics:precordial transition,QRS duration,and V1morphology.Positive precordial concordance(R>S in lead V6)is relatively specific of MV VAs,reflecting their more basal location.Conversely,VAs from the left posterior fascicle and PPM usually have R<S by lead V5.A QRS duration of<130 ms is highly suggestive of fascicular VAs,reflecting the more rapid ventricular depolarization via the Purkinje system.For the same reason,fascicular VAs typically have an rsR′(r<R′)pattern in lead V1,mimicking typical RBBB.In comparison,PPM and MV VAs usually have an Rsr′(R>r′),R,or qR pattern in lead V1.
Inferior lead discordance
Inferior lead discordance reflects an opposite depolarization vector along bipolar limb leadsⅡ(from the left leg to the right arm)andⅢ(from the left leg to the left arm).This is most often observed in VAs originating from midcavitary structures(interventricular septum,MB,and APM)and sometimes from the lateral aspect of the atrioventricular valves(Figures 2G-2H).Positive/negative discordance(positiveⅡ/negativeⅢ)is equivalent to a frontal axis of-30° to+30°,and negative/positive discordance(negativeⅡ/positiveⅢ)is equivalent to a frontal axis of+150°to+210°.In particular,the likely sites of origin are as follows:
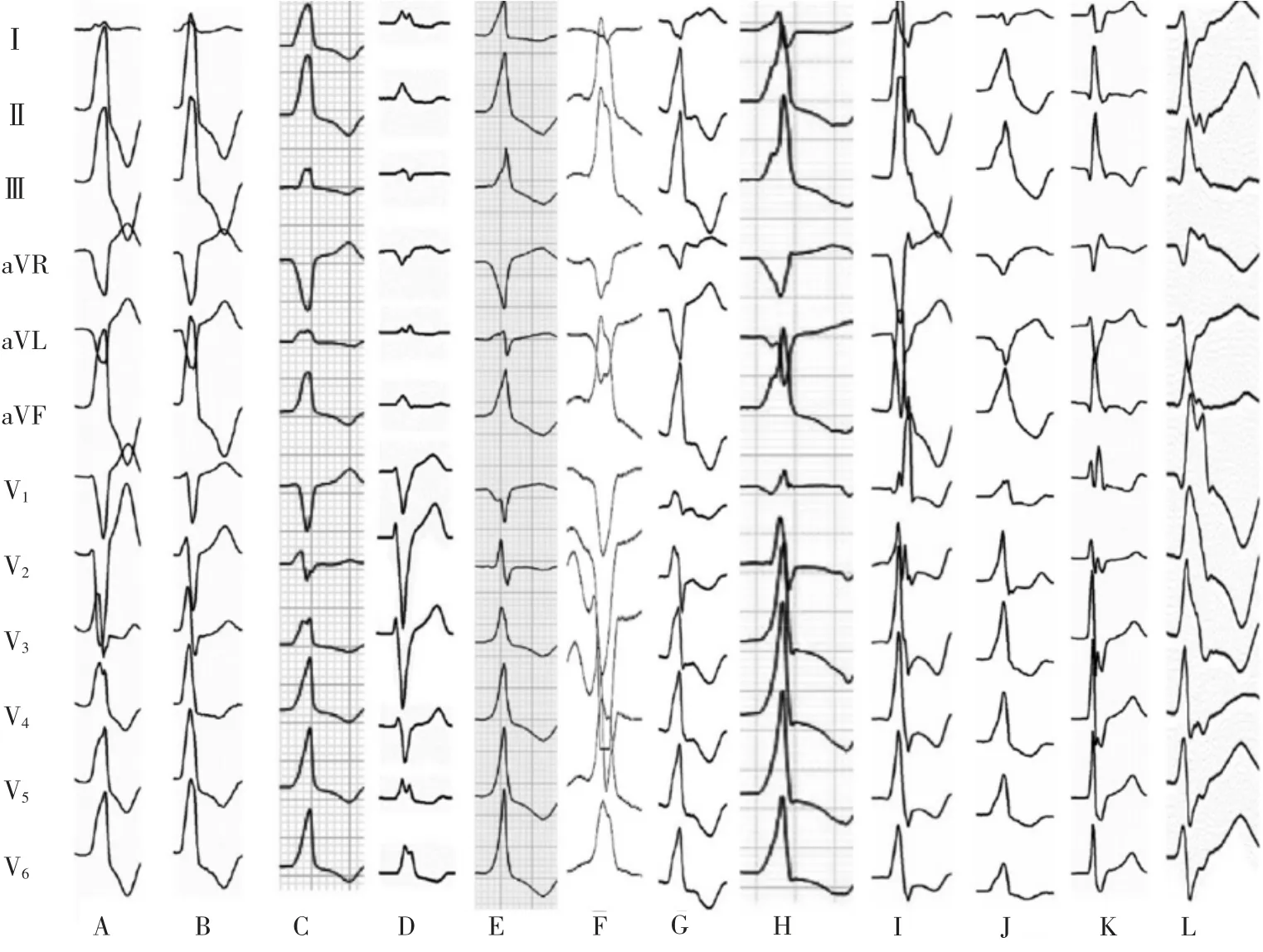
Figure 1 Inferior-axis VAs with origin at the(A)posterior RVOT(septal wall),(B)RCC,(C)para-Hisian region,(D)superior TV,(E)RCC-LCC commissure,(F)anterior RVOT,(G)LCC,(H)AMC,(I)anterolateral MV,(J)LV summit,(K)left anterior fascicle,and(L)anterolateral papillary muscle.

Figure 2 Superior-axis VAs with origin at the(A)inferior TV,(B)moderator band,(C)cardiac crux,(D)inferior MV,(E)left posterior fascicle,and(F)posteromedial papillary muscle.Two examples of VAs with inferior lead discordance ablated from the(G)moderator band and(H)anterolateral papillary muscle.
1.Positive/negative discordance:RV structures,including the lateral TV,MB,and interventricular septum(para-Hisian region).All these have an LBBB configuration.
2.Negative/positive discordance:LV structures,including the lateral MV and APM.These have an RBBB configuration.
词 汇
obliquely adv.倾斜地
sulcus n.纵沟;回间沟
elliptical adj.椭圆的,隐晦的
aortomitral adj.主动脉二尖瓣的
commissure n.合缝处,缝口,接合点(缘,处)
approximation n.近似值,粗略估算,类似事物
discriminator n.辨别者,鉴别器
circumscribe v.限制,约束(自由、权利、权力等),画…的外接圆
quadrant n.四分之一圆,象限;象限仪,四分仪
midcavitary n.中腔,腔中间
注 释1.Attitudinal一词通常译为表示人的主观意识的表现状态,即“态度的,姿态的”,医学文献中有时用作表示客观的身体体态,特别在描述心脏解剖时强调的是原位。本文中两处出现该词,其一为“attitudinal perspective”,译为“体态视角”,其二为“attitudinal orientation”,译为“体态方向”,强调的是心脏原位的视角和方向。例如“From the nonattitudinal perspective,the anterior pulmonic cusp is the most anterior cusp;however,when viewed from an attitudinal perspective,the right pulmonic cusp is equally anterior relative to the chest wall.”。译为“从非体态视角看,前肺窦尖是最靠前的窦尖,然而,从体态视角看,相对胸壁而言,右肺窦尖一样靠前”。
参考译文
第96课 如何应用12导联心电图预测室性心律失常起源
解剖基础
当以体态视角观看心脏时,右心腔室较左心腔室靠前。右心室位于左心室的右前方。在胸腔内,左心室倾斜走向,基底部靠后,心尖部朝左。事实上,所谓的前室间沟始于上方,向左走行,略向前,而所谓的后室间沟实际上位于下方。
就流出道区域而言,解剖复杂,源于该区域不同结构的室性心律失常(VAs)具有类似的心电图表现。右心室流出道(RVOT)从前方包绕并跨过左心室流出道(LVOT),因此,肺动脉瓣位于主动脉瓣的前方和左侧。这一关系是重要的,因为RVOT的前面部分实际上是最靠左侧且最高位的流出道结构。
LVOT相当于左心室的椭圆形出口,McAlpine称其为左心室口。其组成前方为主动脉根部,后方为二尖瓣环,朝向左侧。解剖上主动脉瓣和二尖瓣通过纤维组织带相连,即主动脉二尖瓣结合部,从二尖瓣前叶到主动脉瓣的左冠窦和无冠窦。主动脉瓣占据心脏的中心位置,由3个窦组成,各有相应的解剖关系。在体态方向上,相对于胸骨右冠窦最为靠前,无冠窦靠后偏右,左冠窦靠后偏左。无冠窦位置最低,左冠窦位置最高。右冠窦紧密连接RVOT的后间隔部分,而左冠窦毗连左心室口前部,接近左前降支冠状动脉。相反,无冠窦与左心房和右心房之间由房间隔分隔。右冠窦和无冠窦结合处下方为室间隔膜部,希氏束穿行于此。
心电图特征
许多心电图特征与特定的VAs定位有关。最重要的有(1)QRS波群心电轴,(2)束支传导阻滞图形,(3)心前区移行,和(4)QRS波群宽度。
QRS波群心电轴包含垂直(上-下)与水平(左-右)方向。垂直方向反映在双极导联Ⅱ和Ⅲ的QRS极性上。例如,所有流出道VAs的QRS波群心电轴向下,Ⅱ和Ⅲ呈正向波。水平方向主要反映在Ⅰ上。接近左臂的结构将在Ⅰ产生深度负向波(心电轴右偏);相反,接近右臂的结构将在Ⅰ产生明显的正向波(心电轴左偏)。另一与水平方向类同的是肢体aVR和aVL间的振幅比:正向极性aVR大于aVL的,提示起源偏左,正向极性aVL大于aVR的起源偏右。
束支传导阻滞图形与左右心室的激动顺序有关。呈右束支传导阻滞(RBBB)图形的VAs来自左心室,而呈左束支传导阻滞(LBBB)图形的VAs可来自右心室的任何部位,但也可来自室间隔左侧。
当起源部位从间隔部位转向右心室游离壁时,RBBB图形VAs的心前区移行(出现以S波为主的第一个胸导联)逐渐提前。起源于心脏基底部的VAs心室激动朝向前方和心尖,所有胸导联一致表现为正向波。相反,起源接近心尖的VAs,电激动背离胸壁,胸导联均为负向波。
最后,间隔部位起源VAs同步而非先后激动两心室,因此,QRS波群较心室游离壁起源的窄。
预测起源部位的综合解剖定位方法
步骤1
我们先看向上/向下心电轴,这反映在Ⅱ和Ⅲ的极性上。心电轴向下的VAs(Ⅱ和Ⅲ正向QRS波群)起源于心脏基底区域,包括流出道和房室瓣上部,心电轴向上的VAs(Ⅱ和Ⅲ负向QRS波群)起源于两心室下部。
步骤2
下一步是区分VAs来自胸部中线的左侧或右侧,这并不意味着一定是左心室对右心室,尤其在流出道,左右流出道之间存在明显的重叠。
1.对于流出道起源VAs,最佳单一心电图鉴别点是Ⅰ左偏/右偏心电轴。偏右结构起源的,如RVOT后部、右冠窦、希氏束旁区及三尖瓣环上部,Ⅰ为正向波,而偏左结构起源的,如RVOT的前部、左冠窦、主动脉二尖瓣结合部、二尖瓣环前外侧及左心室顶部,Ⅰ为负向波。右冠窦和左冠窦结合处是特发性VAs的常见起源部位,接近中线,基于我们的经验,该区域起源的VAs在Ⅰ可表现为正向、负向或双向的QRS波群。
2.对于心室下部起源的VAs,最具有帮助的是束支传导阻滞图形,尽管一些左心室间隔部位起源的VAs可呈心电轴左偏。心电轴向上伴LBBB图形的VAs起源部位可以是右心室结构(三尖瓣环下部或调节束)或心脏十字沟。相反,心电轴向上伴RBBB图形的VAs起源于左心室结构(二尖瓣环下部,后内侧乳头肌,或左后分支)。
步骤3
当我们将预期的起源部位限定于4个象限之一时,更精细的定位依赖于其他特征,如心前区移行、QRS波群宽度或特殊导联的QRS形态。
右上象限:这包括RVOT的后面部分、右冠窦、三尖瓣环上部和希氏束旁区(图1A-E)。总体上,通过观看aVL的极性即能区分流出道起源VAs与三尖瓣环和希氏束旁区起源VAs。aVL是左侧向上导联,因此,多数流出道VAs在此导联上与aVR一样呈现负向波(QS波)。相反,三尖瓣环和希氏束旁区位置较低且偏向胸部右侧,因此,常在aVL上表现为正向波(R或r波)。另外,RVOT和右冠窦起源VAs显示明显的向下心电轴,Ⅱ和Ⅲ表现为高R波。三尖瓣环和希氏束旁区起源VAs的正向向量不突出,特别在Ⅲ,可以表现为等电位或负向波。最后,希氏束旁区起源VAs,因为早期激动希-浦系统,典型表现为窄QRS间期(通常<130 ms)。
左上象限:这包括RVOT前部和多数LVOT结构(除外右冠窦)(图1F-L)。在此组中,心前区移行是值得关注的最有利特征。当从RVOT游离壁逐渐转向较后面的二尖瓣环外侧时,心前区移行逐渐提前(RVOT游离壁为V4或V5,RVOT间隔为V3或V4,左冠窦为V1或V2),最后,在主动脉二尖瓣结合部或二尖瓣环顶部图形从LBBB转为RBBB。除了LBBB图形外,V1的一些特征有助于定位:RVOT和右冠窦VAs典型表现为QS波;QS波伴有切迹时提示来自右冠窦与左冠窦结合处;左冠窦VAs常在V1呈现多相波图形(M或W形);V1qR波常见于主动脉二尖瓣结合部起源的VAs;二尖瓣环前外侧起源VAs在V1常呈R波,且心前导联均为正向波。
右下象限:该象限特发性VAs最常见起源为三尖瓣环下部、调节束和心脏十字沟(图2A-C)。调节束是一突出的肌小梁,从右心室间隔部跨越至游离壁,对三尖瓣的前乳头肌起支撑作用。心脏的十字沟为心外膜区域,接近心中静脉与冠状窦连接处。调节束起源VAs典型表现为左上心电轴和心前区移行晚(V4以后)。相反,十字沟起源VAs也呈左上心电轴,但移行早(V2),且下壁导联呈QS波。它们也可出现提示心外膜起源的特征图形,如假性delta波或最大反折指数>0.55。三尖瓣起源VAs心前区移行范围大(从V2到V5),这决定于间隔或侧壁起源(V2或V3为间隔起源,V4或V5为游离壁起源)。大多数三尖瓣环间隔部起源VAs V1呈QS波,而多数游离壁起源VAs V1呈rS波。
左下象限:呈RBBB且心电轴向上的特发性VAs可起源于二尖瓣环下部、左后分支及左后乳头肌(图2D–F)。这可基于三大特征加以鉴别:心前移行、QRS间期和V1图形。心前导联一致正向(V6R>S)对于二尖瓣起源VAs是相对特异的,反映它们较基底的位置。相反,左后分支或左后乳头肌起源的VAs通常V5R<S。QRS时间<130 ms高度提示分支型VAs,反映了经过浦肯氏系统的较快心室除极。基于相同的理由,分支型VAs V1上典型表现为rsR′(r<R′)波,类似典型的RBBB。相比较,左后乳头肌和二尖瓣环起源VAs通常V1呈现Rsr′(R>r′)、R、或qR波。
下壁导联不一致性
下壁导联的不一致性反映在双极肢体导联Ⅱ(从左腿到右臂)和Ⅲ(从左腿到左臂)的除极向量对立。这常见于起源于心室腔内结构(室间隔、调节束和前乳头肌)的VAs,有时见于房室瓣环的外侧部(图2G-H)。正/负不一(Ⅱ+/Ⅲ-)相当于额面电轴-30°到+30°,负/正不一(Ⅱ-/Ⅲ+)相当于额面电轴+150°到+210°。特殊情况下,可能的起源部位如下:
1.正/负不一:右心室结构,包括三尖瓣环外侧、调节束、室间隔(希氏束旁区)。所有这些均呈LBBB图形。
2.负/正不一:左心室结构,包括二尖瓣环外侧和前乳头肌。这些呈RBBB图形。
图1心电轴向下的VAs起源(A)RVOT后间隔,(B)右冠窦,(C)希氏束旁区,(D)三尖瓣环上部,(E)右冠窦-左冠窦结合处,(F)RVOT前部,(G)左冠窦,(H)主动脉二尖瓣结合部,(I)二尖瓣环前外侧,(J)左心室顶部,(K)左前分支,和(L)前外侧乳头肌
图2心电轴向上的VAs起源(A)三尖瓣环下部,(B)调节束,(C)心脏十字沟,(D)二尖瓣环下部,(E)左后分支,和(F)后内测乳头肌。下壁导联不一致的两例VAs消融部位(G)调节束和(H)前外侧乳头肌