非梗阻型MAGP腹腔镜胆囊切除手术时机及糖类抗原19-9变化意义
崔巍 王旭 刘成栋 龚义军 余亮


【摘要】目的 评估非梗阻型轻度急性胆石性胰腺炎(MAGP)腹腔镜胆囊切除术合理的手术时机及血清糖类抗原19-9水平变化在疾病发展过程中的意义。方法 回顾性分析接受早期腹腔镜胆囊切除术治疗的181例非梗阻型MAGP患者的临床资料。按血清淀粉酶及糖类抗原19-9是否阳性将其分为3组(淀粉酶阳性定义为正常值上限的3倍或以上,糖类抗原19-9阳性为超过正常值上限),研究组1为淀粉酶阳性+糖类抗原19-9阴性(28例),研究组2为淀粉酶阳性+糖类抗原19-9阳性(21例),对照组为淀粉酶阴性+糖类抗原19-9阴性(132例)。比较各组手术相关指标及手术前后淀粉酶和糖类抗原19-9变化情况。结果 3组患者在肛门排气时间、中转开腹率及并发症发生率方面比较差异均无统计学意义(P均> 0.05)。术中所见,研究组2患者胆囊、胆囊三角及胆囊周围炎症的严重程度重于其他2组患者。研究组2在手术时间、住院时间、术中出血量方面劣于研究组1和对照组(P均 < 0.05)。淀粉酶陽性或糖类抗原19-9阳性患者腹腔镜胆囊切除术后血清淀粉酶或糖类抗原19-9水平均较术前低(P均< 0.05)。结论 非梗阻型MAGP患者早期行腹腔镜胆囊切除术是安全、有效的;对于同时伴糖类抗原19-9升高者,需警惕炎症的严重性及手术难度,避免并发症的发生。
【关键词】手术时机;腹腔镜胆囊切除术;非梗阻型;轻度急性胆石性胰腺炎;淀粉酶;糖类抗原19-9
【Abstract】Objective To evaluate the significance of optimal timing of laparoscopic cholecystectomy and variations in the serum carbohydrate antigen 19-9 (CA19-9) level during the progression of non-obstructive mild acute gallstone pancreatitis (MAGP). Methods Clinical data of 181 non-obstructive MAGP patients undergoing early laparoscopic cholecystectomy were retrospectively analyzed. All patients were divided into three groups: study group 1 (amylase(+)+CA19-9(-), 28 cases), study group 2 (amylase (+)+CA19-9(+), 21 cases), and control group (amylase (-)+CA19-9(-), 132 cases). Amylase (+) is defined as more than 3 times of the upper limit of normal value and CA19-9(+) is defined as exceeding the upper limit of normal value. Surgery-related parameters and the changes in the amylase and CA19-9 levels before and after surgery were statistically compared among three groups. Results There was no significant difference in the flatus time, rate of conversion to open cholecystectomy and incidence rate of postoperative complications among three groups (all P > 0.05). Intraoperatively, the severity of gallbladder, the triangle of Calot and perigallbladder inflammation in the study group 2 was higher compared with those in the other two groups. The operation time, length of hospital stay and intraoperative blood loss in the study group 2 were significantly worse than those in the study group 1 and control group (all P < 0.05). Postoperative serum levels of amylase and CA19-9 in patients with amylase (+) or CA19-9 (+) were significantly lower than preoperative levels (both P < 0.05). Conclusions Early laparoscopic cholecystectomy is safe and effective for patients with non-obstructive MAGP. Nevertheless, for those complicated with elevated CA19-9 levels, extensive cautions should be taken for the severity of inflammation and surgical difficulty to avert the incidence of postoperative complications.
【Key words】Surgical timing;Laparoscopic cholecystectomy;Non-obstructive;Mild acute gallstone pancreatitis;Amylase;Carbohydrate antigen 19-9
目前,对于急性结石性胆囊炎或慢性结石性胆囊炎急性发作患者,行早期腹腔镜胆囊切除术(ELC)治疗已被广大外科医师接受,但对于血清淀粉酶水平达正常值上限3倍或以上且无胆管结石或胆管梗阻者,即非梗阻型轻度急性胆石性胰腺炎(MAGP)患者,其ELC的手术时机目前尚未达成共识。同时有研究显示,非梗阻型MAGP患者入院时血清糖类抗原19-9(CA19-9)水平往往升高,升高机制尚不清楚,血清CA19-9水平在胆胰的良恶性疾病中均可升高,有时较难区分疾病性质[1]。笔者见目前国内外关于CA19-9在急性胆囊炎疾病的发生、发展中的作用研究甚少。在本研究中,我们评估了非梗阻型MAGP患者的手术时机以及血清CA19-9水平变化及其与疾病的关联,以期指导临床决策。
对象与方法
一、研究对象
收集2018年10月至2019年10月于我科接受ELC治疗的183例非梗阻型MAGP患者的临床资料。181例患者的症状主要为右上腹疼痛、恶心、呕吐;体征为局限于上腹部的压痛和(或)伴轻度反跳痛;入院后均经腹部B超和磁共振胰胆管造影(MRCP)证实有胆囊结石,不合并胆管结石,无胆胰恶性肿瘤影像学征象。181例均无肝内外胆道梗阻及阻塞性黄疸表现,无明显血清胆红素和转氨酶异常,无消化道恶性肿瘤,无器官衰竭,无局部并发症(包括胰周积液、胰腺和胰周坏死及假性囊肿形成等),无全身并发症[2]。
淀粉酶的阳性定义为正常值上限的3倍或以上;CA19-9阳性定义为超过正常值上限。根据血清淀粉酶及CA19-9是否阳性将181例分为3组,研究组1为淀粉酶阳性+ CA19-9阴性,共28例;研究组2为淀粉酶阳性+ CA19-9阳性,共21例;对照组为淀粉酶阴性+ CA19-9阴性,共132例。淀粉酶阴性+ CA19-9阳性病例仅2例,且为CA19-9轻度升高,故排除,最后共纳入181例患者的资料作分析。所有患者围术期均给予抗感染、补液或解痉等对症处理。由于本研究中淀粉酶阳性者多为血清淀粉酶水平轻度升高,因此不常规予抑酸、抑酶治疗。
本研究符合医学伦理学并通过我院医学伦理委员会批准,诊疗过程均经患者本人或家属同意,并签署了知情同意书。
二、观察指标
181例患者均于入院后96 h内接受ELC,均采用3孔法。观察并比较各组手术时间、术后肛门排气时间、住院时间、术中出血量、中转开腹率、术后并发症发生率。比较血清淀粉酶阳性及CA19-9阳性者手术前后血清淀粉酶及CA19-9的变化情况。
三、统计学处理
采用SPSS 17.0进行数据分析。计量资料以表示,多组间比较采用单因素方差分析,两两比较采用LSD-t检验;手术前后比较采用配对t检验;计数资料以例(%)表示,组间比较采用χ2检验或Fisher确切概率法。P < 0.05为差异具有统计学意义。
结果
一、3组非梗阻型MAGP患者一般情况比较
3组患者的性别、年龄、术前住院时间比较差异无统计学意义(P > 0.05)。研究组1和研究组2术前血清淀粉酶水平高于对照组(P均< 0.05),研究组2术前血清CA19-9水平高于研究组1和对照组(P均< 0.05),见表1。
二、3组非梗阻型MAGP患者手术相关指标比较
术中所见,研究组2患者胆囊、胆囊三角及胆囊周围炎症程度较其他2组患者重,胆囊颈部结石及胆囊胆汁淤积情况也更严重,见图1。3组患者的肛门排气时间、中转开腹率及并发症发生率比较差异无统计学意义(P > 0.05)。中转开腹原因:对照组中2例为胆囊管变异,1例为胆囊三角炎症严重,解剖困难;研究组1和研究组2各有1例胆囊三角区域组织粘连严重。3组的并发症主要为切口感染以及肺部感染,均未发生胆道损伤、胆漏、胆道狭窄及梗阻、腹腔出血等并发症。研究组2在手术时间、住院时间、术中出血量方面劣于研究组1和对照组(P均< 0.05)。研究组1和对照组的各项手术相关指标比较差异均无统计学意义(P均> 0.05),见表2。
三、血清淀粉酶阳性及CA19-9阳性者手术前后血清淀粉酶及CA19-9变化情况
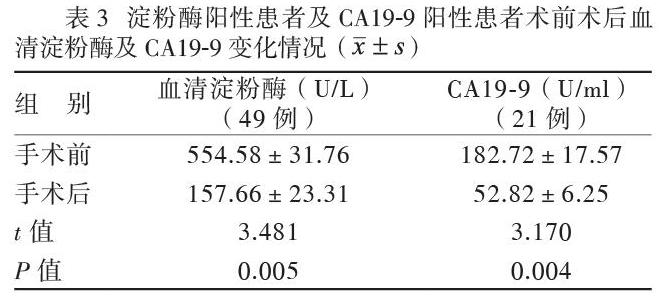
血清淀粉酶阳性及CA19-9阳性者术后2项指标均较术前下降(P均< 0.05),见表3。
讨论
胆囊结石在发达国家的发病率为10% ~ 15%,其中高达20%为急性结石性胆囊炎,胰腺炎患者中80%为轻度急性胰腺炎,而急性胰腺炎中约30% ~ 55%为胆石性胰腺炎[3]。病理学和放射学研究表明,胆囊结石和胰腺炎的伴随发生率可能远高于人们既往认为的那样[4]。CA19-9是胆胰恶性肿瘤最常用的标志物,90%胆胰恶性肿瘤患者血清CA19-9水平超过37 U/ml[5]。CA19-9升高也可见于多种良性疾病,如胆管炎、肝脂肪变性、泌尿系结石、肝肾囊肿和胆囊炎等[6-7]。有研究显示,老年急性胆囊炎患者(年龄> 65岁)入院时CA19-9水平为(620.5±205.6) U/ml,在接受经皮经肝胆囊穿刺引流术治疗后72 h内,其CA19-9水平降至(55.2±20.1)U/ml,提示CA19-9可能在胆囊炎症急性发作中发挥重要作用[8]。
目前ELC应用于胆囊炎急性发作期已被临床医师广泛接受,美国胃肠病学会、国际胰腺病学会及美国胰腺病学会也推荐对非梗阻型MAGP患者行ELC治疗[9]。但有研究显示这可能会造成一部分进展中未被识别的坏死性胰腺炎患者出现潜在的严重后果[10]。同时有研究显示,术前高淀粉酶血症与腹腔鏡胆囊切除困难显著相关,术前血清淀粉酶水平升高会增加中转开腹的风险,故建议对于此类患者延迟手术[11-12]。因此,目前对于非梗阻型MAGP手术时机尚未达成一致。各个国际指南对于ELC的“早期”定义缺乏共识,有学者将其定义为症状发作后3 d内或7 d内,也有学者将其定义为入院后1周内或2周内[13-17]。对于“早期”定义的多样化可能是导致各研究结论存在偏差的原因[18]。我们的研究小组一直致力于探索胆囊炎症急性发作时的最佳手术时机,并定义急性发病入院后96 h内为“早期”[19]。术前正确预测手术难度可以避免多种手术带来的相关问题[20]。在本研究中,非梗阻型MAGP患者均无胆管结石及胆管梗阻,其血清淀粉酶升高原因并不明确,我们推测可能与患者胆囊功能减退有关,由于Oddis 括约肌与胆囊间存在局部反射,在胆囊收缩功能减退的情况下,Oddis括约肌运动功能受到抑制,进而可能导致血清淀粉酶升高[21]。我们发现,研究组1与对照组手术及术后各项相关指标无差异,2组术中胆囊炎症程度及手术难易程度也相似,提示血清淀粉酶水平不代表急性胆囊炎的严重程度,这与近期的研究结果相似,淀粉酶并不是一个可靠的炎性诊断指标[22-23]。本研究结果显示,对于非梗阻型MAGP患者,ELC是安全、有效的,与对照组相比并不增加手术时间、中转开腹率、术后并发症发生率和住院时间,与部分研究结果相同[24-26]。
ELC能夠降低整体风险,避免或减少疾病复发,改善患者生活质量[27]。
尽管3组之间中转开腹率无差异,但我们在术中发现,研究组2患者胆囊、胆囊三角及胆囊周围炎症程度较其他2组患者重,胆囊颈部结石及胆囊胆汁淤积情况也更严重。研究组2的手术时间、术中出血量和住院时间劣于研究组1和对照组。我们考虑CA19-9可能是一个特异性炎症指标,在胆囊炎症急性发病中发挥重要作用。一般来说,胆胰恶性肿瘤及部分阻塞性黄疸患者血清CA19-9水平显著升高。我们发现,胆囊炎症程度较重的研究组2患者的CA19-9水平大多数为轻度升高,我们推测其升高的机制及与胆囊炎症的关系为:胆囊管结石嵌顿,引起胆囊管不同程度阻塞,胆囊内压力升高,炎症加剧,胆囊壁上皮细胞受损;胆囊上皮细胞中的CA19-9产生增加,并进入血液循环;同时病情进一步加重会导致炎症从胆囊底部扩散到肝脏内。本研究结果显示,胆囊切除术后CA19-9水平较术前下降,因此,我们认为CA19-9水平变化对预测胆囊炎症的严重程度和手术难度可能起一定的指导作用。
综上所述,对非梗阻型MAGP患者实施ELC是安全、有效的,对于同时伴CA19-9升高者,则需谨慎,在排除恶性肿瘤的同时,要充分认识胆囊炎症的严重程度及手术的难度,避免胆道及手术相关并发症的发生。由于本研究为回顾性研究,且样本量较少,研究结果需要经更高质量的大样本量前瞻性随机对照研究来进一步验证,以便更好地指导临床工作。
参 考 文 献
[1] Binicier OB, Pakoz ZB. CA19-9 levels in patients with acute pancreatitis due to gallstone and metabolic/toxic reasons. Rev Assoc Med Bras (1992), 2019,65(7):965-970.
[2] Mueck KM, Wei S, Liang MK, Ko TC, Tyson JE, Kao LS. Protocol for a randomized trial of the effect of timing of cholecystectomy during initial admission for predicted mild gallstone pancreatitis at a safety-net hospital. Trauma Surg Acute Care Open, 2018,3(1):e000152.
[3] Aksoy F, Demiral G, Ekinci ?. Can the timing of laparoscopic cholecystectomy after biliary pancreatitis change the conversion rate to open surgery? Asian J Surg, 2018,41(4):307-312.
[4] Pereira J, Afonso AC, Constantino J, Matos A, Henriques C, Zago M, Pinheiro L. Accuracy of ultrasound in the diagnosis of acute cholecystitis with coexistent acute pancreatitis. Eur J Trauma Emerg Surg, 2017,43(1):79-83.
[5] Kim MS, Jeon TJ, Park JY, Choi J, Shin WC, Park SE, Seo JY, Kim YM. Clinical interpretation of elevated CA19-9 levels in obstructive jaundice following benign and malignant pancreatobiliary disease. Korean J Gastroenterol, 2017,70(2):96-102.
[6] Mei Y, Chen L, Peng CJ, Wang J, Zeng PF, Wang GX, Li WP, Luo YQ, Du C, Liu K, Xiong K, Leng K, Feng CL, Jia JH. Diagnostic value of elevated serum carbohydrate antigen 199 level in acute cholangitis secondary to choledocholithiasis. World J Clin Cases, 2018,6(11):441-446.
[7] Souza-Gallardo LM, de la Fuente-Lira M, Galaso-Trujillo R, Martínez-Ordaz JL. Persistent elevation of CA19-9 and an unexpected finding. A case report. Cir Cir, 2017,85(5):449-453.
[8] Hu YR, Pan JH, Tong XC, Li KQ, Chen SR, Huang Y. Efficacy and safety of B-mode ultrasound-guided percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for acute cholecystitis in elderly and high-risk patients. BMC Gastroenterol, 2015,15:81.
[9] Nesvaderani M, Eslick GD, Cox MR. Acute pancreatitis: update on management. Med J Aust, 2015,202(8):420-423.
[10] Kwong WT, Vege SS. Unrecognized necrosis at same admission cholecystectomy for pancreatitis increases organ failure and infected necrosis. Pancreatology, 2017,17(1):41-44.
[11] Guida F, Monaco L, Schettino M, Porfidia R, Iapicca G. Predictive factors of difficult procedure in octogenarians undergoing elective laparoscopic cholecystectomy: a single center experience. G Chir, 2016,37(2):68-70.
[12] Oymaci E, Ucar AD, Aydogan S, Sari E, Erkan N, Yildirim M. Evaluation of affecting factors for conversion to open cholecystectomy in acute cholecystitis. Prz Gastroenterol, 2014,9(6):336-341.
[13] Guadagni S, Cengeli I, Palmeri M, Bastiani L, Bertolucci A, Modesti M, Galatioto C, Chiarugi M. Early cholecystectomy for non-severe acute gallstone pancreatitis: easier said than done. Minerva Chir, 2017,72(2):91-97.
[14] Navarro-Sanchez A, Ashrafian H, Laliotis A, Qurashi K, Martinez-Isla A. Single-stage laparoscopic management of acute gallstone pancreatitis: outcomes at different timings. Hepatobiliary Pancreat Dis Int, 2016,15(3):297-301.
[15] Zhang J, Li NP, Huang BC, Zhang YY, Li J, Dong JN, Qi TY, Xu J, Xia RL, Liu JQ. The value of performing early non-enhanced CT in developing strategies for treating acute gallstone pancreatitis. J Gastrointest Surg, 2016,20(3):604-610.
[16] Abdelaal A, El-Matbouly M, Sulieman I, Elfaki A, El-Bakary T, Abdelaziem S, Gehani S, Toro A, Di Carlo I. Role of intraoperative cholangiography for detecting residual stones after biliary pancreatitis: still useful? A retrospective study. World J Emerg Surg, 2017,12:18.
[17] E?in S, Ye?ilta? M, G?k?ek B, Tezer H, Karahan SR. Early laparoscopic cholecystectomy following acute biliary pancreatitis expedites recovery. Ulus Travma Acil Cerrahi Derg, 2017,23(6):495-500.
[18] Zhong FP, Wang K, Tan XQ, Nie J, Huang WF, Wang XF. The optimal timing of laparoscopic cholecystectomy in patients with mild gallstone pancreatitis: a meta-analysis. Medicine (Baltimore), 2019,98(40):e17429.
[19] Cui W, Zhang RY, Sun DQ, Gong RH, Han TQ. Early laparoscopic cholecystectomy for acute gallbladder disease in Chinese elderly. Hepatogastroenterology, 2010,57(99-100):409-413.
[20] Chand P, Kaur M, Bhandari S. Preoperative predictors of level of difficulty of laparoscopic cholecystectomy. Niger J Surg, 2019,25(2):153-157.
[21] 胡元元,胡亦懿,周围,李凤棉,潘立群,吕茵,何文娜,王成,欧阳云珍. 胆囊切除术后合并胆管扩张患者肝胆动态显像参数分析及临床意义. 新医学, 2018,49(6):440-444.
[22] Amini M, Pakdaman A, Shapoori S, Mosayebi G. High Mobility Group box-1 (HMGB1) protein as a biomarker for acute cholecystitis. Rep Biochem Mol Biol, 2019,7(2):204-209.
[23] Chang KL, Estores DS. Upper gastrointestinal conditions: pancreatitis. FP Essent, 2017,458:25-32.
[24] Guadagni S, Cengeli I, Palmeri M, Bastiani L, Bertolucci A, Modesti M, Galatioto C, Chiarugi M. Early cholecystectomy for non-severe acute gallstone pancreatitis: easier said than done. Minerva Chir, 2017,72(2):91-97.
[25] Mueck KM, Wei S, Pedroza C, Bernardi K, Jackson ML, Liang MK, Ko TC, Tyson JE, Kao LS. Gallstone pancreatitis: admission versus normal cholecystectomy-a randomized trial(gallstone PANC trial). Ann Surg, 2019,270(3): 519-527.
[26] Riquelme F, Marinkovic B, Salazar M, Martínez W, Catan F, Uribe-Echevarría S, Puelma F, Mu?oz J, Canals A, Astudillo C, Uribe M. Early laparoscopic cholecystectomy reduces hospital stay in mild gallstone pancreatitis. A randomized controlled trial. HPB (Oxford), 2020,22(1):26-33.
[27] Parkin E, Stott M, Brockbank J, Galloway S, Welch I, Macd-onald A. Patient-reported outcomes for acute gallstone pathology. World J Surg, 2017,41(5):1234-1238.
(收稿日期:2020-02-20)
(本文編辑:洪悦民)

