破裂脑动脉瘤不同时机夹闭术后的颅内压监测研究
许雅纹 方文华 蔡嘉伟

[摘要]目的 探討破裂脑动脉瘤不同时机夹闭术后患者的颅内压(ICP)变化特点。方法 回顾性分析2014年10月~2016年9月我院收治的满足纳入和排除标准的49例成人破裂脑动脉瘤患者的临床资料,按照动脉瘤夹闭手术时间分为早期(发病≤3 d)手术组(26例)和延迟(发病4~21 d)手术组(23例),两组均在术后行持续ICP监测及以ICP为导向的综合治疗。比较、分析两组患者术后ICP变化特点及其临床意义。以随访12个月的死亡率和改良Rankin量表(mRS)评分评价两组患者的预后。结果 两组患者的影像学特征方面、预后情况比较,差异无统计学意义(P>0.05)。早期手术组患者术后ICP总体平均值为(15.21±3.71)mmHg,高于延迟手术组的(14.12±4.13)mmHg,差异有统计学意义(P<0.05)。早期手术组患者术后ICP平均值呈现先缓慢增高而后下降的趋势,术后第3、5天均高于术后第1天,其中以术后第5天最高,而术后第7天则降低,且低于术后第1天,差异有统计学意义(P<0.05);延迟手术组患者术后第2天ICP平均值增高之后即开始下降,术后第6、7天均低于术后第1天,其中以术后第7天为最低,差异有统计学意义(P<0.05);两组患者术后第7天的ICP平均值比较,差异无统计学意义(P>0.05)。结论 发病3 d内早期手术的破裂脑动脉瘤患者术后总体ICP高于延迟手术组。早期手术和延迟手术术后ICP均呈先增高而后下降的趋势,早期手术最高峰在第5天,而延迟手术术后第2天最高。两种手术时机术后患者的ICP在经过治疗后均能够下降至较低水平。这一规律有助于破裂脑动脉瘤术后ICP增高临床诊疗策略的制定。
[关键词]脑动脉瘤;蛛网膜下腔出血;颅内压监测;预后
[Abstract] Objective To explore the characteristics of intracranial pressure (ICP) in patients after ruptured cerebral aneurysms clipped at different timing. Methods The clinical data of 49 adult patients with ruptured cerebral aneurysm in our hospital who met the inclusion and exclusion criteria from October 2014 to September 2016 were retrospectively analyzed. They were divided into the early surgery (≤ 3 days after onset) group (26 cases) and delayed surgery (4-21 days after onset) group (23 cases) according to the timing of clipping. The continuous ICP monitoring and ICP-oriented comprehensive treatment were performed after surgery in both groups. The characteristics and clinical significance of postoperative ICP of patients in two groups were compared and analyzed. The prognosis of the patients in two groups was evaluated by mortality and modified Rankin scale (mRS) score at 12-month follow-up. Results There were no significant differences in imaging characteristics and prognosis between the two groups of patients (P>0.05). The total average postoperative ICP of patients in the early surgery group was (15.21±3.71) mmHg, which was higher than that in the delayed surgery group for (14.12±4.13) mmHg, and the difference was statistically significant (P<0.05). The average postoperative ICP of patients in the early surgery group increased slowly and then decreased, average ICP on the third and fifth days after surgery was higher than that at the first day, with the highest on the fifth day and it decreased on the seventh day after surgery, and was lower than that on the first day after surgery, with statistically significant differences (P<0.05). In the delayed surgery group, the average ICP started to decrease on the second day after surgery, and the average ICP on the sixth and seventh days after surgery was lower than that on the first day, lowest on the seventh day after surgery, with statistically significant differences (P<0.05). There was no significant difference in the average ICP between the two groups on the seventh day after surgery (P>0.05). Conclusion The total postoperative ICP of patients with ruptured cerebral aneurysm who have been operated within 3 days after onset is higher than that of delayed surgery. The postoperative ICP of patients with either early or delayed surgery shows a tendency of increasing first and decreasing then. The ICP reaches the peak on the fifth day after early surgery while that on the second day after delayed surgery. The ICP of patients after clipping at different timing can be reduced to a lower level after treatment. This feature may be helpful for the clinical diagnosis and treatment of increased postoperative ICP in patients with ruptured cerebral aneurysm.
[Key words] Cerebral aneurysm; Subarachnoid hemorrhage; Intracranial pressure monitoring; Prognosis
尽管针对破裂脑动脉瘤(cerebral aneurysm)及其导致的动脉瘤性蛛网膜下腔出血(aneurysmal subarachnoid hemorrhage,aSAH)的诊疗技术已获得较大进步,但在全世界范围内其病死率和致残率仍然居高不下,其不良预后与全脑水肿、颅内压(intracranial pressure,ICP)增高、脑血管痉挛、迟发性脑梗死、全身系统并发症等因素密切相关[1-2]。由于医疗条件、水平和理念的差异,不同医院对破裂脑动脉瘤行夹闭或介入治疗的时机选择各不相同,其中对术后ICP增高、脑肿胀等继发脑损害和不良预后的疑虑则是影响手术时机判断的重要因素。有研究指出,aSAH患者存在ICP增高现象,ICP增高的控制是破裂脑动脉瘤临床治疗过程中的重要环节[3]。但对于破裂脑动脉瘤行开颅夹闭手术患者术后ICP变化的特点和规律则较少有文献,因此,本研究旨在分析不同时机夹闭手术患者的ICP变化特点,为临床诊疗提供参考,现报道如下。
1资料与方法
1.1一般资料
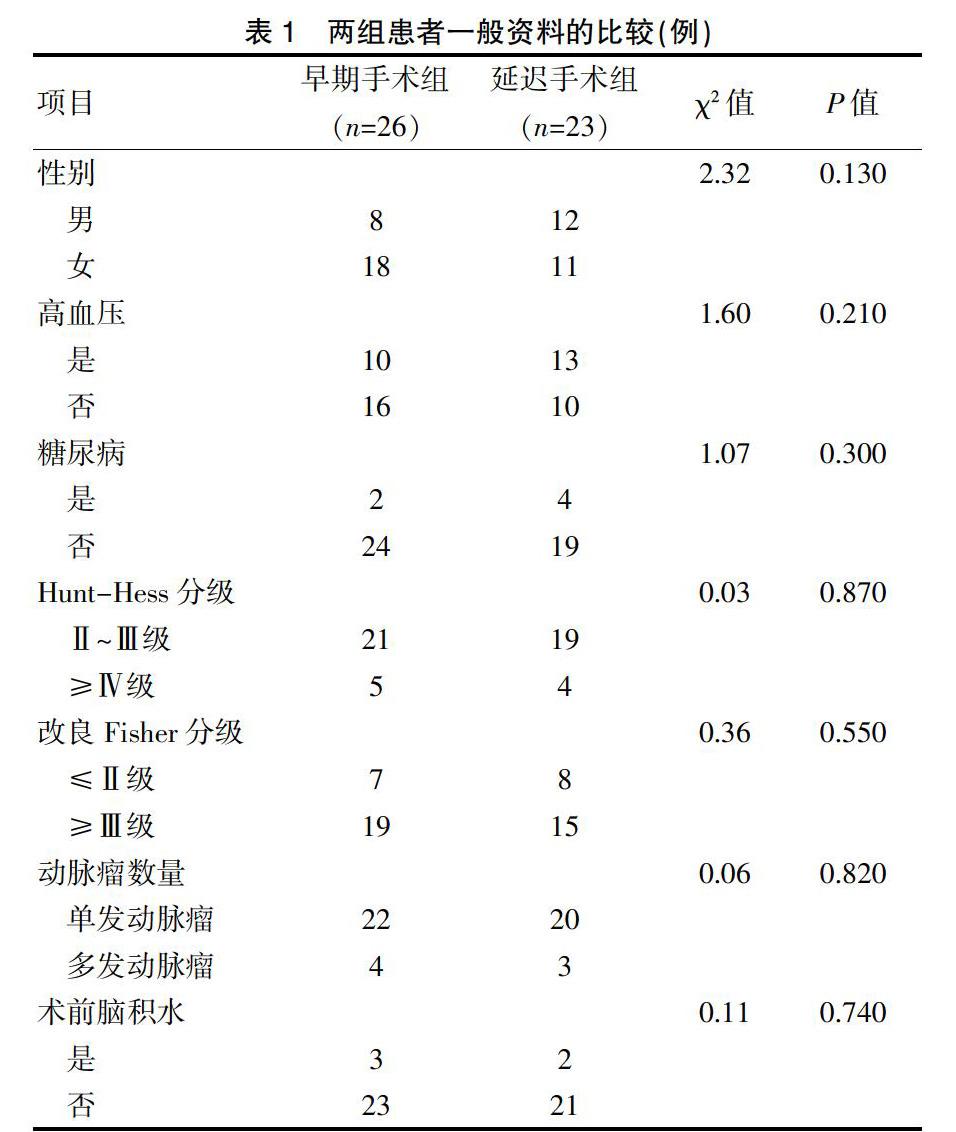
选取2014年10月~2016年9月我院共收治的467例自发性蛛网膜下腔出血患者,其中部分患者根据《神经外科重症管理专家共识》[4]行有创ICP监测,并从中进行研究对象的筛选,同时满足纳入和排除标准的患者49例,对其临床资料进行回顾性分析。纳入标准[5]:①CT显示蛛网膜下腔出血,且CT血管造影术(CTA)或数字减影血管造影(digital subtraction angiography,DSA)确诊为脑动脉瘤;②年龄≥18岁;③Hunt-Hess分级≥Ⅱ级;④经专业组讨论适合行开颅夹闭手术治疗;⑤发病到手术时间≤21 d;⑥持续有创ICP监测时间>24 h。排除标准:①未破裂脑动脉瘤;②严重肝、肾衰竭或凝血功能障碍;③患者及家属拒绝行夹闭手术或ICP传感器置入。按动脉瘤夹闭手术距离发病后的时间,将患者分为早期(发病≤3 d)手术组和延迟(发病4~21 d)手术组。早期手术组患者26例,平均年龄(56.80±12.40)岁。延迟手术组患者23例,平均年龄(55.80±9.40)岁。两组患者年龄、性别、高血压、糖尿病、Hunt-Hess分级、改良Fisher分级、动脉瘤数量、术前脑积水等一般资料比较,差异无统计学意義(P>0.05)(表1),具有可比性。本研究经我院医学伦理委员会审核及同意,患者及家属均知晓治疗情况并签署知情同意书。
1.2方法
两组患者在入院前后均按照2012年美国心脏协会/美国卒中协会(AHA/ASA)《动脉瘤性蛛网膜下腔出血处理指南》[5]进行诊疗。在术前准备完善并经全科讨论符合夹闭手术条件,行经翼点锁孔入路开颅,显微镜下确认破裂责任动脉瘤并予夹闭,清除可见血肿。置入ICP传感器(Codman,USA):伴有脑积水或脑室内出血患者选择脑室型置于侧脑室内,其余患者选择脑实质型置于同侧额叶皮层下2 cm处。术后给予神经重症监护,每个患者每天至少进行3次临床评估[包括格拉斯哥昏迷量表(GCS)评分、Ramsay镇静评分、神经功能障碍程度评估等]。术后24 h内常规复查头颅CT,1周内复查头颇CTA或DSA,病情变化或ICP持续增高时随时复查头颅CT或CTA以明确颅内情况等。术后行持续ICP监测,并采取以ICP监测为导向的综合治疗策略。ICP控制措施采用阶梯式方案,包括抬高床头、维持正常体温、镇静、镇痛、呼吸道管理、脱水药物(甘露醇、速尿)、渗透压治疗(维持血浆渗透压300~320 mOsm/L)、轻度过度通气[动脉二氧化碳分压(PaCO2)30~35 mmHg]等。
1.3观察指标及评价标准
所有患者的术前、术后影像学资料由两名高年资主治以上医师独立阅片,评估两组患者的脑积水、环池受压、中线移位≥5 mm、侧脑室受压和颅内低密度灶(提示脑缺血或脑水肿)等情况。ICP控制与数据采集:所有患者通过数据连接线联接ICP监护仪和床旁心电监护仪(BeneView T6,Mindray,中国),实时采集并存储术后ICP数据,在剔除受干扰的异常值后,取每个患者每24小时的ICP平均值,对两组患者术后不同时间点ICP的高低、变化趋势、峰值出现时间等进行分析。以发病后12个月为随访时间点,采取门诊和电话随访方式,评估两组患者的死亡率和改良Rankin量表(mRS)评分情况,其中mRS≤3分为预后良好,mRS 4~5分及死亡病例归为预后不良。
1.4统计学方法
采用SPSS 17.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;计数资料采用率表示,组间比较采用Fisher确切概率法检验,以P<0.05为差异有统计学意义。
2结果
2.1两组患者影像学特征和预后情况的比较
两组患者围术期均未出现再出血。早期手术组中,有15例患者术后CT上显示环池受压、中线移位≥5 mm、侧脑室受压征象,8例显示颅内低密度灶;延迟手术组中,有17例患者术后CT上显示环池受压、中线移位≥5 mm、侧脑室受压征象,7例显示颅内低密度灶。两组患者的影像学特征方面比较,差异无统计学意义(P>0.05)。随访12个月,早期手术组中,预后良好22例,预后不良4例(其中包括1例死亡);延迟手术组中,预后良好16例,预后不良7例。两组患者的预后情况比较,差异无统计学意义(P>0.05)。
2.2两组患者术后不同时间点ICP变化趋势的比较
早期手术组患者的ICP总体平均值高于延迟手术组,差异有统计学意义(P<0.05);早期手术组患者术后ICP平均值呈现先缓慢增高而后下降的趋势,术后第3、5天均高于术后第1天,其中以术后第5天最高,而术后第7天则降低,且低于术后第1天,差异有统计学意义(P<0.05);延迟手术组患者术后第2天ICP平均值增高之后即开始下降,术后第6、7天均低于术后第1天,其中以术后第7天为最低,差异有统计学意义(P<0.05);两组患者术后第1~4及7天的ICP平均值比较,差异无统计学意义(P>0.05);早期手术组患者术后第5、6天的ICP平均值均高于延迟手术组,差异有统计学意义(P<0.05)(表2)。
[5]Connolly ES Jr,Rabinstein AA,Carhuapoma JR,et al.Guidelines for the management of aneurysmal subarachnoid hemorrhage:a guideline for healthcare professionals from the American Heart Association/American Stroke Association[J].Stroke,2012,43(6):1711-1737.
[6]Andersen CR,Fitzgerald E,Delaney A,et al.A systematic review of outcome measures employed in aneurysmal subarachnoid hemorrhage (aSAH) clinical research[J].Neurocrit Care,2019,30(3):534-541.
[7]Qian Z,Peng T,Liu A,et al.Early timing of endovascular treatment for aneurysmal subarachnoid hemorrhage achieves improved outcomes[J].Curr Neurovasc Res,2014,11(1):16-22.
[8]Park J,Woo H,Kang DH,et al.Formal protocol for emergency treatment of ruptured intracranial aneurysms to reduce in-hospital rebleeding and improve clinical outcomes[J].J Neurosurg,2015,122(2):383-391.
[9]Mahaney KB,Todd MM,Bayman EO,et al.Acute postoperative neurological deterioration associated with surgery for ruptured intracranial aneurysm:incidence,predictors,and outcomes[J].J Neurosurg,2012,116(6):1267-1278.
[10]Cossu G,Messerer M,Stocchetti N,et al.Intracranial pressure and outcome in critically ill patients with aneurysmal subarachnoid hemorrhage:a systematic review[J].Minerva Anestesiol,2016,82(6):684-696.
[11]Zhao DD,Guo ZD,He S,et al.High intracranial pressure may be the initial inducer of elevated plasma D-dimer level after aneurysmal subarachnoid haemorrhage[J].Int J Neurosci,2019,18:1-6.
[12]Etminan N,Chang HS,Hackenberg K,et al.Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region,time period,blood pressure,and smoking prevalence in the population:a systematic review and meta-analysis[J].JAMA Neurol,2019,76(5):588-597.
[13]Florez WA,García-Ballestas E,Deora H,et al.Intracranial hypertension in patients with aneurysmal subarachnoid hemorrhage:a systematic review and meta-analysis[J].Neurosurg Rev,2020.[Epub ahead of print]
[14]Lv Y,Wang D,Lei J,Clinical observation of the time course of raised intracranial pressure after subarachnoid hemorrhage[J].Neurol Sci,2015,36(7):1203-1210.
[15]Darkwah Oppong M,Buffen K,Pierscianek D,et al.Secondary hemorrhagic complications in aneurysmal subarachnoid hemorrhage:when the impact hits hard[J].J Neurosurg,2019,1:1-8.
[16]Duan W,Pan Y,Wang C,et al.Risk factors and clinical impact of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage:analysis from the China National Stroke Registry[J].Neuroepidemiology,2018,50(3-4):128-136.
[17]Olsen MH,Orre M,Leisner ACW,et al.Delayed cerebral ischaemia in patients with aneurysmal subarachnoid haemorrhage:Functional outcome and long-term mortality[J].Acta Anaesthesiol Scand,2019,63(9):1191-1199.
(收稿日期:2020-01-14 本文編辑:任秀兰)