Kidney health for everyone everywhere—from prevention to detection and equitable access to care
-, -,- , , - , , , , , ,sa , yar -0;
1Department of Medicine and Therapeutics,Carol & Richard Yu PD Research Centre,Prince of Wales Hospital,Chinese University of Hong Kong,Hong Kong
2Nephrology Service,Hospital Civil de Guadalajara Fray Antonio Alcalde,University of Guadalajara Health Sciences Center,Guadalajara,Jalisco,Mexico
3Division of Health System,Policy and Management,Jockey Club School of Public Health and Primary Care,The Chinese University of Hong Kong,Hong Kong
4James Whitcomb Riley Hospital for Children,Indiana University School of Medicine,Indianapolis,Indiana,USA
5World Kidney Day Office,Brussels,Belgium
6Tanker Foundation,Chennai,India
7Division of Nephrology and Hypertension,1st Department of Internal Medicine,AHEPA Hospital,Aristotle University of Thessaloniki,Thessaloniki,Greece
8Nephrology Unit,Department of Internal Medicine,Faculty of Medicine,Cairo University,Giza,Egypt
9Renal Unit,Department of Medicine,College of Medicine,University of Nigeria,Ituku-Ozalla,Enugu,Nigeria
10Division of Nephrology and Hypertension and Kidney Transplantation,University of California Irvine School of Medicine,Orange,California,USA
Key words awareness detection kidney diseases prevention
Around 850 million people currently are affected by different types of kidney disorders. Up to 1 in 10 adults worldwide has chronic kidney disease (CKD),which is invariably irreversible and mostly progressive. The global burden of CKD is increasing,and CKD is projected to become the fifth most common cause of years of life lost globally by 2040. If CKD remains uncontrolled and if the affected person survives the ravages of cardiovascular and other complications of the disease,CKD progresses to end-stage kidney disease,where life cannot be sustained without dialysis therapy or kidney transplantation. Hence,CKD is a major cause of catastrophic health expenditure. The costs of dialysis and transplantation consume 2%-3% of the annual health care budget in high-income countries,spent on less than 0.03% of the total population of these countries.
Importantly,however,kidney disease can be prevented and progression to end-stage kidney disease can be delayed with appropriate access to basic diagnostics and early treatment including lifestyle modifications and nutritional interventions. Despite this access to effective and sustainable health care provision programs,kidney care remains highly inequitable across the world. Indeed,of parallel importance is the ongoing health inequity in CKD care including inequity of health care access particularly among some of the indigenous populations in certain regions of the world,and this may have a bearing on the preexisting and emerging health gaps between low-middle-income,middle-income,and high-income countries. Kidney disease is crucially missing from the international agenda for global health. It is notably absent from the impact indicators for theSustainableDevelopmentGoalGoal 3,Target 3.4,“By 2030,reduce by one third premature mortality from n ̄o ̄n ̄c ̄o ̄m ̄m ̄u ̄n ̄i ̄c ̄a ̄b ̄l ̄e diseases (NCDs) through prevention and treatment and promote mental health and well-being,” and the latest iteration of the United Nations Political Declaration on NCDs. CKD is a major risk factor for heart disease and cardiac death,as well as for infections such as tuberculosis,and is a major complication of other preventable and treatable conditions including diabetes,hypertension,HIV,and hepatitis. Moreover,consumer engagement and self-help management are crucial to improving kidney health. To that end,the World Kidney Day steering committee suggests adopting strategies that focus on preventative interventions.
Definition and classification of CKD prevention
According to the expert definitions including the Center for Disease Control and Prevention, the term “prevention” refers to activities that are typically categorized by the following 3 definitions:(i)primarypreventionimplies intervening before health effects occur in an effort to prevent the onset of illness or injury before the disease process begins,(ii)secondarypreventionsuggests preventive measures that lead to early diagnosis and prompt treatment of a disease to prevent more severe problems developing and includes screening to identify diseases in the earliest stages,and (iii)tertiarypreventionindicates managing disease after it is well established in order to control disease progression and the emergence of more severe complications,which is often by means of targeted measures such as pharmacotherapy,rehabilitation,and screening for and management of complications. These definitions have important bearing in the prevention and management of CKD,and accurate identification of risk factors that cause CKD or lead to faster progression to renal failure,as shown in Figure 1,is relevant in health policy decisions and health education and awareness related to CKD.
Primary prevention of CKD
Measures to achieve effective primary prevention should focus on the 2 leading risk factors for CKD including diabetes mellitus and hypertension. Other CKD risk factors include polycystic kidneys or other congenital or acquired structural anomalies of the kidney and urinary tracts,primary glomerulonephritis,exposure to nephrotoxic substances or medications (such as nonsteroidal anti-inammatory drugs),having 1 single kidney,for example,solitary kidney after cancer nephrectomy,high dietary salt intake,inadequate hydration with recurrent volume depletion,heat stress,exposure to pesticides and heavy metals (as has been speculated as the main cause of Mesoamerican nephropathy),and possibly high protein intake in those at higher risk of CKD. Among nonmodifiable risk factors are advancing age and genetic factors such as apolipoprotein 1 (APOL1) gene that is mostly encountered in those with sub-Saharan African ethnicity,especially among African Americans. Table 1 shows some of the risk factors of CKD.
Among measures to prevent emergenceofdenovoCKD are screening efforts to identify and manage persons at high risk of CKD,especially those with diabetes mellitus and hypertension. Hence,targeting primordial risk factors of these 2 conditions including metabolic syndrome and overnutrition is relevant to primary CKD prevention as is correcting obesity. Promoting healthier lifestyle includes physical activity and healthier diet. The latter should be based on more plant-based foods with less meat,less sodium intake,more complex carbohydrates with higher fiber intake,and less saturated fat. In those with hypertension and diabetes,optimizing blood pressure and glycemic control has shown to be effective in preventing diabetic and hypertensive nephropathies. Persons with solitary kidney should avoid high protein intake above 1 gram per kilogram body weight per day. Obesity should be avoided,and weight reduction strategies should be considered.
An emerging challenge relevant to these primary preventive efforts is the rise of a new form of CKD that is of “unknown etiology” and is,hence,referred to as “CKDu,” which has resulted in substantial morbidity and mortality including in certain regions of the world with heavy agricultural occupation such as Nicaragua and Sri Lanka. There are currently concerted efforts by the international nephrology community to identify the potential modifiable and nonmodifiable risk factors of CKDu,and to develop potential interventions to mitigate the burden of this emerging disease state.
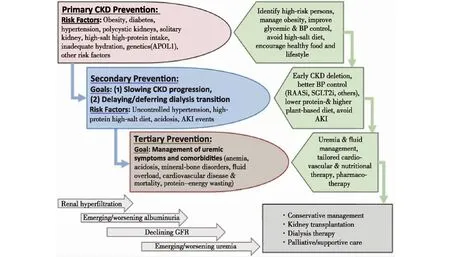
Figure 1 Overview of the preventive measures in chronic kidney disease (CKD) to highlight the similarities and distinctions pertaining to primary,secondary,and tertiary preventive measures and their intended goals
Secondary prevention in CKD
Evidence suggests that among those with CKD,the vast majority have early stage of the disease,that is,CKD stages 1 and 2 with microalbuminuria (30-300 mg/d) or CKD stage 3B (estimated glomerular filtration rate between 45 and 60 ml/min per 1.73 m2). For these earlier stages of CKD,the main goal of kidney health education and clinical interventions for “secondary prevention” is how to slow disease progression. Uncontrolled or poorly controlled hypertension is one of the most established risk factors for faster CKD progression.
The cornerstone of the pharmacotherapy in secondary prevention is the renin-angiotensin-aldosterone system inhibitors. Low protein diet appears to have a synergistic effect on renin-angiotensin-aldosterone system inhibitor therapy. Recent data suggest that a new class of antidiabetic medications known as sodium-glucose cotransporter-2 inhibitors can slow CKD progression,but this effect may not be related to glycemic modulation of the medication. Whereas acute kidney injury may or may not causedenovoCKD,acute kidney injury events that are superimposed on preexisting CKD may accelerate disease progression. A relatively recent case of successful secondary prevention that highlights the significance of implementing preventive strategies in CKD is the use of a vasopressin V(2)-receptor antagonists in adult polycystic kidney disease.
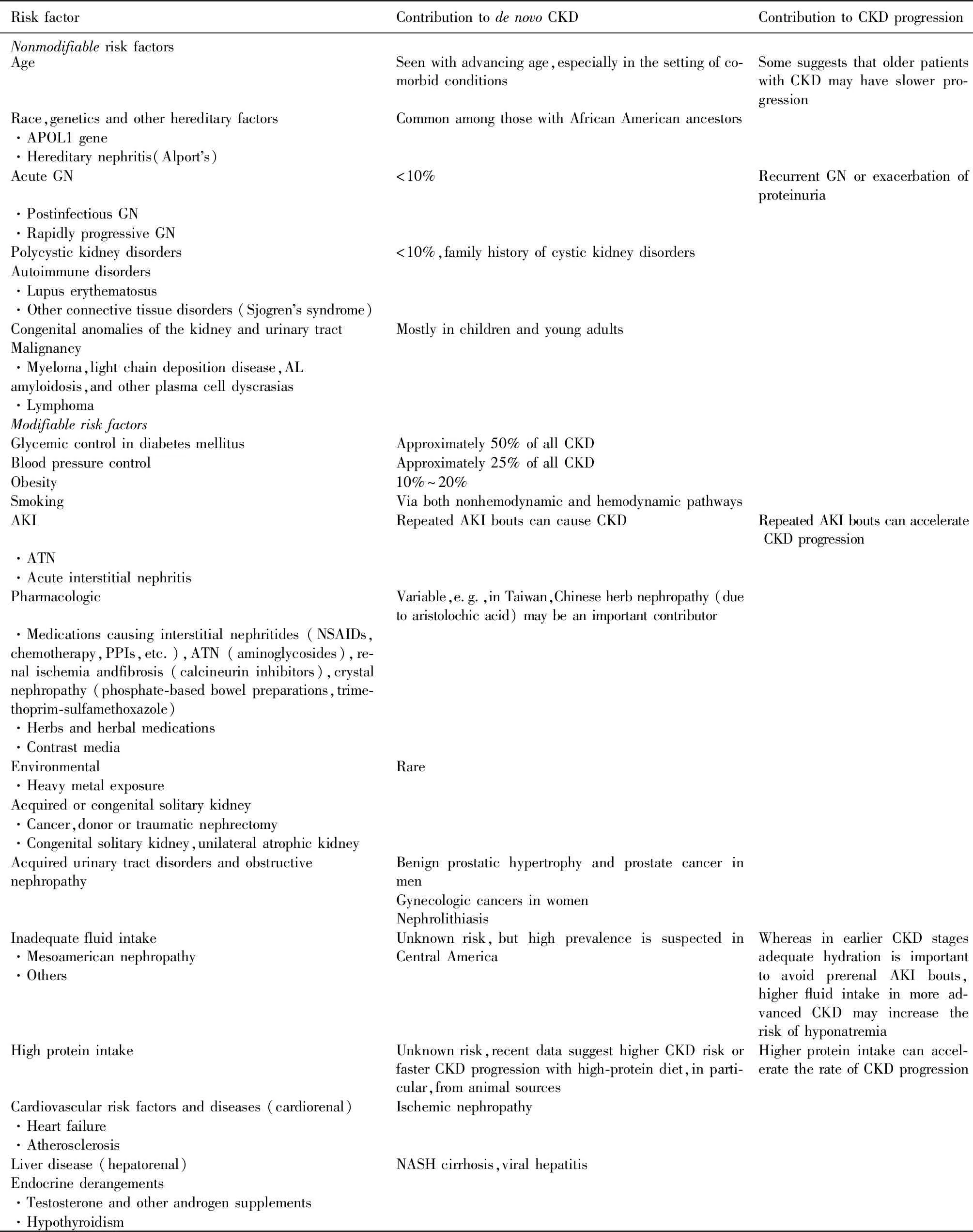
Table 1 Risk factors for de novo CKD as well as preexisting CKD progression
AKI:acute kidney injury; AL:amyloid light-chain; ATN:acute tubular necrosis; CKD:chronic kidney disease; GN:glomerulonephritis; NASH:nonalcoholic steatohepatitis; NSAID:nonsteroidal anti-inammatory drug; PPI:proton pump inhibitor. Many of these risk factors contribute to bothdenovoCKD and its faster progression and hence are relevant to both primary and secondary prevention.
Tertiary prevention in CKD
In patients with advanced CKD,management of uremia and related comorbid conditions such as anemia,mineral and bone disorders,and cardiovascular disease is of high priority,so that these patients can continue to achieve highest longevity. Whereas many of these patients will eventually receive renal replacement therapy in the form of dialysis therapy or kidney transplantation,a new trend is emerging to maintain them longer without dialysis by implementing conservative management of CKD.
Approaches to identification of chronic kidney diseases
The lack of awareness of CKD aroundthe world is one of the reasons for late presentation of CKD in both developed and developing economies. The overall CKD awareness among general population and even high cardiovascular risk groups across 12 low-income and middle-income countries was less than 10%.
Given its asymptomatic nature,screening of CKD plays an important role in early detection. Consensus and Positional Statements have been published by International Society of Nephrology,National kidney Foundation,Kidney Disease Improving Global Outcomes,National Institute of Clinical Excellence (NICE) Guidelines,and Asian Forum for CKD Initiatives.Most guidelines do not recommend population-based screening because of the potential risk of overdiagnoses and the potential harms such as psychological burden of being labeled with CKD. There is also a lack of trial-based evidence to support routine screening and monitoring of CKD.Currently,most will promote a targeted screening approach to early detection of CKD. Some of the major groups at risk for targeted screening includes patients with diabetes and hypertension,those with family history of CKD,individuals receiving potentially nephrotoxic drugs or herbal medicines,patients with past history of acute kidney injury,and individuals older than 65 years.Early detection of CKD could be facilitated among high-risk groups using a urine test for the detection of proteinuria and a blood test to estimate the glomerular filtration rate. Given that low- to middle-income countries may be ill-equipped to deal with the devastating consequences of CKD,particularly the late stages of the disease,effective preventative measures to avoid CKD or to slow progression are of immense importance in these regions. There are suggestions that screening should primarily include high-risk individuals,but also extend to those with suboptimal levels of risk,for example,prediabetes and prehypertension.
Cost-effectiveness of early detection programs
Secondary prevention of CKD relays on timely identification of early signs of CKD including hyperfiltration,microalbuminuria,microscopic hematuria,sporadic foamy urine,and minor elevations in serum creatinine level or other kidney filtration markers. Prior economic evaluations have indicated routine screening using estimated glomerular filtration rate,and urine tests are not cost-effective without risk stratification in the general population. The incremental cost-effectiveness ratios were consistently above $50,000 per life years saved or per quality-adjusted life years unless screening is targeted to higher risk populations,such as those with diabetes mellitus and hypertension and those with rapid CKD progression where routine use angiotensin pathway modulators could be used for renal and vascular risk reduction. To this end,it is important to note some of the key factors that may drive the incremental cost-effectiveness of CKD preventative measures in different regions and health care jurisdictions.
Integration of CKD prevention into national NCD programs
Given the close links between CKD and other NCDs,it is critical that CKD advocacy efforts be aligned with existing initiatives concerning diabetes,hypertension,and cardiovascular disease,particularly in the low-and middle-income countries. Some countries and regions have successfully introduced CKD prevention strategies as part of their NCD management programs. As an example,in 2003,a kidney health promotion program was introduced in Taiwan,with its key components including a ban on herbs containing aristolochic acid,public-awareness campaigns,patient education,funding for CKD research,and the setting up of teams to provide integrated care. In Cuba,the Ministry of Public Health has implemented a national program for the prevention of CKD. It is hoped that the integration of CKD prevention into the NCD program may result in the reduction of renal and cardiovascular risks in the general population. Over time there have been increasingly higher incidences of risk factors for CKD including higher rates of diabetes mellitus and hypertension,and parallel to that more blood pressure medications including renoprotective agents have been prescribed including angiotensin-pathway modulators.Recently,the US Department of Health and Human Services has introduced an ambitious program to reduce the number of Americans developing end-stage kidney disease by 25% by 2030. The program,known as the Advancing American Kidney Health Initiative,has set goals with metrics to measure its success; among them is to put more efforts to prevent,detect,and slow the progression of kidney disease,in part by addressing traditional risk factors such as diabetes and hypertension. Ongoing programs,such as the Special Diabetes Program for Indians,represent an important part of this approach by providing team-based care and care management. Since its implementation,the incidence of diabetes-related kidney failure among American Native populations decreased by over 40% between 2000 and 2015.
The interdisciplinary prevention approach
Since 1994,a National Institutes of Health consensus advocated for early medical intervention in predialysis patients. Owing to the complexity of care of CKD,it was recommended that patients should be referred to a multidisciplinary team consisting of nephrologist,dietitian,nurse,social worker,and health psychologist,with the aim to reduce predialysis and dialysis morbidity and mortality. In Mexico,a nurse-led,protocol-driven,multidisciplinary program reported better preservation in estimated glomerular filtration rate and a trend in the improvement of quality of care of patients with CKD similar to those reported by other multidisciplinary clinic programs in the developed world. Future models should address region-specific causes of CKD,increase the quality of diagnostic capabilities,establish referral pathways,and provide better assessments of clinical effectiveness and cost-effectiveness.
Online educational programs for CKD prevention and treatment
The e-learning has also become an increasingly popular approach to medical education. Online learning programs for NCD prevention and treatment,including CKD,have been successfully implemented in Mexico. By 2015,over 5000 health professionals (including nonnephrologists) had been trained using an electronic health education platform. It is equally important to promote “Prevention” with education programs for those at risk of kidney disease and with the general population at large. Education is key to engaging patients with kidney disease. It is the path to selfmanagement and patient-centered care. Narvaetal. found that patient education is associated with better patient outcomes. Obstacles include the complex nature of kidney disease information,low baseline awareness,limited health literacy,limited availability of CKD information,and lack of readiness to learn. Schatelletal. found that Web-based kidney education is helpful in supporting patient self-management. Reputable health care organizations should facilitate users to have easier access to health information on their websites (Supplementary Appendix S1). Engagements of professional society,patient groups,charitable,and philanthropic organizations promote community partnership and patient empowerment on prevention.
Renewed focus on prevention and awareness raising and education
Given the pressing urgency pertaining to the need for increasing education and awareness of the importance of the preventive measures,we suggest the following goals to redirect the focus on plans and actions:
(i)Empowerment through health literacy in order to develop and support national campaigns that bring public awareness to prevention of kidney disease.
(ii)Population-based approaches to manage key known risks for kidney disease,such as blood pressure control and effective management of obesity and diabetes.
(iii)Implementation of the World Health Organization “Best Buys” approach including screening of at-risk populations for CKD,universal access to essential diagnostics of early CKD,availability of affordable basic technologies,and essential medicines and task shifting from doctors to front-line health care workers to more effectively target progression of CKD and other secondary preventative approaches.
“Kidney Health for Everyone,Everywhere” with emphasis on prevention and early detection should be a policy imperative that can be successfully achieved if policy makers,nephrologists,health care professionals and the general public place prevention and primary care for kidney disease within the context of their Universal Health Coverage programs.
APPENDIX
Members of the World Kidney Day Steering Committee are Philip Kam Tao Li,Guillermo Garcia-Garcia,Sharon Andreoli,Kamyar Kalantar-Zadeh,Latha Kumaraswami,Vassilios Liakopoulos,Siu-Fai Lui,Gamal Saadi,Luisa Strani,and Ifeoma Ulasi.
DISCLOSURE
All the authors declared no competing interests.
参考文献从略