Ultrasonographic assessment of paediatric ocular emergencies: A tertiary eye hospital based observation
Amar Pujari, Deepa R Swamy, Rashmi Singh, Ritika Mukhija, Rohan Chawla, Pradeep Sharma
Dr. Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi 110029, India
KEY WORDS: Paediatric ocular emergencies; Ultrasound B scan; Posterior segment and orbital pathologies
INTRODUCTION
Paediatric patients coming to the ocular emergency can have varied presentations; these cases need careful and systematic evaluation by an experienced paediatric ophthalmologist. The presenting disease can vary from a mild form of conjunctivitis to grievous trauma and posterior segment tumours. Ultrasound becomes even more important in paediatric patients owing to lesser co-operation and clinical difficulty in children. Thus judicious use of B scan ultrasound by an experienced ophthalmologist in these patients will help in the diagnosis of signifi cant posterior segment diseases.[1]
METHODS
Paediatric patients up to the age of 12 years presenting to the ocular emergency services at Dr.Rajendra Prasad Centre for Ophthalmic Sciences, AIIMS,New Delhi between December 2016 to February 2017(90 days) were included in the study. After obtaining written informed consent in the ocular emergency, each patient was evaluated by an experienced paediatric ophthalmologist with a sound experience in posterior segment ultrasonography for at least 1.5 years. This study was adhered to declaration of Helsinki and STROBE guidelines.
All the patients were initially assessed in a systematic way for the following clinical parameters: age of the child, sex, chief complaint, laterality, mode of injury, duration of the complaint, associated systemic conditions, family history, slit lamp biomicroscopic findings and a dilated fundus evaluation (in cases with clear media and if the child was co-operative). A provisional clinical diagnosis was made in patients with opaque anterior segment hindering posterior segment evaluation and was followed by a B scan posterior segment ultrasonography to look for the pathology and to reach a final diagnosis. Authors evaluated all the quadrants of the posterior segment for any vitreous,retinochoroidal or scleral pathology, followed by extraocular muscle pathology within or around them and orbital space-occupying lesions if suspected. B scan ultrasound (Sonomed) of 10 MHz was used for all the patients. The ultrasound was performed gently by placing the probe over closed eyelids. A correct diagnosis could be established in 119 cases. In 3 post traumatic cases there was a diagnostic dilemma between the vitreous haemorrhage alone or vitreous haemorrhage with associated retinal detachment.
Once a fi nal diagnosis is ascertained after combining all clinical and imaging findings, patients were divided into three groups by the treating surgeon. (1) Those that need early medical treatment received appropriate medical treatment and kept under close follow-up. (2)Those that need immediate surgical intervention. For these patients, appropriate management strategy was planned after cumulating all the clinical and imaging data and necessary surgical intervention was performed by an experienced surgeon under the emergency services.(3) In third category, the patients needed an elective intervention after further assessment and systemic stabilization.
RESULTS
The median age at presentation was 6 years (1 month to 12 years). Of the total 122 patients assessed over a period of three months, 78 patients (63.93%) were male and 44 patients (36.07%) were female.
The ocular pathology was unilateral in 122 patients.A signifi cant proportion of the patients presented within 6 hours to 48 hours after the onset of the ocular problem.Blunt ocular trauma constituted a major indication for posterior segment ultrasonography comprising 80(65.57%) patients out of the 122. All eighty patients underwent posterior segment ultrasonography to delineate and define the posterior segment and orbital pathology. Fifty-two patients were found to have anechoic posterior segment whereas in remaining 28 cases, ultrasonography showed various posterior segment pathologies which include (1) vitreous haemorrhage in ten (8.19%) eyes; (2) retinal detachment in eight (6.55%)eyes; (3) choroidal detachment in six (4.91%) eyes; (4)posteriorly dislocated clear lens in one (0.81%) case; and(5) retained intraocular foreign body in seven (5.73%)cases (Figure 1).
Remaining 42 (34.42%) eyes underwent ultrasonographic evaluation for nontraumatic concerns. The indication for ultrasound in this category in descending order include cases of corneal ulcer in 9 (7.37%) eyes, retinoblastoma in 8 (6.55%) eyes, endophthalmitis in 6 (4.91%) eyes,extraocular muscle cysticercosis in 6 (4.91%) eyes, orbital cellulitis in 5 (4.09%) eyes, periocular haemorrhage related to paediatric leukaemias in 3 (2.45%) eyes, proptosis in 2 (1.63%) eyes, pediatric cataract in 2 (1.63%) eyes,complete cryptophthalmos in one (0.81%) eye (Figure 2).No complication or worsening of the ocular pathology was noted as a consequence of performing ultrasound B scan in the emergency.
DISCUSSION
Ocular emergencies need to be addressed at the earliest as they can lead to permanent visual loss once the crucial time period is lost. In our set up emergency services encounters a significant number of paediatric patients who carry a diverse group of posterior segment and orbital pathologies. Clinical examination is of utmost importance in these cases but the presence of anterior segment pathology may hinder a good quality assessment of posterior segment. It is in such cases that ultrasound plays an important role in diagnosing and deciding further management. In the field of ophthalmology,ultrasound is a key imaging modality to decide management and prognosis of various vitreoretinal and orbital conditions. Even though ultrasonography came in post-World War II era, its role has quickly gained importance in elective as well as emergency cases.With improved compactness and portability, use of this modality in emergency services has widened since late 20th century. Point of care ultrasonography basically involves assessment of patient at the bedside with portable ultrasound machine by the clinician to get an instant underlying picture of the patient’s problem. It can then help guide the clinician to decide further course of measures to tackle the disease.
There are few studies which have evaluated the patients with ocular trauma and retinal detachment.Jacobsen et al[2]evaluated 109 patients to compare the accuracy of diagnosing retinal detachment by an ophthalmologist to that by an emergency physician who is not well trained in the visualization of the retinal periphery and diagnose it by using point focused ultrasound. Among the 34 patients confirmed as retinal detachment by an ophthalmologist, 31 patients were found to have retinal detachment on ultrasound by an emergency physician. Similarly, Horowitz et al[3]discussed ultrasound fi ndings in two cases, the fi rst case had an intraocular foreign body and the second case had an increased optic nerve sheath diameter. In the first case, a diagnosis of intra ocular foreign body was made whereas in the second case, on further assessment,a diagnosis of pseudotumor cerebri was made. These cases highlight the valuable role of point focused ultrasound in emergencies. Ultrasonography helps not just in diagnosing ocular conditions but sometimes can give a clue towards the presence of a systemic illness.Abu-Zidan et al[4]discussed the posterior segment and periocular ultrasound findings in a case of severe posttraumatic eye with externally impinging foreign body. Similarly, other studies[5–7]have evaluated the accuracy of ultrasound in detecting acute posterior segment pathologies such as retinal detachment,retinal tear, vitreous hemorrhage and posterior vitreous detachment. An early detection of the above conditions can help in appropriate referral, early management and visual rehabilitation.
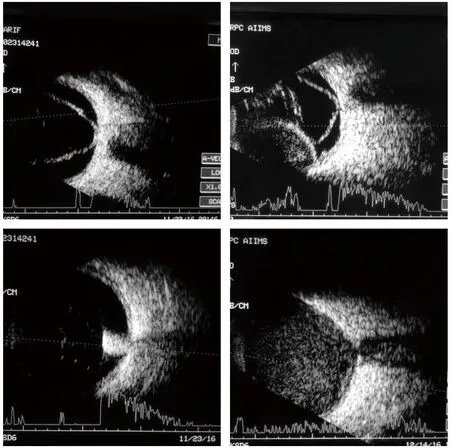
Figure 1. Various posterior segment pathologies showed by ultrasonography.A: High amplitude membranous echo with little after movements attached to the optic disc and persisting till low gain suggestive of retinal detachment; B: Similar findings as retinal detachment along with thick double peak dome-shaped elevation not extending beyond the equator is suggestive of choroidal detachment; C: Inferior high amplitude localized spike with shadowing is suggestive of retained intraocular metallic foreign body; D: Mild to moderate amplitude dot like echoes fi lling the entire vitreous cavity following trauma is suggestive of vitreous haemorrhage.
Our study mainly evaluated the paediatric population presenting to the ocular emergency services. All children were thoroughly assessed by a single paediatric ophthalmologist in the emergency service and in cases where posterior segment pathology was suspected,a detailed posterior segment ultrasonography was performed by the same surgeon (with more than 1.5 years of experience in performing ultrasound under such a scenario). Among the 122 patients included in the study,defi nitive posterior segment pathology was delineated in a significant proportion of the cases. More importantly,vision-threatening, as well as a life-threatening condition like posterior segment tumors, was ruled out by a detailed screening of all the quadrants of the posterior segment.
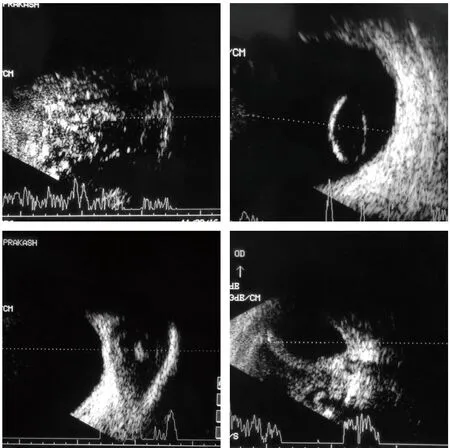
Figure 2. Ultrasonographic evaluation for nontraumatic concerns. A:Diffuse intravitreal mass with internal localized high amplitude spikes are suggestive of specs of calcification in case of retinoblastoma;B: Posteriorly dislocated relatively biconvex structure with internal hollowness is suggestive of posteriorly dislocated lens; C: Well defi ned cystic lesion within an extraocular muscle having a localized high amplitude spike is characteristic of cysticercosis; D: In a case of a severely traumatized eye showing irregularity and discontinuity along the posterior ocular coats.
Ultrasound in these cases was repeatable with almost consistent findings. Postoperatively, all cases were assessed by the same surgeon to avoid inter-observer variation. Cases with endophthalmitis were immediately managed by a retina expert by giving intravitreal injection after ruling out retinal detachment or early surgical intervention in the form of pars plana vitrectomy.Corneal ulcer cases that had anechoic posterior segment were immediately subjected to obtain tissue specimen for culture and antibiotic sensitivity followed by initiation of appropriate antibiotic therapy. Suspected Retinoblastoma cases were screened bilaterally using ultrasound and were followed by immediate contrast-enhanced imaging of the brain and orbit followed by evaluation under anaesthesia to stage the tumour.
Two cases with periorbital hemorrhage showed welldefined cystic masses with an internal eco lucent area.After obtaining contrast-enhanced computed tomography of the orbit and head a defi nite extent of hematoma was made. Subsequently these patients under needle guided drainage by the same surgeon under feasible anesthesia.Acute lymphoblastic leukemia commonly presented with subconjunctival hemorrhage, rhe retinal examination in these cases revealed subhyaloid and retinal hemorrhage but without any orbital hematoma on the ultrasound.These cases were referred back to the respective physician for further systemic stabilization.
Two cases of paediatric cataracts were planned for early surgery by a paediatric cataract surgeon. There was one case of cryptophthalmos which revealed absent globe on one side and a microphthalmic globe on the other side. The patient underwent lid reconstruction procedure within a week after systemic stabilization.Out of the seven extraocular muscle cysticercosis cases, one patient was diagnosed to have intracranial cysticercosis after a computed tomographic evaluation of the brain and orbit. She was referred and managed under neurologists’ observation. The remaining six cases who had only extraocular muscle cysticercosis received oral albendazole 15 mg/kg in two divided doses along with oral prednisolone acetate 1 mg/kg over a period of 4 to 6 weeks depending upon the response on serial ultrasounds after every fi fteen days.
CONCLUSION
To conclude, paediatric patients presenting to ocular emergencies can have sight threatening disorders affecting the posterior segment as well as the orbit.These can be optimally managed by a systematic clinical approach. However, with addition of first point of care posterior segment and orbital ultrasound in the evaluation protocol of these cases the visual and clinical outcome can be signifi cantly improved.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors declare that there are no confl icts of interest regarding the publication of this paper.
Contributors:AP proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
 World journal of emergency medicine2018年4期
World journal of emergency medicine2018年4期
- World journal of emergency medicine的其它文章
- Social attitude and willingness to attend cardiopulmonary resuscitation training and perform resuscitation in the Crimea
- Sub-dissociative dose ketamine administration for managing pain in the emergency department
- Effect of sedative agent selection on morbidity,mortality and length of stay in patients with increase in intracranial pressure
- Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology
- Accuracy of abdominal ultrasound for the diagnosis of small bowel obstruction in the emergency department
- Estimating the weight of children in Nepal by Broselow, PAWPER XL and Mercy method
