Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology
Elaine Situ-LaCasse, Ryan W. Grieger, Stephen Crabbe, Anna L. Waterbrook, Lucas Friedman, Srikar Adhikari
1 Department of Emergency Medicine, Banner University Medical Center, Tucson, AZ, USA
2 The University of Arizona College of Medicine, Tucson, AZ, USA
3 Department of Emergency Medicine, The University of Arizona, Tucson, AZ, USA
4 University of California Riverside, Riverside, CA, USA
KEY WORDS: Point-of-care ultrasound; Musculoskeletal; Emergency department
INTRODUCTION
Physician-performed point-of-care ultrasound(POCUS) has become more prevalent over recent decades in the evaluation of patients presenting with musculoskeletal symptoms to the emergency department(ED). In 2008, a study using Medicare data determined that of 30% of all diagnoses made using magnetic resonance imaging (MRI) could have been diagnosed using ultrasound.[1]In the recent years, the role of POCUS has continued to evolve. The utility of POCUS to accurately diagnose musculoskeletal injuries, obtain appropriate consultation, and perform interventional procedures in the ED has been demonstrated in previous studies.[2–4]Where traditionally radiography, computed tomography (CT), and MRI imaging studies have been the gold standard for evaluating musculoskeletal complaints, recent studies have demonstrated that POCUS can be used to confidently rule out long bone fractures and metatarsal fractures, detect ankle ligament and Achilles tendon injury, evaluate for suspected joint effusions,and distinguish abscesses from cellulitis.[5–8]Unlike MRI, clinicians can rapidly evaluate musculoskeletal symptoms at the bedside with ultrasound and also perform dynamic assessment of muscles, tendons, and ligaments. The sensitivity and specificity of point-ofcare musculoskeletal ultrasound for the diagnosis of long bone fractures in the ED are 90% and 96% respectively.[2]It has also been shown that emergency physicians can diagnose extremity tendon injuries with POCUS with 100% sensitivity and 95% specifi city.[9]
The advantages of POCUS compared to other imaging modalities such as absence of radiation,improved patient safety, real-time image acquisition,and relatively low cost of imaging have been well documented.[10–15]Therefore, POCUS allows for the emergency physician to make appropriate medical decisions for patient care by using real-time images in a safe and cost-effective way. However, to our knowledge,no study to date has investigated the direct impact that POCUS has on the medical decision-making of the emergency physician in patients presenting with musculoskeletal complaints. The purpose of this study was to evaluate the utilization of POCUS for assessment of ED patients presenting with musculoskeletal symptoms and the impact of musculoskeletal POCUS on medical decision-making and patient management in the ED.
METHODS
Study design and study setting
This was a retrospective review of ED patients presenting with musculoskeletal symptoms who received a POCUS over a 3.5-year period from November 1, 2013 through May 30, 2017. This study includes musculoskeletal POCUS studies performed at two urban academic EDs totaling approximately 110,000 patient visits per year. Both EDs have an Accreditation Council for Graduate Medical Education (ACGME)-accredited Emergency Medicine residency program. One ED has an additional five-year combined Emergency Medicine/Pediatrics residency program and an Emergency Ultrasound fellowship training program. The residents receive ultrasound training per ACGME guidelines. The attending physicians completed Emergency Medicine residency training and are board certifi ed in Emergency Medicine. The attending physicians had previously taken a standardized 16-hour course on emergency ultrasound that included didactics and hands-on training dedicated to musculoskeletal ultrasound. The physicians had performed an average of 50 musculoskeletal ultrasound examinations before the study. Hospital-based credentialing in POCUS is available for ED attending physicians at both sites and was derived from American College of Emergency Physicians ultrasound guidelines.Musculoskeletal POCUS examinations were performed by both Emergency Medicine residents and attending physicians.
All POCUS examinations were archived in the webbased workflow solutions database, Qpath (Q-path,Telexy Healthcare, BC, Canada), and quality assurance of all the studies were performed by either Emergency Ultrasound fellows or Emergency Ultrasound fellowshiptrained emergency physicians. This database stores all POCUS examinations performed at both EDs, including interpretation reports detailing indications, findings,and final diagnoses, which accompany each POCUS examination. Institutional board review approval was obtained for this study.
Study population/inclusion criteria
Patients were included in the study if they received a musculoskeletal POCUS examination in the ED and if it was used for medical decision-making. No specific ED POCUS protocol for evaluating musculoskeletal symptoms was followed. Patients received musculoskeletal POCUS when credentialed emergency sonologists were on duty. POCUS is not routinely used in our ED to detect fractures.
Study protocol
Qpath database was initially queried for eligible subjects who received musculoskeletal POCUS examinations followed by electronic medical record review. Pediatrics patients, patients with incomplete data, and those whose POCUS was not mentioned in the physicians’ medical decision-making were excluded from analysis.
A total of three chart reviewers performed data abstraction using a standardized data extraction form. The data extraction form included information about demographic characteristics, history, physical examination findings, ED course, POCUS findings,additional imaging studies, impact of musculoskeletal POCUS on patient management in ED, disposition, and repeat visits to ED. Impact of musculoskeletal POCUS on patient management was defi ned as the ED providers’decision to perform invasive procedures, order further imaging, request consultation, order antibiotics, and decide to admit or discharge the patient.
Statistical analysis
Descriptive statistics were used to summarize the data. Continuous data were presented as means with standard deviations, and dichotomous and nominal data were presented as percentage frequency of occurrence.The proportion of patients whose treatment plan was altered by the addition of musculoskeletal POCUS was determined.
RESULTS
A total of 264 subjects (92 females, 172 males) and 292 musculoskeletal POCUS studies were included in the fi nal analysis. The mean age was 48.26±18.97 years(range 18–98).
Pain was the most common symptom (76.1%),followed by swelling/edema/effusion (27.7%) to warrant musculoskeletal POCUS study.
Most common symptomatic sites were knee (31.8%)and ankle (16.3%). The POCUS fi ndings are summarized in Table 1. Joint effusion was the most common fi ndingon musculoskeletal POCUS, noted in 33.7% of the patients, and subcutaneous edema/cobblestoning was found in 10.2% of the patients. Muscle or tendon rupture was found in 2.3% of the patients, and 1.9% of the patients had joint dislocation. Bursitis or bursa fl uid was found in 3.4% of patients, and tendonitis/tendinopathy was found in 2.3%.
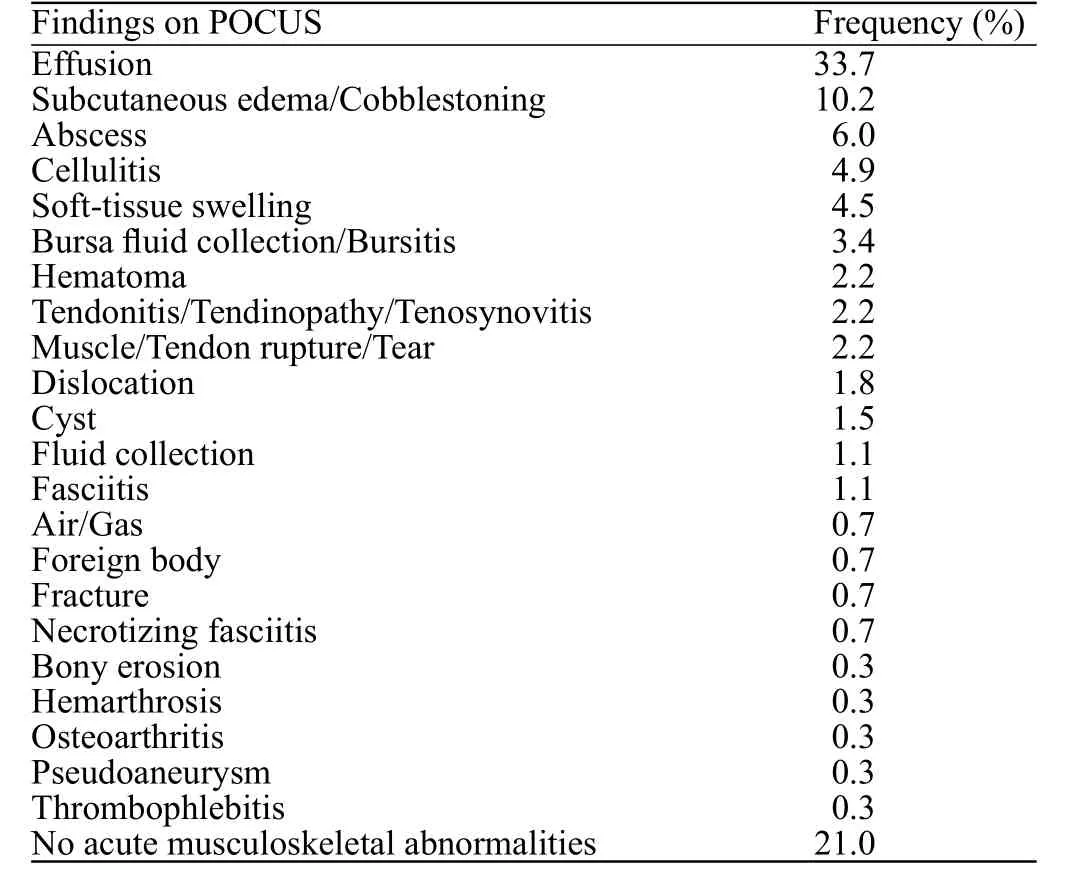
Table 1. Musculoskeletal POCUS fi ndings (n=264)
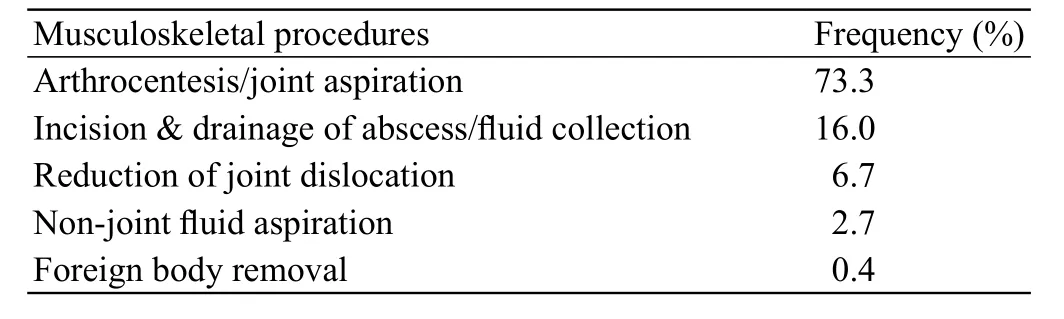
Table 2. Musculoskeletal procedures performed based on POCUS fi ndings (n=75)
Of the 292 musculoskeletal POCUS studies, 20%of them were ultrasound-guided musculoskeletal procedures, and most of them were arthrocentesis. The majority of them were knee arthrocentesis with other procedures being shoulder dislocation reduction and intra-articular injection of anesthetic agents.
Of the 234 diagnostic musculoskeletal POCUS studies performed (which excludes ultrasound-guided procedures), all except three cases either changed or helped guide patient management as documented in the patients’ electronic medical records. Because of the POCUS, 134 unnecessary joint aspirations or incisions and drainage procedures were avoided. In 75 cases,musculoskeletal procedures were performed by the emergency physician, due to findings seen on POCUS(Table 2). In 18 cases, the POCUS findings directly prompted the physician to consult a specialty service or admit the patient for further inpatient management. Of the patients who received a musculoskeletal POCUS,18.2% were admitted to hospital, only 8.3% of patients returned to the ED for the same complaint within 30 days, and 27.3% of patients subsequently followed up in our hospital system as an outpatient.
DISCUSSION
Patients with musculoskeletal complaints are often evaluated in the ED.[16]Derlet et al[17]found that joint pain was the most common symptom among ED patients presenting with musculoskeletal symptoms. This is consistent with the results of our study, with pain being the most common symptom warranting a musculoskeletal POCUS. However, the differential diagnosis for musculoskeletal pain is extensive, from joint effusion to thrombophlebitis, and POCUS can be key in making the accurate diagnosis while ruling out other possibilities.Our study findings illustrate the use of POCUS in the evaluation of a variety of musculoskeletal pathologies.This adds to the growing research demonstrating the importance of POCUS on patient safety, patient satisfaction, patient throughput, cost-effectiveness,and POCUS utility in a wide array of musculoskeletal applications.
POCUS plays a critical role in screening for pathology and has the advantage over other imaging modalities of being able to perform a dynamic assessment, which can be critical when evaluating musculoskeletal pathology. For instance, actively ranging a ligament or tendon while performing a POCUS can help clarify the extent of a rupture or tear. POCUS is performed rapidly at the patient’s bedside, which can be critical in disease states such as identifying necrotizing fasciitis from cellulitis; diagnosing pyomyositis,thrombophlebitis or pseudo-aneurysm from abscess; and bursitis from septic arthritis. Additionally, POCUS has been shown to be a relatively inexpensive diagnostic modality compared to other imaging, such as magnetic resonance imaging and computed tomography. POCUS can also direct health care providers to more appropriate imaging modalities. In our study, there were three cases in which the providers elected to pursue additional imaging studies after the POCUS. Two of the three patients had MRIs ordered afterwards to look for musculoskeletal pathology.
Previous studies have documented the diagnostic and treatment benefits of ultrasound with musculoskeletal procedures such as arthrocentesis, joint loading,abscess drainage, and nerve blocks. The most common musculoskeletal application that we identifi ed, evaluating for joint effusions, has been shown in prior research to be accurately diagnosed by ultrasound.[18]In fact, the use of POCUS has been documented to change management,prompting physicians to perform an arthrocentesis or abandon plans to do so based on sonographic findings.[5]This study further demonstrates this as all except three of the included musculoskeletal POCUS examinations included in our study either changed or helped guide patient management. Physicians often encounter physical examination findings such as erythema, induration, and fluctuance overlying a joint that may mimic a septic arthritis, but POCUS can confirm the presence of an effusion, which provides the patient and physician with stronger evidence for undergoing the risk, pain, and time of an invasive procedure.[7]The vast majority of management changes due to POCUS in our study was the decision to perform a procedure or not, such as joint aspiration or incision and drainage. Ensuring appropriate therapy requires synovial fluid analysis for patients with a joint effusion and for the study’s patients who ultimately did not have a joint effusion as determined by POCUS, they were spared an unnecessary invasive procedure and its associated risks.[19]POCUS further aids in patient safety as a tool for procedural needle guidance.In this study, 20% of the 292 ultrasound examinations included were ultrasound-guided procedures. Ultrasound needle guidance reduces the number of attempts and decreases patient-reported pain compared to landmark technique and maximizing the amount of fl uid removed during an arthrocentesis.[20]
A majority of prior studies investigated the accuracy of POCUS in diagnosing musculoskeletal pathology,primarily fractures, and joint effusions. Our study investigates the utilization of POCUS in diagnosing a wide variety of musculoskeletal pathology in ED.Additionally, we studied the impact of musculoskeletal POCUS on medical decision-making and patient management in ED with different musculoskeletal conditions. This highlights the advantages of incorporating musculoskeletal POCUS in the assessment of ED patients, changing management, and/or patient disposition, all while performing these studies in real time at bedside, potentially improving patient safety,length of stay, and cost effectiveness.
Limitations
This study has multiple limitations, with one being its retrospective study design and also small sample size, which can limit the conclusions that can be reached. Other limitation of this study is the selection bias from the convenience sample design,since patients received musculoskeletal POCUS only when credentialed emergency sonologists were on duty. The chart reviewers were not blinded to the study hypothesis and results; we attempted to reduce the bias in data collection by using a standardized data abstraction form. We also did not review inpatient charts documenting impact of musculoskeletal POCUS on the admitting team’s patient management. Prior literature highlights the need for POCUS to further penetrate the non-academic community ED practice environment. Although one of the two ED sites included in this review was considered a community ED, both are staffed by emergency medicine residents and academic emergency medicine attending physicians that work at the other large referral University hospital.There is also an Emergency Ultrasound fellowship program at this institution, so the physicians there are not only more experienced, but also more driven to perform musculoskeletal POCUS. Consequently, the practice patterns are not necessarily generalizable to the community ED. Additionally, our sample does not include the diagnosis of fractures. However, there is an abundance of literature on the topic of fractures.Further research showing the impact of musculoskeletal POCUS is needed to support its application and fully realize its potential benefi ts on patient care in the ED.
CONCLUSIONS
In conclusion, despite the limitations, our study fi ndings illustrate the utility of POCUS in the evaluation of a variety of musculoskeletal pathologies in the ED. Our study suggests that musculoskeletal POCUS positively impacts patient management not only in the diagnosis of musculoskeletal pathology, but also in the performance of musculoskeletal procedures.
Funding sources:None.
Ethical approval:Institutional board review approval was obtained for this study.
Confl icts of interest:Authors have no fi nancial or other confl icts of interest related to this submission.
Contributors:ES proposed the study and wrote the fi rst draft. All authors read and approved the fi nal version of the paper.