Accuracy of abdominal ultrasound for the diagnosis of small bowel obstruction in the emergency department
Sarah E. Frasure, Amy F. Hildreth, Raghu Seethala, Heidi H. Kimberly
1 George Washington University Hospital, Washington DC 20037, USA
2 Naval Medical Center San Diego, San Diego, CA 92134, USA
3 Department of Emergency Medicine, Brigham and Women’s Hospital, Boston, MA 02115, USA
KEY WORDS: Abdominal ultrasound; Small bowel obstruction; Emergency department
INTRODUCTION
Patients frequently present to the emergency department (ED) with symptoms concerning for small bowel obstructions (SBO). Typically, ED providers obtain an abdominal computed tomography (CT) scan to confi rm the diagnosis prior to admission to the hospital.Indeed, CT imaging is the current gold standard for the diagnosis of SBO.[1,2]A few studies including a recent systematic review and meta-analysis by Gottlieb et al[3,4]have examined the use of ultrasound to diagnose SBO,an intriguing concept, as an ultrasound can be performed at the bedside, does not emit ionizing radiation, and is very helpful in low-resource settings. None of these studies included ED midlevel providers performing the ultrasound. Certainly, the use of ultrasound to accurately diagnose SBO in the ED could potentially reduce the length-of-stay of stable patients in the ED, reduce healthcare costs by limiting the use of CT imaging,and reduce patient exposure to ionizing radiation.The majority of patients with recurrent SBOs are conservatively managed with nasogastric tube (NGT)insertion, bowel rest, and IV fluids, and do not require operative intervention.[5–7]Theoretically, if a rapid, noninvasive ultrasound can accurately identify a SBO with similar accuracy to CT imaging, stable patients (normal vital signs, pain relief with NGT and IV analgesia)could potentially be expeditiously admitted to the hospital, avoiding the need for a CT scan in the ED. If a patient’s condition fails to improve over the course of the hospitalization, he/she could then undergo CT imaging. The primary aim of this study was to evaluate the accuracy of point-of-care ultrasound compared to abdominal CT in the assessment of patients by a variety of providers (attending physicians, ultrasound fellows,residents, and physician assistants) with suspected small bowel obstructions in the ED.
METHODS
Subjects and study protocol
This was a retrospective, single-center cohort study in a large tertiary care academic center with >65,000 yearly patient visits. The ED is affiliated with an emergency medicine residency program. The ED is also associated with a large cancer institiute with 230,000 outpatient visits per year. Many of our ED patients have active malignancy and, thus, risk factors for SBO.All point-of-care ultrasound images obtained in the ED are reviewed on a weekly basis by members of the emergency ultrasound division for quality assurance and are stored in a secure database. We utilized this database to search for all patients who underwent point-of-care abdominal ultrasound in the ED between September 2015 and September 2016 for suspected small bowel obstruction.
Ultrasound protocol: As part of the point-of-care ultrasound curriculum in our emergency department,residents, physician assistants, and ultrasound fellows are taught how to perform point-of-care ultrasound to evaluate for acute abdominal pathology. Our standardized scanning protocol to assess for SBO includes the following: All four quadrants of the abdomen are scanned using a curvilinear transducer at an imaging depth of 12-18 cm. Video clips of peristalsis and still images with appropriate measurements of the bowel in all four quadrants are saved. Our ultrasonographic criteria of a small bowel obstruction on point-of-care ultrasound include dilated (>2.5 cm) fl uid-fi lled loops of bowel and abnormal ‘back-and-forth’ peristalsis (Figure 1). Our providers are encouraged to perform a point-ofcare ultrasound on patients in whom the diagnosis of obstruction is expected, however, the use of ultrasound is at the discretion of the provider.
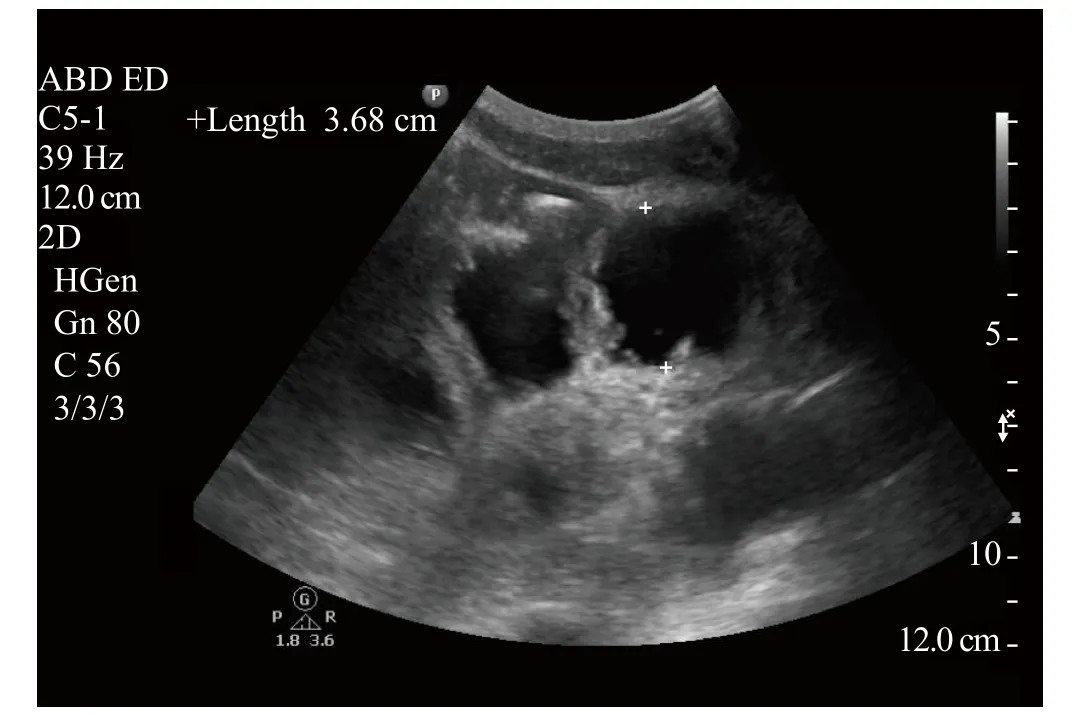
Figure 1. Example of a fl uid-fi lled loop of small bowel that measures 3.68 cm in diameter.
Computed tomography: abdominal/pelvic CT from the same ED visit were reviewed and abstracted. The CT scans were read by attending radiologists and considered positive if read as SBO, partial SBO, or early SBO. Patients were excluded from the chart review if they presented to the ED from another facility with CT imaging that already confi rmed the diagnosis of small bowel obstruction.
Medical chart review: we recorded the type of provider who performed the study (physician assistant, resident,ultrasound fellow/faculty) and his/her interpretation of the study. We also documented patient demographic characters including age, gender, history of prior SBO,abdominal surgery within two weeks of ED presentation,active malignancy, type of malignancy, abdominal/pelvis CT results, and whether the patient was conservatively managed or underwent an operation during the hospitalization. The chart review was performed by SF.This study was approved by the hospital’s Institutional Review Board (IRB) with waiver of informed consent.
Data analysis
The demographics were characterized using descriptive statistics. The distributions of continuous data were examined and found to be slightly skewed.As a result, continuous variables were reported as medians with interquartile ranges. Dichotomous variables were reported as frequencies and percentages.Sensitivity, specifi city, positive, and negative likelihood ratios were calculated using CT diagnosis as the gold standard. In accordance with the Standards for Reporting of Diagnostic Accuracy (STARD) steering group recommendations, 95% confi dence intervals were calculated for the measures of diagnostic accuracy and reported as well.[8,9]The data were analyzed using Stata SE, version 14.2 (StataCorp, Texas, USA 2015).
RESULTS
Table 1 demonstrates the baseline characteristics of the 64 patients who had a point-of-care abdominal ultrasound in the ED to assess for a SBO. The mean age was 58.8 years and 34.4% of our patients were male. Half of our patients had a prior SBO and 62.5%of all subjects had a history of active malignancy. 55 out of 64 patients underwent CT imaging, those nine patients that did not undergo CT imaging were excluded from primary analysis. Additionally, 8 patients had indeterminate ultrasound fi ndings, and so were excluded from the primary analysis. Indeterminate scans typically demonstrated dilated loops or abnormal peristalsis but not both. Of the 8 indeterminate scans, one was found to have an SBO on CT and seven were not. Thirty-two(50%) patients had small bowel obstructions identified on CT imaging and 28 (88%) were treated conservatively while 4 (12%) patients were taken to the operating room.
Table 2 shows the performance characteristics of point-of-care ultrasound for SBO for the 47 patients who underwent both point-of-care abdominal ultrasound and CT in the ED. Our data demonstrated a sensitivity of 93.8% (95% CI 79.2%–99.2%) and a specificity of 93.3% (95% CI 68.1%–99.8%) of ultrasound compared to CT imaging. Table 3 demonstrates the diagnoses of patients who did not have a SBO on CT. A total of 9 patients did not undergo CT imaging in the ED after their point-of-care ultrasound study. Table 4 represents their final ‘discharge diagnoses’ per medical record review.We performed a secondary analysis of performance characteristics of point-of-care ultrasound for SBO using the data from those 9 patients that did not ultimately undergo CT scan by using the gold standard of a composite of either CT scan or fi nal discharge diagnosis(Table 5). Our data showed a sensitivity of 93.8% (79.2%–99.2%) and a specificity of 95.2% (76.2%–99.9%) of ultrasound compared to a composite endpoint of CT plus final discharge diagnosis. The 64 point-of-care ultrasounds were performed by physician assistants(22%), emergency medicine residents (58%), and ultrasound fellows/faculty (20%). A subgroup analysis was not performed given how few patients were included in the study.
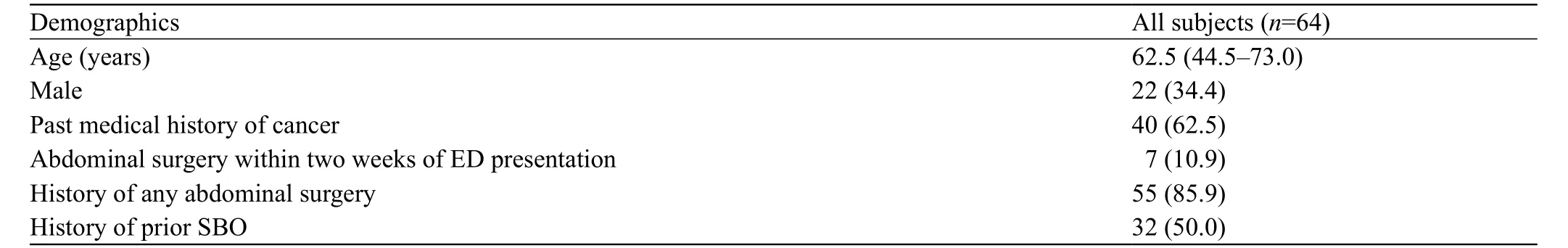
Table 1. Baseline characteristics
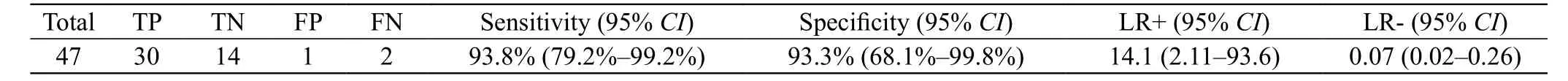
Table 2. Performance characteristics of bedside US for SBO compared to abdominal CT
DISCUSSION
Despite limited data regarding its accuracy, plain radiography was historically viewed as the initial imaging study of choice in patients with a suspected SBO. Recently, the poor sensitivity and specificity of plain radiographs to make the diagnosis of SBO has called into question the routine use of this imaging modality as a first-line tool in the ED in patients in whom SBO is suspected.[10,11]In order to assess the utility of different imaging modalities to diagnose SBO, Jang et al[4]enrolled 76 ED patients who were suspected to have a small bowel obstruction based on their symptoms. All patients underwent plain film imaging, point-of-care ultrasound, and CT imagingin the ED. Sonographic findings suggestive of a SBO were described as fluid-filled dilated bowel 2.5 cm or decreased/absent bowel peristalsis. Whereas abdominal plain films demonstrated a sensitivity and specificity of 46.2% and 66.7% respectively, point-of-care ultrasound demonstrated a sensitivity of 93.9% and specificity of 81.4% for SBO compared with CT. In 2017 Gottlieb et al[12]published a systemic review and meta-analysis of the use of ultrasound to evaluate SBO. The authors identifi ed 11 studies with 1,178 patients – the providers who performed the ultrasounds included emergency physicians, surgeons, and radiologists. In this systematic review ultrasound was found to be 92.4% sensitive and 96.6% specific for SBO. In our study, however,only clinicians in the emergency department (physician assistants, residents, emergency ultrasound fellows,emergency ultrasound faculty) performed the point-ofcare ultrasound. To our knowledge this is the fi rst study to include physician assistants as ultrasound operators in the ED. Our data demonstrated a sensitivity of 93.8%and a specifi city of 93.3% when compared to abdominal CT, and a sensitivity of 94.3% and specificity of 95.2%using a composite endpoint of abdominal CT and discharge diagnosis. Using a broad range of emergency providers, our results compare similarly to prior studies,suggesting that ultrasound can play an important role in the identification of small bowel obstructions in ED patients.
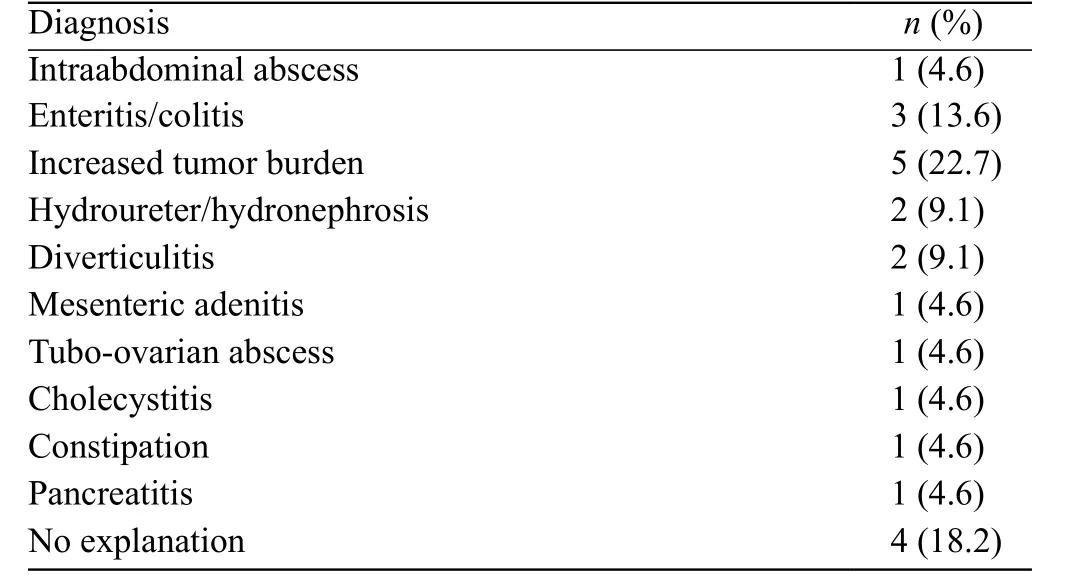
Table 3. Final diagnosis in patients with a negative CT for SBO
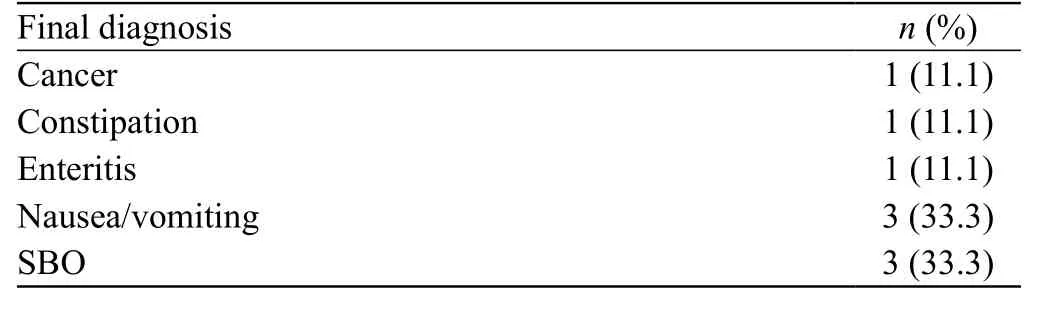
Table 4. Final discharge diagnosis if no CT done
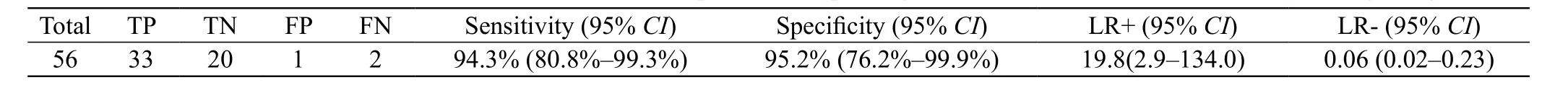
Table 5. Performance characteristics of bedside US for SBO compared to composite gold standard of abdominal ct or fi nal discharge diagnosis
Certainly point-of-care ultrasound is an attractive imaging modality as it can be performed at the bedside by the provider within a few minutes of meeting a patient and can identify many other causes of abdominal pain(gallstones, abdominal aortic aneurysm, appendicitis,hydronephrosis suggestive of a kidney stone, or intraabdominal free fluid). In addition, ultrasound is likely to be the only imaging tool that is readily accessible in low resource settings, making it particularly useful when assessing a patient for a SBO when CT is either not available or prohibitively expensive. Ultrasound is limited, however, in its ability to detect the transition point of a bowel obstruction and as such may not be adequate for operative planning.
In a previous retrospective chart review we examined 370 charts of patients who had been admitted to our hospital with a diagnosis of SBO over a two-year period.[5]Patients with a prior SBO were less likely to undergo operative intervention (20.3% [42/207]) compared to those without a prior SBO (35.2% [57/162]). Abnormal bloodwork(leukocytosis and lactic acid) did not predict which patients would require an operation. Patients with active malignancy were just as likely as other patients to go to the operating room – but did so nearly 2 days later.This delay in operative management may be explained by the higher post-operative morbidity in oncology patients.[13]In our current study, we also evaluated how many patients had a history of recent abdominal surgery,malignancy, and/or prior SBO. We examined how many patients required operative intervention during their hospitalization. Of the 32 small bowel obstructions that were identified on CT imaging, 28 (88%) were treated conservatively and 4 (12%) patients were taken to the operating room. Of the 28 patients who were treated conservatively with NGT and bowel rest, 17 (53%) had a prior SBO. Perhaps stable patients with a documented prior SBO, who have sonographic evidence of a SBO (fluid-filled dilated loops of bowel ³ 2.5 cm and decreased/absent peristalsis), and whose pain is wellcontrolled in the ED, could be expeditiously admitted to the hospital for a trial of conservative treatment. CT imaging in the ED would be reserved for toxic-appearing patients, those without a prior history of SBO, and those patients in whom the point-of-care ultrasound is nondiagnostic. Further prospective studies are potentially warranted and could help to create a clinical decision rule incorporating patient characteristics with bedside ultrasound.
Limitations
There are several limitations to our study. The sample size of our study population was small. Our data was obtained through a retrospective chart review with a single-center cohort. Our providers (physician assistants, emergency medicine residents, ultrasound fellows, faculty members) have varied experience levels with point-of-care abdominal ultrasonography.8/64 (13%) of the ultrasounds performed were deemed“indeterminate” by the performing provider. Operator dependence is a limitation to ultrasound for SBO. Most of the patients who are diagnosed with a SBO in our ED have active cancer. Our patient population, therefore,is not necessarily generalizable to other emergency departments. Not every patient in the ED in whom the provider suspects a SBO receives an abdominal pointof-care ultrasound prior to CT imaging and this may have introduced selection bias. A combination of factors including patient acuity, type of provider, individual provider interest in the use of ultrasound, perceived patient body habitus, and ED volume, often determine which patients undergo point-of-care ultrasound imaging.
CONCLUSION
Our results compare similarly to prior findings,suggesting that ultrasound can play an important role in the identifi cation of SBO in ED patients.
Funding:None.
Ethical approval:This study was approved by the hospital’s Institutional Review Board (IRB) with waiver of informed consent.
Confl icts of interest:No any benefi ts have been received from a commercial party related directly or indirectly to the study.
Contributors:SEF proposed the study and wrote the first draft.All authors read and approved the fi nal version of the paper. The work was performed at Brigham and Women’s Hospital, Boston MA, USA.