Effect of sedative agent selection on morbidity,mortality and length of stay in patients with increase in intracranial pressure
Brian G. Cornelius, Elizabeth Webb, Angela Cornelius, Kenneth W.G. Smith, Srdan Ristic, Jay Jain, Urska Cvek, Marjan Trutschl
1 Department of Anesthesia, University Health-Shreveport, Louisiana, Louisiana 71103, USA
2 Department of Emergency Medicine, Louisiana State University Health Sciences Center, Shreveport, Louisiana 71103,USA
3 Laboratory for Advanced Biomedical Informatics, Department of Computer Science, Louisiana State University Shreveport, Louisiana 71115, USA
KEY WORDS: Ketamine; Intracranial hypertension; Craniocerebral trauma; Head injury; Intubation
INTRODUCTION
Trauma is the leading cause of death among young adults, specifically traumatic brain injury (TBI) can yield high morbidity and mortality.[1]Management of the TBI patient requires early intervention including aggressive stabilization of airway with attentiveness to maintaining optimum hemodynamic parameters. The goal is to maintain adequate cerebral perfusion pressure(CPP) and cerebral blood flow to salvage the fragile parenchymal penumbra.[2]Rapid sequence intubation(RSI) is often completed in the field or enroute to the emergency department. A variety of sedative agents(Benzodiazepines, Opioids, Barbiturates, Etomidate,Ketamine, Propofol) are used for the induction of general anesthesia. The intent is to prevent ongoing brain injury by optimizing ventilation. A secondary effect is to reduce cerebral metabolic rate and intracranial pressure.In appropriate dosages, all commonly used agents are capable of inducing anesthesia but agent selection may play a critical role in secondary effects. Provider preference and familiarity is a common deciding factor in this selection and may not provide the best benefi t for the patient. Although there is still debate regarding which induction agent is most appropriate, recent research in critical care medicine suggests that the choice of induction agent in a critically ill patient may affect patient outcome.[3]
Ketamine is an N-methyl-d-aspartate receptor antagonist, often used in RSI due to its rapid onset and lack of both adrenal suppression and hypotension, when compared with Etomidate and Propofol respectively.[4]However, information regarding its safety in TBI patients is limited due to historical under-use specifi cally in this patient population, based on prior literature reporting an increase in intracranial pressure (ICP).[5]Those initial studies utilized human subjects with known CSF outflow tract obstruction and therefore, one could argue, they are inapplicable to the general population.[6]Of note, the patients in these studies were allowed to breathe spontaneously while receiving Ketamine as a sole anesthetic during craniotomy.[7]Recent research suggests that Ketamine increases mean arterial pressure (MAP) and cerebral perfusion pressure(CPP) with minimal impact on intracranial cerebral pressure (ICP), and may be neuroprotective as it is decreases the release of glutamate.[8]While evidence driven practice has suggested increased use of Ketamine 15 years ago, change has been slow to come.[9]
A comprehensive literature review[10]revealed seven prospective studies evaluating Ketamine in head trauma. Three of the studies found a decrease in ICP with Ketamine bolus while two others found CPP and MAP increased resulting in less supportive therapy post intubation.[11]There were no significant adverse events identifi ed though outcome data was limited. Researchers have also questioned the role of other therapies commonly utilized during intubation of the head injured patient.[12]There is no evidence that pretreatment with lidocaine reduces ICP however administration of Fentanyl and Esmolol has been shown to block hemodynamic instability. The summary by Bucher et al[12]also proposed Ketamine as the ideal sedative agent in head trauma due to its neutral hemodynamic profile.In light of the recent change in opinion surrounding Ketamine, a local air transport service developed a protocol using Ketamine as their sedative for RSI in trauma. By utilizing this data in comparison with prehospital data of RSI with Etomidate and Midazolam,our goal is to demonstrate that TBI patients should not be excluded from the potential use of Ketamine for RSI.
METHODS
Study design and setting
This was a retrospective analysis utilizing EMR and scanned records from air medical transport of TBI patients who underwent prehospital RSI at the discretion of the air crew, prior to arrival to a Level 1 emergency department. The study period was from January 2014 through October 2015. University Health-Shreveport is the teaching hospital for the Louisiana State University Health Sciences Center-Shreveport (LSUHSC-S), a level one trauma center, children’s hospital and regional burn center serving a diverse geographical area to include Louisiana, Texas, Arkansas and Oklahoma. Several different scores were utilized for patient comparison[13,14]:Revised Trauma Score (RTS), Glasgow Coma Scale(GCS) (initial/ED arrival), Injury Severity Score (ISS),Trauma Injury Severity Score (TRISS) and Systolic Blood Pressure (SBP) (initial/ED arrival). The RTS is a physiologic score, composed of GCS, SBP and respiratory rate. A RTS less than 4 identifies significant injury that should be treated in a trauma center. The GCS is used as an objective measure of neurologic status, values were obtained from the initial provider and Emergency Department arrival. The ISS is an anatomical scoring system used to evaluate bodily injury and predict mortality, increase ISS correlates with increased morbidity and mortality. TRISS is utilized to determine the probability of trauma survival, it is calculated from the ISS and RTS, coupled with contributions for blunt vs.penetrating trauma and age. The primary objectives were to evaluate the effect of sedative administration selection on length of stay, morbidity and mortality. The length of stay (LOS) was evaluated from the time of trauma center admission to discharge. Morbidity was evaluated on the basis of discharge destination; home, long term care or death. Mortality was evaluated by the number of days from the time of insult to expiration. Patients were also evaluated for blunt versus penetrating insult. The use of adjunct agents including narcotics, sedative dosage and post intubation sedatives were not evaluated.
Study criteria
Patients were identified through EPIC Electronic Medical Record query of all patients intubated prior to facility arrival with evidence of intracranial hypertension.Intracranial hypertension was defined by abnormal head computerized tomography (CT) scan or increased intracranial pressure by invasive monitoring. Patients were intubated and transported by eight different flight programs with differing protocols. Ketamine was used by several services for induction per provider and program discretion. Study inclusion criteria: age >18, patient with suspected increase in intracranial pressure, patient arrived by air medical transport, endotracheal tube placed prior to arrival at LSUHSC-S, documentation of sedative medication administration. Exclusion criteria: age <18, pregnant female,intubated after arrival at LSUHSC-S, absence of sedative medication administration documentation.
Analysis
The ANOVA was conducted in R by separating the data into seven separate fi les corresponding to the seven continuous input variables. Each row contains the value of the respective variable as well as a group label where group 1 corresponds to Versed, group 2 corresponds to Etomidate, and group 3 corresponds to Ketamine.The P-values were calculated and subsequent t-tests with Bonferroni correction were conducted on initial Glasgow Coma Scale (initial GCS) and RTS. The initial GCS parameter had a statistically significant (<0.05)P-value of 0.017. The t-test with Bonferroni correction was also conducted on the Revised Trauma Score (RTS)parameter which had a P-value of 0.09, although not statistically signifi cant with our alpha value of 0.05. The t-tests with Bonferroni correction produced adjusted P-values to correct for Type I error in pairwise t-tests.The resulting output tables of the t-test with Bonferroni correction show comparisons between each of the three drug treatments. For the initial GCS parameter, there is a statistically significant (<0.05) P-value of 0.033 when Versed and Ketamine treatments were compared. For the RTS parameter, there was no statistically significant P-values between any of the drug treatments. Due to the retrospective nature of our study a post-hoc multivariable analysis was performed to obtain a less biased estimate of the effects.
Linear regressions on each drug were conducted for the two continuous outcomes: length of stay (LOS) and time of mortality. The input variables for both the length of stay and time of mortality outcomes included initial GCS, ED GCS, RTS, ISS, TRISS, initial SBP, and ED SBP.No linear regression was conducted on the time of mortality outcome for Ketamine as there were only two data points.
Subsequently, root mean squared error (RMSE)calculations were conducted to compare the observed and predicted values from the regressions. For the Ketamine LOS outcome, an RMSE value of 13.45 days was calculated where the mean length of stay was 29.5 days. For the Etomidate LOS outcome, a RMSE value of 15.33 days was calculated where the mean length of stay was 15.7 days. For the Versed LOS outcome, an RMSE value of 13.3 days was calculated where the mean length of stay was 14.1 days. Since no regression was done for the Ketamine time of mortality outcome, no RMSE was calculated. For the Etomidate time of mortality outcome,a RMSE of 1.29 days was calculated where the mean time of mortality was 1.9 days. For the Versed time of mortality outcome, and RMSE of 1.36 was calculated where the mean time of mortality was 5.6 days.
Additionally, three logistic regressions were conducted upon the discharge disposition outcomes, where the possible values are home, LTAC, and expired. The input variables for the logistic regression are the same as the linear regression except for the addition of the injury type (blunt or penetrating). Injury type was not used on the Ketamine logistic regressions because there was only one penetrating injury in the Ketamine group. The first logistic regression combined the home and LTAC outcomes and compared it to the expired outcome. The second logistic regression compared the home versus the LTAC outcome. The third logistic regression compared all outcomes versus each other. Each logistic regression was conducted upon each of the three drug treatments.
For the first logistic regression (home+LTAC vs. expired), the initial SBP regression coefficient was statistically significant (<0.05) for the Ketamine(P=0.027) and Etomidate (P=0.046) drug groups. For the second logistic regression (home vs. LTAC), the regression coefficients for TRISS (P=0.042) and initial SBP (P=0.40) were statistically signifi cant for Ketamine.For the third logistic regression (home vs. LTAC vs.expired), initial GCS (P=0.049), TRISS (P=0.012),and initial SBP (P=0.016) regression coefficients were statistically significant for Ketamine. Additionally, the TRISS (P=0.027) regression coeffi cient was statistically signifi cant for Etomidate.
The Aikaike Information Criterion (AIC) was calculated for all logistic regressions to compare models for quality of model fit and number of parameters while minimizing information loss.[14]For the first logistic regression, the Ketamine model had minimum informational loss with an AIC score of 7.89 when compared to Etomidate (60.1) and Versed (42.55). For the second logistic regression, the Ketamine model had minimum information loss with an AIC score of 13.91 when compared to Etomidate (53.89) and Versed (42.55).For the third logistic regression, the Ketamine model had minimum information loss with an AIC score of 24.56 when compared to Etomidate (110) and Versed (71.73).
RESULTS
Over the 22-month period, 148 patients were identifi ed as meeting inclusion criteria, 52 were excluded due to incomplete data. After exclusion for incomplete data, 96 patients remained, due to low sample number 7 patients that had received Ativan (2), Fentanyl (1),Propofol (2) and Valium (2) were excluded (total of 89 patients). Patients arriving as hospital transfers as well as those arriving directly from the scene were included. Patients received a variety of sedative agents for intubation to include; Ativan, Etomidate,Fentanyl, Ketamine, Midazolam, Propofol and Valium.The primary agents used: Etomidate (n=47, 48.9%),Midazolam (n=27, 28.1%) and Ketamine (n=15, 15.6%),were chosen for comparison (Tables 1–3).
DISCUSSION
It is well understood the need to maintain CPP in patients with elevated intracranial pressure. Previous research has shown that Etomidate can reduce intracranial pressure while maintaining blood pressure[14]thus improving CPP. However, there is increasing evidence that the administration of Etomidate results in transient adrenal suppression.[15]Past literature has also suggested to avoid Ketamine due to myocardial depressanteffects.[16]A case series of pediatric patients receiving Ketamine while simultaneously mechanically ventilated with ICP monitors found that Ketamine decreased ICP and blunted increases during stimulation without lowering CPP or blood pressure.[17]In our study the patients receiving Ketamine for intubation experienced minimal decrease in their systolic blood pressure between initial contact and ED arrival, signifi cantly less than the patients receiving Etomidate or Midazolam.This relation between systolic blood pressure and the Ketamine treatment is supported by the fi rst two logistic regressions that showed that the initial SBP value for Ketamine was statistically significant. This value resulted in artificial increase in the RTS and thus the TRISS upon hospital arrival. There was also a higher percentage of penetrating injuries in the Ketamine group. Excluding these noted figures, the stratification data is comparable. Most Ketamine studies have shown no increase in cerebral oxygen consumption.[18]This fi nding is critical to reduce secondary injury and improve long term outcome.
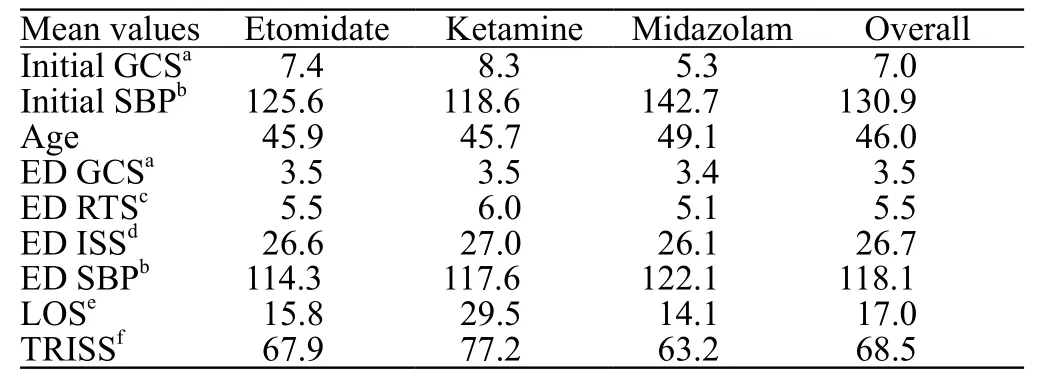
Table 1. Patient characteristic data
Key findings from the study were a longer length of stay for patients receiving Ketamine (# of days=15.8[E] 29.5 [K] 14.1 [M]) nearly double that of those receiving other medications. This is to be expected as patients with head injuries that survive and are not able to be discharged home often require rehab care post hospitalization, placement may result in prolonged admission.[19]There may also be additional requirements prior to placement to include tracheostomy and gastric tube placement. These interventions cumulatively add days to hospitalization. Patients receiving Ketamine demonstrate a substantially lower mortality rate %=38.3(E) 13.3 (K) 40.7 (M). Of note the patients that expired from the Ketamine group survived in the hospital 8.5 days which was longer than the other two groups 1.9 (E)5.6 (M). In reviewing discharge destination for the study groups, the number of patients being discharged home is equivalent 25.5 (E) 26.7 (K) 25.9 (M). However, the number being sent to Long Term Acute Care (LTAC) is quite different %=36.2 (E) 60 (K) 33.3 (M). There is an obvious shift, the patients that expired after receiving other sedatives instead survive after receiving Ketaminebut do require LTAC admission.
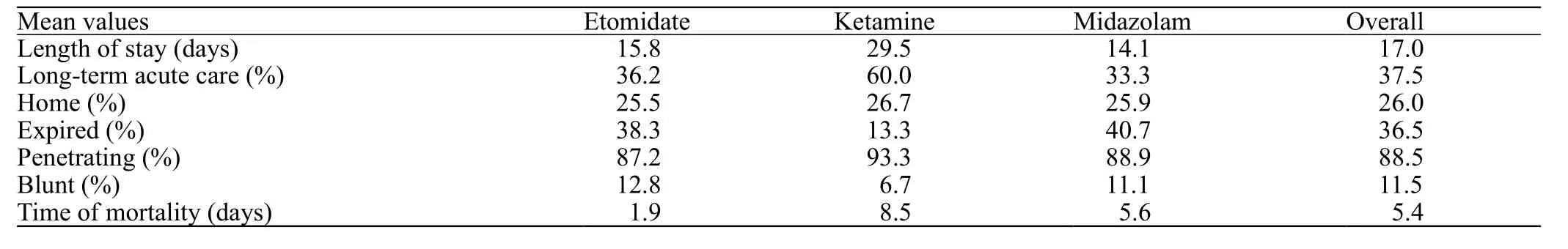
Table 2. Outcome data
This data also broaches the question of appropriate sedative selection for patients post intubation. The agents evaluated in this study are also commonly used for long term sedation in the intensive care unit. Propofol and Midazolam have routinely been used as a sedative infusion alone or in conjunction with Fentanyl.[20]Past research has indicated these sedatives result in similar outcomes.[21]A prospective trial of post-operative neurosurgical patients receiving Midazolam, Propofol and Fentanyl found a significant reduction in mean ICP when compared to Midazolam or Propofol alone.[22]Ketamine is routinely used as a multimodal analgesic and may provide benefit as a long-term sedative, either as a stand-alone agent or in conjunction with more traditional sedatives.[23]A recent study evaluated Ketamine for long term sedation as compared to opioids, midazolam and Propofol and found it resulted in the lowest incidence of cortical spreading depolarization.[24]Cortical spreading has been found to result in increased lesion expansion in cases of acute brain injury. As control of depolarization may reduce the impact of secondary brain injury,Ketamine may offer a neuro protective role for TBI.
The retrospective nature of this study results in limitations to the outcome data. Additionally, the low sample sizes reduces the statistical significance. This study included patients intubated by multiple air medical services, this creates potential disparity as there was little standardization in dosing regimen and adjunct medications used. Future randomized control trial would be benefi cial to reinforce the fi ndings of our study.
CONCLUSION
Previous practice and research that resulted in the avoidance of Ketamine in patients with elevated intracranial pressure was not evidence based. This study represented a stratifi ed retrospective analysis of patientswith intracranial hypertension undergoing endotracheal intubation prior to arrival at the tertiary care center.Agent selection appears to influence patient outcome,with Ketamine showing a reduced rate of mortality when compared to Etomidate and Midazolam. This is likely due to blood pressure maintenance achieved with the administration of Ketamine for induction. The reduction in mortality is exchanged for an increased likelihood of admission to long term care upon discharge. Ketamine shows great promise as a diverse agent for use in the care and management of patients with intracranial hypertension. Evidence indicates it can be safely used and should be considered in lieu of other medications in this patient subset. In conclusion, Ketamine should be used without concern for worsening outcomes in patient with elevated intracranial pressure requiring intubation.
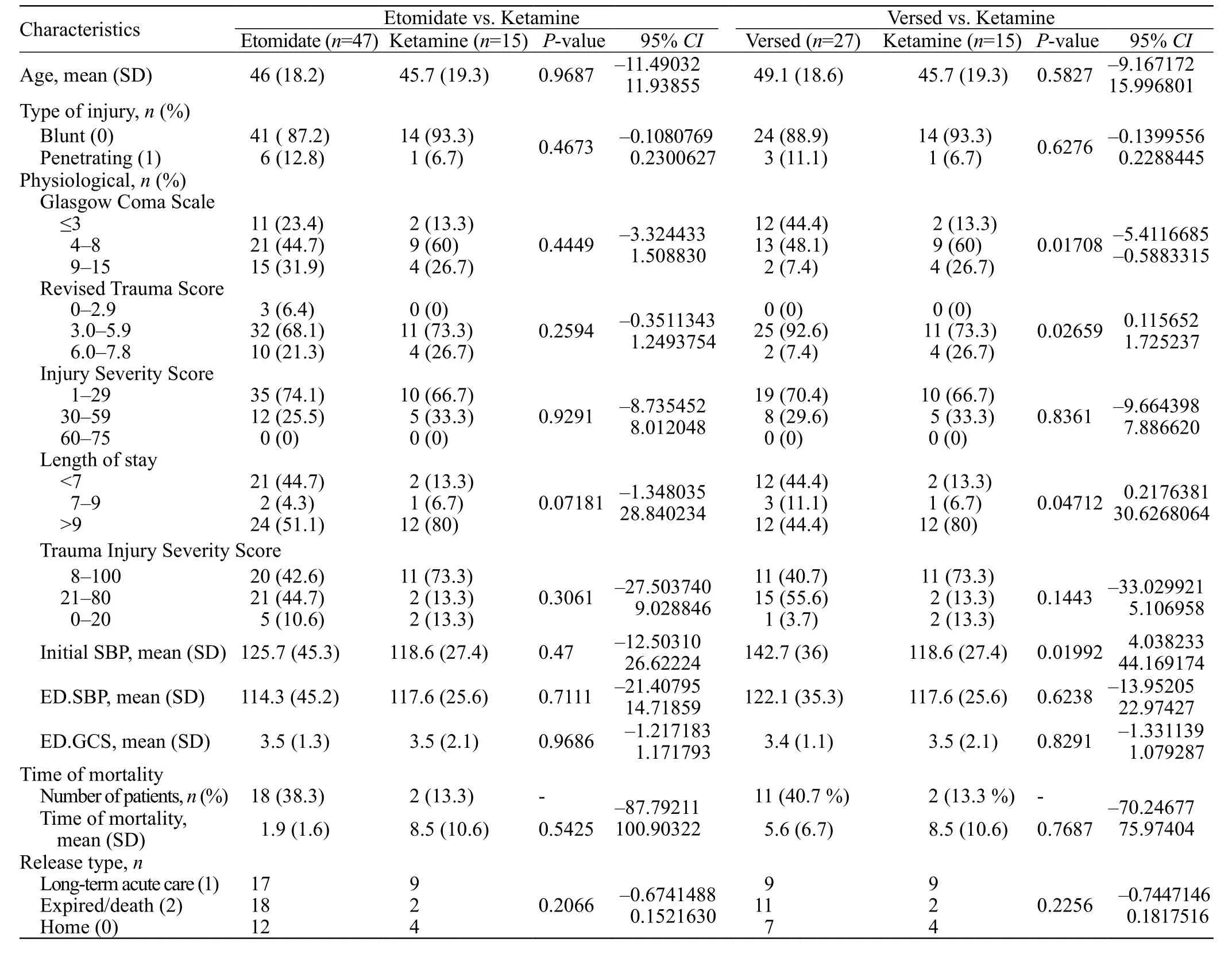
Table 3. Comparative P-values with 95% CI
Funding:None.
Ethical approval:This study was approved by the hospital’s institutional review board.
Confl icts of Interest:All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors have no independent disclosures or confl icts of interest.
Contributors:BC, EW, and AC: author, data collection; KS, SR,JJ, UC, and MT: statistical analysis.