溃疡性结肠炎与小肠细菌过度生长关系探讨
刘治宏,崔立红
1.陆军军医大学研究生院,重庆 400038;2.海军总医院消化内科
溃疡性结肠炎(ulcerative colitis, UC)表现为肠道慢性非特异性炎症,具有复发、缓解的病程特点。UC发病率较高[1],整体发病率为1.2~20.3例每年每100 000人,患病率为7.6~245例每年每100 000人[2]。患者通常出现血性腹泻和腹部绞痛等症状[3]。流行病学表明,UC发病率的升高伴随着社会西方化和工业化的进程,正如自1990年以来,UC在西方国家的发生率基本稳定,但在新兴工业化国家呈上升的趋势[4]。尽管有许多遗传和环境因素已被发现增加了该病的发病率[5],但UC的确切发病机制目前仍不明确。
小肠细菌过度生长(small intestinal bacterial overgrowth, SIBO)是外来细菌或肠道内常驻细菌数量增加导致的食物过度发酵、黏膜炎症、小肠通透性破坏、吸收不良、绒毛损伤[6]。SIBO与很多疾病密切相关,如非酒精性脂肪性肝病(non-alcoholic fatty liver disease, NAFLD)[7]、肠易激综合征[8]、深静脉血栓(deep vein thrombosis, DVT)[9-10]、糖尿病[11-12]、胃肠道肿瘤[13]、帕金森[14-15]、炎症性肠病[16]等。呼气试验有廉价、简便、非侵入性等优点,本试验采用此方法检测SIBO[17]。
目前,关于UC与SIBO的关系报道甚少。本文通过检测轻-中度UC患者的甲烷-氢气呼气试验,探讨UC患者与SIBO之间的关系。
1 资料与方法
1.1一般资料选取2016年6月至2017年12月海军总医院就诊,并同时完善甲烷-氢气呼气试验的轻-中度UC患者,共120例,男64例,女56例,男女比例1.14∶1,年龄(38.6±9.5)岁。对照组选取同期来院体检健康者60名,男31名,女29名,男女比例1.07∶1,年龄(39.0±9.0)岁。两组性别、年龄比较,差异均无统计学意义(P>0.05),具有可比性。
1.2排除标准(1)肝脏病变、急性感染、其他慢性炎性疾病及妊娠患者;(2)行结肠切除术的UC患者,因其可能会导致口盲传输时间(orocecal transit time,OCTT)(OCTT为小肠传递时间,主要反映小肠传输功能[18])延长,从而导致SIBO阳性;(3)在试验开始前1个月内使用抗生素和益生菌的患者;(4)糖尿病患者,因糖尿病扰乱了自主神经功能,可能导致胃肠功能紊乱、菌群失调等[19];(5)长期应用PPI、萎缩性胃炎患者,因其胃酸减少可能导致SIBO。研究[20-21]认为,PPI和胃大部切除术等可能引起胃酸分泌减少的情况会引起SIBO;(6)肥胖患者。
1.3甲烷-氢气呼气试验受检者口服底物前需漱口,而后向采气袋内吹入气体,之后30 min服用乳果糖10 ml,自此每隔30 min重复上述步骤采气,直至收集8个采气袋。最后由甲烷-氢气呼出气体分析仪 (BreathTracker)(美国Quintron公司)检测呼出气体。
注意事项:空腹8 h以上接受检查,整个过程禁食,可饮水;晨起后禁止吸烟;检测过程中不做剧烈运动。
SIBO的诊断标准(口服乳果糖120 min内存在以下任意一种情况即可):
(1)氢气浓度>基础值20 ppm;
(2)甲烷浓度升高>基础值12 ppm;
(3)甲烷和氢气浓度之和升高>基础值15 ppm;
(4)整个检查过程中出现双峰曲线。
1.4治疗及分组采用随机数字法,对UC患者中存在SIBO的,分成A、B两组,A组给予美沙拉嗪(0.5 g,上海爱的发制药有限公司)治疗(1 g,4次/d,6周);B组给予美沙拉嗪(1 g,4次/d,6周)和利福昔明(0.2 g,ALFA WASSERMANN制药公司)(0.2 g,4次/d,14 d)治疗,再比较两组的临床疗效、ESR和CRP。两组均进行健康的饮食、生活教育。
1.5临床疗效临床疗效评价参照既往文献共识[22-23]标准。总有效率=完全缓解+显效+有效(见表1)。

表1 临床疗效评价标准Tab 1 Clinical efficacy evaluation standard
注:相应诊断符合①+②或③,即可诊断。
1.6ESR、CRP检测分别于治疗前、后采集患者清晨空腹静脉血,检测ESR、CRP。

2 结果
2.1试验组、对照组SIBO阳性率结果比较试验组120例患者中,SIBO(+)53例,阳性率44.2%;对照组60名健康体检者,SIBO(+)13名,阳性率21.7%。试验组SIBO阳性率明显高于对照组,差异有统计学意义(χ2=8.720,P<0.001)。
2.2A、B组临床疗效比较利福昔明根除SIBO后可提高美沙拉嗪对UC的临床疗效。A组的总有效率是80.77%,B组是92.59%,B组的疗效明显优于A组(P<0.05,见表2)。
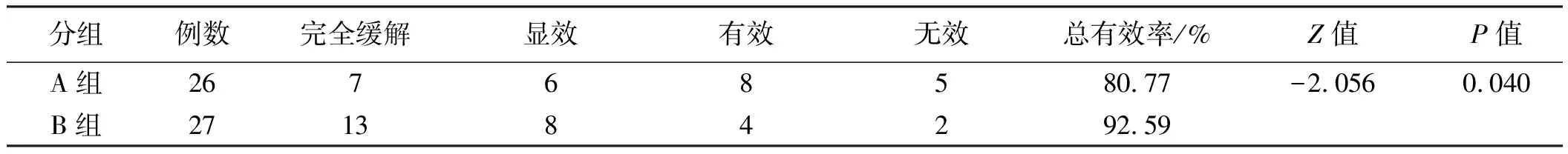
表2 A、B组间疗效比较Tab 2 Comparison of efficacy between group A and group B
2.3ESR、CRP比较利福昔明根除SIBO后,ESR、CRP较根除治疗前明显降低,治疗后B组ESR、CRP明显低于A组(P<0.01,见表3),提示根除SIBO有助于UC病情缓解。

表3 各组治疗前后ESR、CRP变化Tab 3 Changes of ESR, CRP before and after treatment in each group
3 讨论
3.1UC对SIBO的影响UC一般局限于结肠,偶尔延伸到回肠末端。但通过试验,我们发现,UC患者的SIBO阳性率高于健康人群。国外也有研究[24]发现,UC患者及动物模型存在小肠功能异常,可以表现为肠液减少,D-木糖、氨基酸和脂肪的吸收减少等方面。可能的机制有:(1)营养吸收不良:使用灌注研究发现,UC患者的肠液、电解质的吸收显著减少。GUSTAFSSON等[25]发现,即使是在缓解期,UC患者和正常人的肠道分泌能力也不同,即近端结肠黏膜对cAMP依赖的分泌更敏感,对Ca2+依赖的分泌不敏感。(2)通透性的变化:BÜNING等[26]发现,遗传因素导致UC患者的肠道通透性增加,也证实了UC患者即使是在缓解期,小肠通透性依然是增加的。(3)动力紊乱:RANA等[27]认为,UC患者还原性谷胱甘肽、IL-6、IL-8、TNF-α、IL-10失衡,脂质过氧化等导致肠道蠕动能力改变,进而增加UC患者的SIBO发生率。ROLAND等[28]通过对37例或同时进行乳果糖氢呼气试验(lactulose breath testing,LBT)和无线动力胶囊(wireless motility capsule, WMC, 又叫SmartPill)(一种全胃肠动力检测系统,可检测压力、pH和温度[29]) 证明了口盲传输时间的延长容易导致SIBO。另在UC患者中,结肠环肌中IL-1β增加,并可能通过过氧化氢的生成导致UC患者结肠运动功能障碍[30]。以上改变可能由于细胞因子和肠神经系统的改变而引起。
3.2SIBO对UC的影响肠道菌群的改变目前被认为是UC发生的重要机制之一[31]。肠道正常菌群(500~1 000种,总细胞数为1014)有很多功能:抑制病原菌生长;加强上皮屏障作用;通过Toll样受体通路,调节炎症反应[32]。临床研究[33]表明,UC患者中厚壁菌门和拟杆菌减少,变形菌和放线菌增加。孙勇等[34]通过对比缓解期与活动期UC患者的肠黏膜病理与肠道菌群,证明了菌群失调与肠道病理损伤有密切关系。UYGUN等[35]通过对30例UC患者进行粪菌移植,发现30%患者无效,70%患者出现临床症状减轻(其中另有总体30%的患者达到临床和内镜下缓解)。多种益生菌被发现可以通过阻断致病菌的有害作用维持肠道稳态,增加上皮屏障完整性,促进固有免疫,平衡炎性因子等多种机制维持UC的缓解,防止复发[36]。UC患者的菌群改变也许如被破坏的原始森林,很难完全恢复。
3.3利福昔明治疗对UC的影响文献[37]报道,利福昔明可以帮助UC患者达到临床缓解。本试验中部分UC患者在应用利福昔明后临床症状也有明显缓解。具体机制可能包括以下几点:(1)利福昔明的直接杀菌活性。利福昔明为利福霉素衍生物,抗菌谱包括大部分革兰氏阳性菌和革兰氏阴性菌[38]。而且其不改变肠道菌群的构成,还会增加部分益生菌数量[39];(2)减少细菌黏附和内化[40];(3)激活孕烷受体X[41]。在动物模型的炎症性肠病,利福昔明产生治疗效果通过激活孕烷X受体,从而减少NF-κB水平;(4)抑制细菌移位[42]。需要指出的是,利福昔明对SIBO的清除率可达70%[43-44]。B组根除SIBO后,理论上仍有约30%阳性患者,由于时间限制,本试验未进一步研究。考虑到B组可能仍有30%SIBO阳性患者,所有患者根除SIBO后,B组的症状、炎性因子可能会有进一步的改善。
综上,本研究发现,UC患者的SIBO阳性率明显高于健康人,利福昔明根除SIBO后,部分UC患者症状、炎性指标明显缓解。阐释了SIBO在UC中的作用,并提出了利福昔明的治疗方案。
[1] TRONCONE E, MONTELEONE G. The safety of non-biological treatments in ulcerative colitis [J]. Expert Opin Drug Saf, 2017, 16(7): 779-789. DOI: 10.1080/14740338.2017.1340936.
[2] FEUERSTEIN J D, CHEIFETZ A S. Ulcerative colitis: epidemiology, diagnosis, and management [J]. Mayo Clin Proc, 2014, 89(11):1553-1563. DOI: 10.1016/j.mayocp.2014.07.002.
[4] NG S C, SHI H Y, HAMIDI N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies [J]. Lancet, 2018, 390(10114): 2769-2778. DOI: 10.1016/S0140-6736(17)32448-0.
[5] NG S C, BERNSTEIN C N, VATN M H, et al. Geographical variability and environmental risk factors in inflammatory bowel disease [J]. Gut, 2013, 62(4): 630-649. DOI: 10.1136/gutjnl-2012-303661.
[6] ROLAND B C, LEE D, MILLER L S, et al. Obesity increases the risk of small intestinal bacterial overgrowth (SIBO) [J]. Neurogastroenterol Motil, 2018, 30(3). DOI: 10.1111/nmo.13199.
[7] BELEI O, OLARIU L, DOBRESCU A, et al. The relationship between non-alcoholic fatty liver disease and small intestinal bacterial overgrowth among overweight and obese children and adolescents [J]. J Pediatr Endocrinol Metab, 2017, 30(11): 1161-1168. DOI: 10.1515/jpem-2017-0252.
[8] GHOSHAL U C, SHUKLA R, GHOSHAL U. Small intestinal bacterial overgrowth and irritable bowel syndrome: a bridge between functional organic dichotomy [J]. Gut Liver, 2017, 11(2): 196-208. DOI: 10.5009/gnl16126.
[9] FUJIWARA Y, WATANABE T, MURAKI M, et al. Association between chronic use of proton pump inhibitors and small- intestinal bacterial overgrowth assessed using lactulose hydrogen breath tests [J]. Hepatogastroenterology, 2015, 62(138): 268-272.
[10] FIALHO A, FIALHO A, SCHENONE A, et al. Association between small intestinal bacterial overgrowth and deep vein thrombosis [J]. Gastroenterol Rep (Oxf), 2016, 4(4): 299-303. DOI: 10.1093/gastro/gow004.
[11] BULANDA M, GOSIEWSKI T, BRZYCHCZY-WLOCH M. Small intestinal bacterial overgrowth in adult patients with type 1 diabetes [J]. Pol Arch Med Wewn, 2016, 126(9): 623-624. DOI: 10.20452/pamw.3574.
[12] RANA S V, MALIK A, BHADADA S K, et al. Malabsorption, orocecal transit time and small intestinal bacterial overgrowth in type 2 diabetic patients: a connection [J]. Indian J Clin Biochem, 2017, 32(1): 84-89. DOI: 10.1007/s12291-016-0569-6.
[13] LIANG S, XU L, ZHANG D, et al. Effect of probiotics on small intestinal bacterial overgrowth in patients with gastric and colorectal cancer [J]. Turk J Gastroenterol, 2016, 27(3): 227-232. DOI: 10.5152/tjg.2016.15375.
[14] FASANO A, BOVE F, GABRIELLI M, et al. Liquid melevodopa versus standard levodopa in patients with Parkinson disease and small intestinal bacterial overgrowth [J]. Clin Neuropharmacol, 2014, 37(4): 91-95. DOI: 10.1097/WNF.0000000000000034.
[15] HOUSER M C, TANSEY M G. The gut-brain axis: is intestinal inflammation a silent driver of Parkinson’s disease pathogenesis? [J]. NPJ Parkinsons Dis, 2017, 3: 3. DOI: 10.1038/s41531-016-0002-0.
[16] RANA S V, SHARMA S, MALIK A, et al. Small intestinal bacterial overgrowth and orocecal transit time in patients of inflammatory bowel disease [J]. Dig Dis Sci, 2013, 58(9): 2594-2598. DOI: 10.1007/s10620-013-2694-x.
[17] GRACE E, SHAW C, WHELAN K, et al. Review article: small intestinal bacterial overgrowth--prevalence, clinical features, current and developing diagnostic tests, and treatment [J]. Aliment Pharmacol Ther, 2013, 38(7): 674-688. DOI: 10.1111/apt.12456.
[18] 付遥垚, 刘诗. 两种亚型FD患者的口盲传递时间[J]. 世界华人消化杂志, 2014, 22(4): 583-587.
FU Y Y, LIU S. Assessment of orocecal transit time by breath hydrogen test in two subtypes of functional dyspepsia [J]. World Chinese Journal of Digestology, 2014, 22(4): 583-587.
[19] ZHAO M, LIAO D, ZHAO J. Diabetes-induced mechanophysiological changes in the small intestine and colon [J]. World J Diabetes, 2017, 8(6): 249-269. DOI: 10.4239/wjd.v8.i6.249.
[20] FUJIMORI S. What are the effects of proton pump inhibitors on the small intestine? [J]. World J Gastroenterol, 2015, 21(22): 6817-6819. DOI: 10.3748/wjg.v21.i22.6817.
[21] 王洪艳, 孙士东, 毕英杰, 等. 长期使用质子泵抑制剂与小肠细菌过度生长的关系研究[J]. 胃肠病学和肝病学杂志, 2016, 25(11): 1302-1304. DOI: 10.3969/j.issn.1006-5709.2016.11.025.
WANG H Y, SUN S D, BI Y J, et al. Relationship between the long-term use of PPIs and the small intestinal bacterial overgrowth [J]. Chin J Gastroenterol Hepatol, 2016, 25(11): 1302-1304. DOI: 10.3969/j.issn.1006-5709.2016.11.025.
[22] 梁洁, 周林, 沙素梅, 等. 炎症性肠病诊断与治疗的共识意见(2012年·广州)溃疡性结肠炎诊断部分解读[J]. 胃肠病学, 2012, 17(12): 712-720. DOI: 10.3969/j.issn.1008-7125.2012.12.003.
LIANG J, ZHOU L, SHA S M, et al. Interpretation of the consensus on diagnosis and management of inflammatory bowel disease (Guangzhou, 2012) from the perspective of diagnosis of ulcerative colitis [J]. Chin J Gastroenterol, 2012, 17(12): 712-720. DOI: 10.3969/j.issn.1008-7125.2012.12.003.
[23] 中国中西医结合学会消化系统疾病专业委员会. 溃疡性结肠炎中西医结合诊疗指南(草案) [J]. 中国中西医结合消化杂志, 2011, 19(1): 61-65.
[24] MOURAD F H, BARADA K A, SAADE N E. Impairment of small intestinal function in ulcerative colitis: role of enteric innervation [J]. J Crohns Colitis, 2017, 11(3): 369-377. DOI: 10.1093/ecco-jcc/jjw162.
[25] GUSTAFSSON J K, HANSSON G C, SJOVALL H. Ulcerative colitis patients in remission have an altered secretory capacity in the proximal colon despite macroscopically normal mucosa [J]. Neurogastroenterol Motil, 2012, 24(8): e381-e391. DOI: 10.1111/j.1365-2982.2012.01958.x.
[26] BÜNING C, GEISSLER N, PRAGER M, et al. Increased small intestinal permeability in ulcerative colitis: rather genetic than environmental and a risk factor for extensive disease? [J]. Inflamm Bowel Dis, 2012, 18(10): 1932-1939. DOI: 10.1002/ibd.22909.
[27] RANA S V, SHARMA S, KAUR J, et al. Relationship of cytokines, oxidative stress and GI motility with bacterial overgrowth in ulcerative colitis patients [J]. J Crohns Colitis, 2014, 8(8): 859-865. DOI: 10.1016/j.crohns.2014.01.007.
[28] ROLAND B C, CIARLEGLIO M M, CLARKE J O, et al. Small intestinal transit time is delayed in small intestinal bacterial overgrowth [J]. J Clin Gastroenterol, 2015, 49(7): 571-576. DOI: 10.1097/MCG.0000000000000257.
[29] 王艳芝, 彭丽华, 杨云生. 无线动力胶囊对全消化道功能参数的分析及其临床研究[J]. 中华消化杂志, 2014, 34(12): 870-872.
[30] VREES M D, PRICOLO V E, POTENTI F M, et al. Abnormal motility in patients with ulcerative colitis: the role of inflammatory cytokines [J]. Arch Surg, 2002, 137(4): 439-445, 445-446.
[31] SHEEHAN D, SHANAHAN F. The gut microbiota in inflammatory bowel disease [J]. Gastroenterol Clin North Am, 2017, 46(1): 143-154. DOI: 10.1016/j.gtc.2016.09.011.
[32] DUPONT A W, DUPONT H L. The intestinal microbiota and chronic disorders of the gut [J]. Nat Rev Gastroenterol Hepatol, 2011, 8(9): 523-531. DOI: 10.1038/nrgastro.2011.133.
[33] KUMP P K, GRÖCHENING H P, LACKNER S, et al. Alteration of intestinal dysbiosis by fecal microbiota transplantation does not induce remission in patients with chronic active ulcerative colitis [J]. Inflamm Bowel Dis, 2013, 19(10): 2155-2165. DOI: 10.1097/MIB.0b013e31829ea325.
[34] 孙勇, 丁彦青. 溃疡性结肠炎患者肠道菌群与病理变化关系的探讨[J]. 现代消化及介入诊疗, 2009, 13(1): 26-28. DOI: 10.3969/j.issn.1672-2159.2009.01.008.
SUN Y, DING Y Q. Changes of intestinal flora and pathology in ulcerative colitis [J]. Modern Digestion &Intervention, 2009, 13(1): 26-28. DOI: 10.3969/j.issn.1672-2159.2009.01.008.
[35] UYGUN A, OZTURK K, DEMIRCI H, et al. Fecal microbiota transplantation is a rescue treatment modality for refractory ulcerative colitis [J]. Medicine (Baltimore), 2017, 96(16): e6479. DOI: 10.1097/MD.0000000000006479.
[36] LIANG J, SHA S M, WU K C. Role of the intestinal microbiota and fecal transplantation in inflammatory bowel diseases [J]. J Dig Dis, 2014, 15(12): 641-646. DOI: 10.1111/1751-2980.12211.
[37] SHAYTO R H, ABOU M R, SHARARA A I. Use of rifaximin in gastrointestinal and liver diseases [J]. World J Gastroenterol, 2016, 22(29): 6638-6651. DOI: 10.3748/wjg.v22.i29.6638.
[38] SCRIBANO M L. Role of rifaximin in inflammatory bowel disease treatment [J]. Mini Rev Med Chem, 2015, 16(3): 225-229.
[39] SARTOR R B. Review article: the potential mechanisms of action of rifaximin in the management of inflammatory bowel diseases [J]. Aliment Pharmacol Ther, 2016, 43 Suppl 1: 27-36.
[40] BROWN E L, XUE Q, JIANG Z D, et al. Pretreatment of epithelial cells with rifaximin alters bacterial attachment and internalization profiles [J]. Antimicrob Agents Chemother, 2010, 54(1): 388-396.DOI: 10.1128/AAC.00691-09.
[41] DUPONT H L. Therapeutic effects and mechanisms of action of rifaximin in gastrointestinal diseases [J]. Mayo Clin Proc, 2015, 90(8): 1116-1124. DOI: 10.1016/j.mayocp.2015.04.016.
[42] KIMER N, PEDERSEN J S, TAVENIER J, et al. Rifaximin has minor effects on bacterial composition, inflammation and bacterial translocation in cirrhosis: a randomized trial [J]. J Gastroenterol Hepatol, 2018, 33(1): 307-314. DOI: 10.1111/jgh.13852.
[43] 崔立红, 王晓辉, 闫志辉, 等. 小肠细菌过度生长与肠易激综合征的关系[J]. 解放军医学院学报, 2015, 36(10): 979-982. DOI: 10.3969/j.issn.2095-5227.2015.10.005.
CUI L H, WANG X H, YAN Z H, et al. Relationship between irritable bowel syndrome and small intestinal bacterial overgrowth [J]. Acad J Chin PLA Med Sch, 2015, 36(10): 979-982. DOI: 10.3969/j.issn.2095-5227.2015.10.005.
[44] GATTA L, SCARPIGNATO C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth [J]. Aliment Pharmacol Ther, 2017, 45(5): 604-616. DOI: 10.1111/apt.13928.