Mitral Stenosis: A Review
By C. Richard Conti, MD, MACC
1Department of Medicine, University of Florida, Gainseville, FL, USA
Introduction
The purpose of this review is to report and outline the clinical features, diagnostic studies and therapy of mitral stenosis. What is contained in this document will be directed towards physicians who have not evaluated many patients with this problem. Classic mitral stenosis is usually of rheumatic origin, but not all patients with mitral stenosis have had acute rheumatic fever. For example, mitral annular calcification can also produce a diastolic gradient from the left atrium to the left ventricle. In the United States, the number of patients presenting with mitral stenosis, or other forms of rheumatic heart disease,has markedly diminished over the last 60 years but this is not the case in developing countries where there are numerous cases of acute rheumatic fever and mitral stenosis. The decrease in the number of cases of mitral stenosis is probably related to the decrease in the occurrence of beta Hemolytic streptococcus infection with the use of antibiotics e.g.penicillin, which in turn decreases the number of cases of acute rheumatic fever. In addition, the use of prophylactic penicillin in patients who had acute rheumatic fever who are constantly being exposed to B hemolytic Streptococcus infections e.g. school teachers of small children.
An anecdotal experience I had makes the point about repetitive exposure and the development of rheumatic heart disease. Many years ago, I visited with Professor John Barlow at Witswatersrand University in Johannesburg, South Africa. He invited me to accompany him to Baragwanath Hospital, which provided hospital support to the black township of Soweto. There, I saw many children with tight mitral stenosis and was told that this occurred because the children with acute rheumatic fever, who were given penicillin prophylaxis did not take the drug and continued to be repetitively exposed to B hemolytic infections.
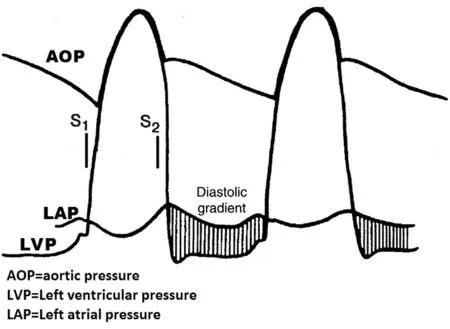
Figure 1 Physiopathology of Mitral Stenosis: Demonstrating the Diastolic Pressure Gradient between Left Atrium and Left Ventricle.
Anatomy and Physiopathology
At autopsy, the mitral valves exposed to repetitive in flammatory processes in the past, reveal signs of healing of the in flamed valves. This healing causes the valves to become thickened, and there is often fusion of the commissures. Because of ongoing stiffness of the non-calci fied mitral valve, the valve tends to “dome down” and snap open like a spinnaker in the wind of a sailboat during diastolic opening; thus, the term “opening snap” gets its origin. During diastole a pressure difference is apparent between the left atrium and the left ventricle (Figure 1). Later, during the life of the patient, calci fication may occur, particularly in men but also in women. Calci fic valves, generally, are not as mobile as non-calci fied valves and on auscultation, an opening snap may not be audible.
Symptoms
A common clinical presentation is a middle-aged female complaining of easy fatigability, dyspnea on exertion, or palpitations. In most, but not all instances, there is slow progression of symptoms,such as dyspnea, and fatigue; e.g. women often present in their late 30s or early 40s. Other less common presentations include hemoptysis, thromboembolic events and endocarditis. Hemoptysis can range from blood tinged sputum to massive hemoptysis.The development of rheumatic heart disease probably depends on repetitive exposure to B hemolytic streptococcus.
Critical mitral stenosis occurs when the mitral ori fice is less than 25% of its normal opening. As a result, most patients will experience dyspnea on exertion because of elevated left atrial and thus elevated pulmonary venous pressure.
Tachycardia of any etiology (including atrial fibrillation) can result in pulmonary congestion, as well. Atrial fibrillation is more common in the older patient with severe mitral stenosis.
Infective endocarditis, although not common,must be considered in any patient with mitral stenosis at risk for infection.
Thrombo-embolic complications do occur because of incomplete emptying and stasis of blood in the left atrium in patients with mitral stenosis.Left atrial thrombi may develop particularly in patients in atrial fibrillation.
Transesophageal cardiac ultrasound has identified a major source of stasis in the left atrium, i.e.the left atrial appendage (Figure 2). This source of thrombosis can result in embolization of thrombi to the brain and peripheral arteries as well as the coronary arteries. As a result of the emboli from the left atrium, cerebral infarction, cardiac infarction, splenic infarction, kidney infarction and saddle embolus at the aortic bifurcation can occur.Thromboembolic events are most obvious in the cerebral circulation since it does not take much of a thrombus to produce symptoms, whereas an embolus of similar size to the lung or peripheral arteries other than cerebral may go unnoticed.
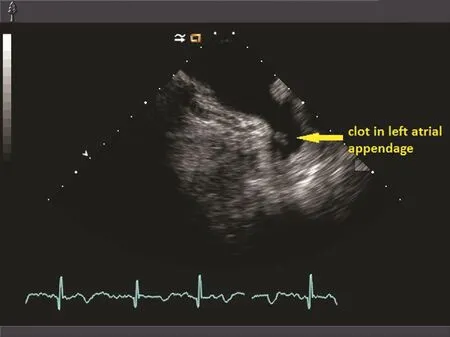
Figure 2 Left Atrial Appendage Clot as Seen on Transesophageal Echo.
Coronary embolus, in my experience, is not very common but it can happen and result in an acute myocardial infarction.
Physical Examination
As in other valvular heart disease, physiologic events account for the physical findings. Physiologic events that account for the abnormalities in patients with pure mitral stenosis include:
1. Pulse:an irregular pulse secondary to atrial fi-brillation may be present. The atrial fibrillation patient may have a fast heart rate. During tachycardia, diastole is shortened and left atrial emptying is diminished,
2. Pregnant patientsnormally have increased cardiac output and sometimes, tachycardia which can exacerbate symptoms if mitral stenosis is present.
3. Blood pressureis generally normal unless the patient has known hypertension.
4. Jugular venous pulse:jugular venous pulsations are not well seen if the right atrial pressure is normal, but right atrial pressure may be elevated if right ventricular diastolic pressure(RVEDP) is elevated. RVEDP may be elevated if pulmonary hypertension is present. Pulmonary hypertension can be associated with mitral stenosis secondary to elevated left atrial pressure.
5. Left parasternal liftmay be present if pulmonary hypertension and elevation of the right ventricular pressure is present.
6. Apex impulseis usually within the normal range, since there is no increase in size of the left ventricle in patients with isolated mitral stenosis.
7. Auscultatory findingsof classic pure mitral stenosis, (especially when auscultation is done with the patient in the left lateral decubitus position)include; a loud first heart sound, clear systole, a normal pulmonary second sound (if pulmonary artery pressure is normal) or an accentuated pulmonary second sound (if pulmonary hypertension is present,) and an opening snap (OS). The OS occurs about 80–90 ms after the second sound if the mitral lea flets are mobile. A diastolic rumble follows the opening snap and morphs into an accentuated presystolic murmur followed by a loud first heart sound (Figure 3). If calci fication of the lea flets occurs, the opening snap may not be heard. When it is audible the OS is followed by a mid-diastolic rumble due to low frequency passive blood flow from the left atrium to the left ventricle across an obstructing mitral valve and presystolic accentuation of the diastolic murmur due to atrial contraction in which high frequency flow across an obstructing mitral valve occurs from left atrium to left ventricle just before the loud first heart sound.
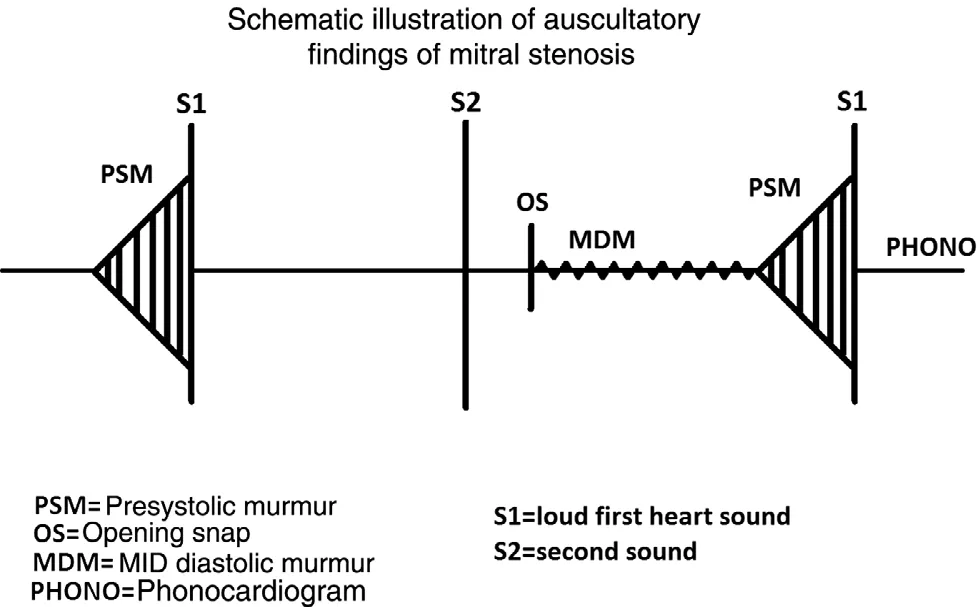
Figure 3 Schematic Illustration of Auscultatory Findings in Pure Mitral Stenosis.
8. Second sound, opening snap interval (S2-OS):in mild mitral stenosis the interval is wide and as the stenosis increases in severity, the interval narrows. This is a reasonably good sign of the severity of the mitral stenosis.
Differential Diagnosis
Some conditions can mimic the symptoms and physical signs of mitral stenosis. These include:
Left atrial myxoma;when a myxoma occurs in the left atrium, it usually attaches to the atrial septum and can extend into the mitral valve during diastole,causing a decrease in flow from the left atrium to the left ventricle. If this occurs, a “tumor plop” can be auscultated which simulates the opening snap of mitral stenosis and a diastolic rumble can also be heard. This condition is easily diagnosed by cardiac ultrasound or by cardiac magnetic resonance(Figure 4).
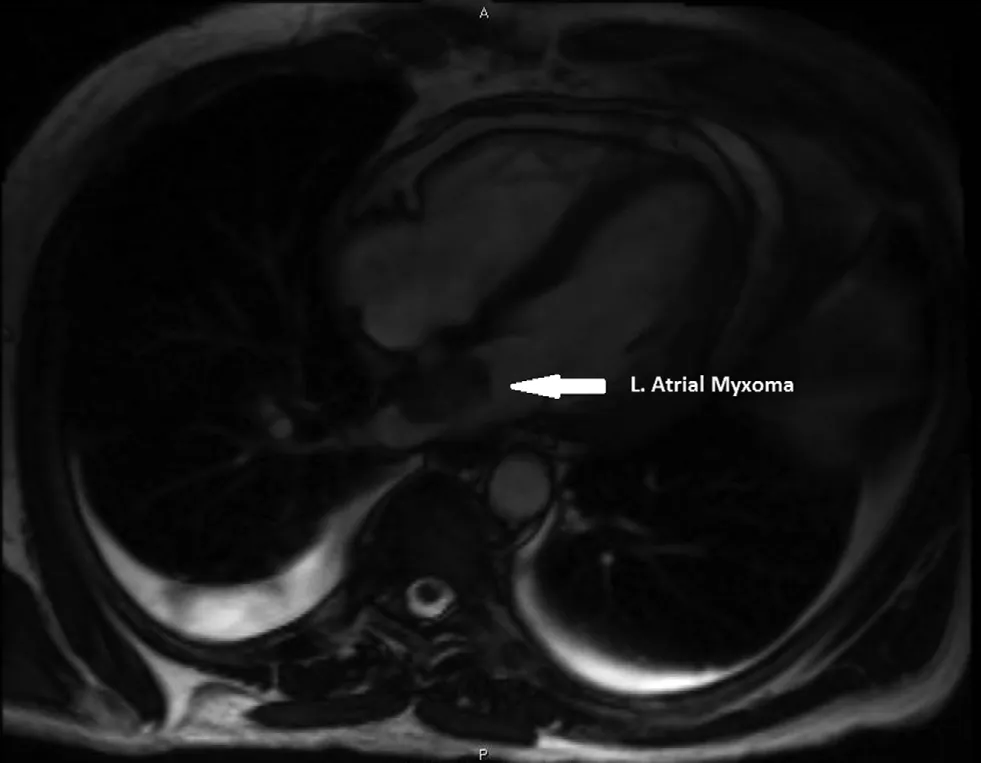
Figure 4 Cardiac Magnetic Resonance of Left Atrial Myxoma Attached to the Atria Septum.
Mitral Prosthetic valvesnormally have a small gradient across the valve and on occasion will thrombose, especially if the patient is not anticoagulated. This will result in more obstruction to flow across the valve and increase atrial pressure.Usually when a mechanical prosthetic valve clots,the closure sounds are muted. But remember, bilea flet mechanical prosthetic valves may still make a closure sound, when one lea flet of the valve is working normally. The best way to evaluate lea flet motion is cine- fluoroscopy.
–Clot that Obstructs Flow from the Pulmonary Veins to the Left Atrium
–Pulmonary Vein Occlusion e.g. Secondary to RF Ablation for Atrial Fibrillation
Occluded prosthetic mitral valves, clot obstructing the pulmonary veins and pulmonary vein occlusion can produce symptoms similar to those of mitral stenosis e.g. pulmonary congestion but not physical signs of mitral stenosis, since the mitral valve is not effected.
Electrocardiography
The ECG may be normal or the patient may be in atrial fibrillation. If the patient is in sinus rhythm there may be a classic broad M-shaped con figuration of the P-wave in lead II called P-mitrale (Figure 5).The P wave may be >120 ms. in duration. There also may be a biphasic P-wave in lead V1, (P negative V1) suggesting increased left atrial pressure.Other ECG abnormalities are non-speci fic and may be due to other conditions such as ischemic heart disease, conduction abnormalities, hypertension etc. Right ventricular hypertrophy is sometimes seen in patients with pulmonary hypertension.
Chest X-Ray
Chest X-Ray can be normal in mild mitral stenosis but it can also show a double density in the posterior-anterior view which suggests a large left atrium in severe mitral stenosis. A large left atrium also can result in elevation of the left main stem bronchus (Figure 6). The left ventricle is not enlarged and the pulmonary artery can be prominent. Calcium is sometimes seen in the area of the mitral valve, particularly in the lateral view.In very severe cases “Kerley” B lines are present and there may be obvious evidence for pulmonary congestion particularly in the upper lobes of the lung.
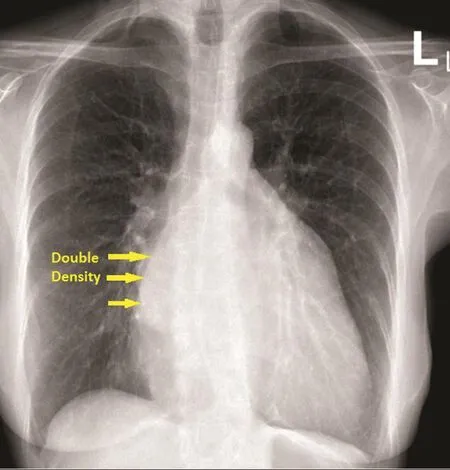
Figure 6 Chest X-Ray of Mitral Stenosis Illustrating Double Density at Right Heart Border Suggesting Enlarged Left Atrium.
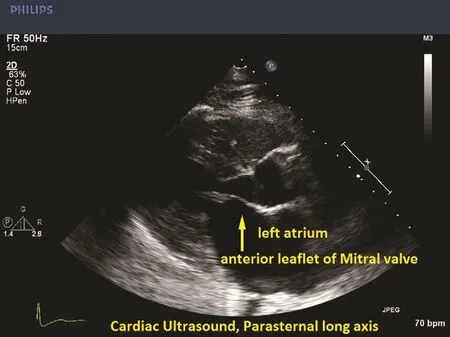
Figure 7 Cardiac Ultrasound; Parasternal Long Axis View,Demonstrating Abnormal Anterior Mitral Valve Lea flet in Early Diastole-Not Quite a “Hockey Stick” Deformity but Close.
The findings on Chest X-Ray and ECG, just described are suggestive of mitral stenosis but not diagnostic.
Cardiac Ultrasound
Mitral stenosis is easily diagnosed with both M mode and 2D echocardiography. Using 2D cardiac ultrasound the anterior lea flet of the mitral valve, in the para sternal long axis view, often resembles a“hockey stick” during diastole (Figure 7).
The following Cardiac ultrasound features are evaluated when mitral stenosis is clinically suspected and include evaluation of mitral valve motion, left ventricular function, left atrial size,and it may be especially useful to detect the presence or absence of left atrial clots in patients with mitral stenosis. Using the technique of Doppler ultrasound, one can derive the transvalvular gradient across the mitral valve (Figure 8). In my opinion, cardiac ultrasound should not be used prior to history, physical exam, ECG and chest X-Ray, but rather should be use to con firm or refute the clinical diagnosis of mitral stenosis.
Cardiac Catheterization
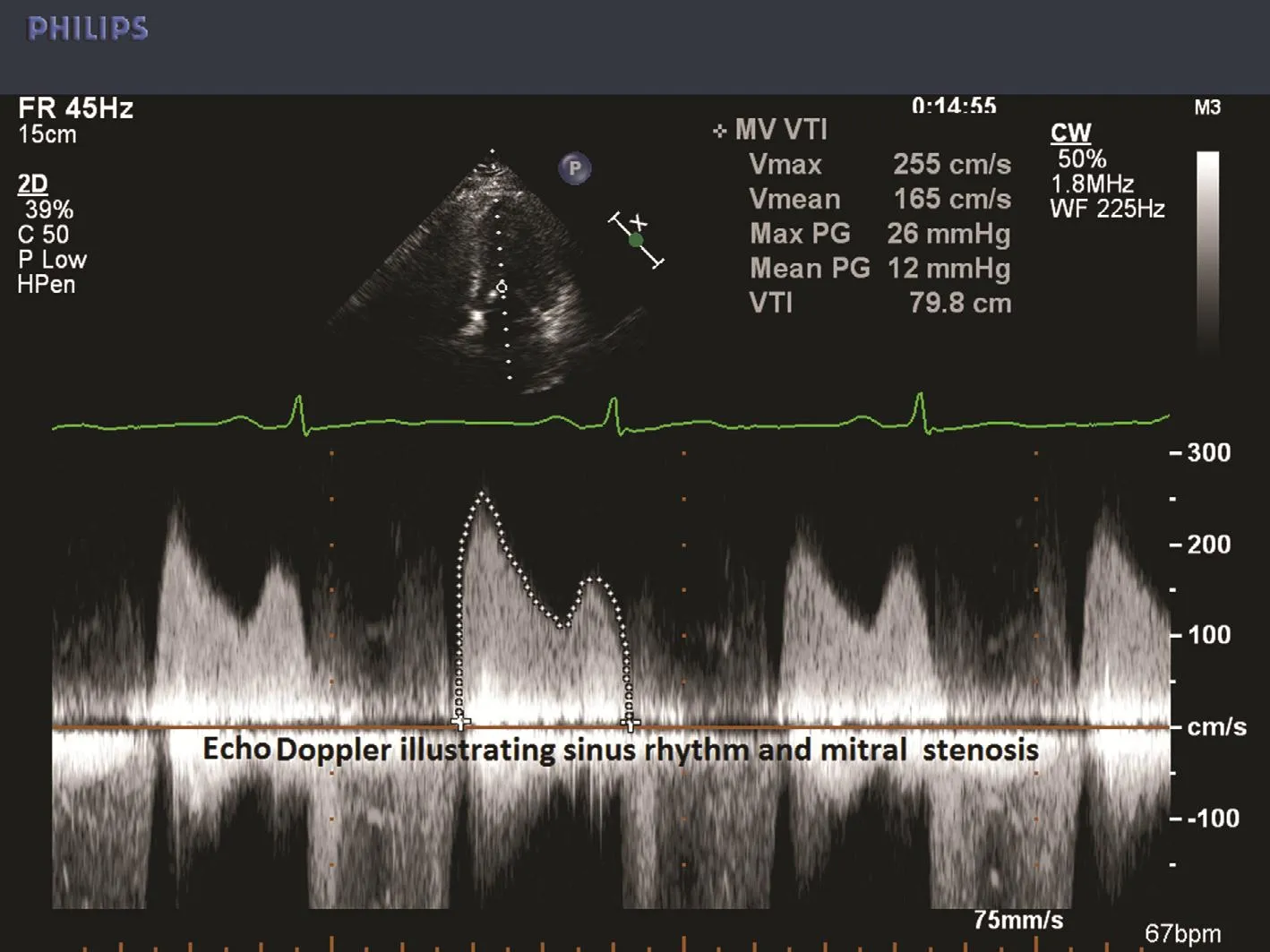
Figure 8 Cardiac Ultrasound Doppler Evaluation of Mitral Valve Gradient.
If surgery or mitral balloon valvuloplasty using non-surgical techniques e.g. Inoue Balloon, is contemplated, cardiac catheterization usually is performed to assess and con firm the degree of stenosis. In the case of balloon valvuloplasty, a transseptal left heart catheterization must be performed.A resting pressure gradient across the mitral valve greater than 10 mmHg is consistent with moderately severe mitral stenosis. Angiography of the left ventricle or left atrium reveals a “doming down” of the mitral valve during diastole if the valve is pliable and not heavily calci fied. In some catheterization laboratories, exercise is performed during cardiac catheterization to evaluate the effect of increased stress on myocardial blood flow. When this is done, there may be a marked increase in the left atrial and pulmonary venous pressure which may result in symptoms. e.g. dyspnea due to pulmonary congestion.
In the older patient where there may be some concern for the presence of coronary artery disease,coronary angiography may be performed.
Non-Surgical Therapy
Drug therapy is effective in controlling symptoms in many instances. The mainstay of therapy is slowing the heart to increase diastolic filling time and decreasing vascular volume. B blockers are probably the best drug to do this in combination with diuretics. If the patient presents with new onset of symptomatic atrial fibrillation, DC cardioversion(often with TEE ultrasound to search for clots in the left atrial appendage) is effective therapy.
Mitral Commisurotomy
As with most stenotic valve disease, surgical treatment has been the reference standard for many years, particularly in patients who have been treated medically and have persistent symptoms. In my opinion, both surgical therapy or balloon valvuloplasty (Figure 9) of the mitral valve generally relieves symptoms, and may possibly prolong life by reducing the prevalence or incidence of pulmonary edema and arrhythmias in these patients. There are many criteria for surgical commisurotomy and balloon mitral valvuloplasty, which will not be detailed here. However, if the valve is severely calci fied, and there is a signi ficant amount of mitral regurgitation, and sub-valvular thickening of the chordae tendiniae, the valve may need to be replaced or reconstructed using surgical techniques. The goal of therapy in 2016 is to reconstruct the mitral valve,if at all possible. This seems to be taking place frequently in 2016.
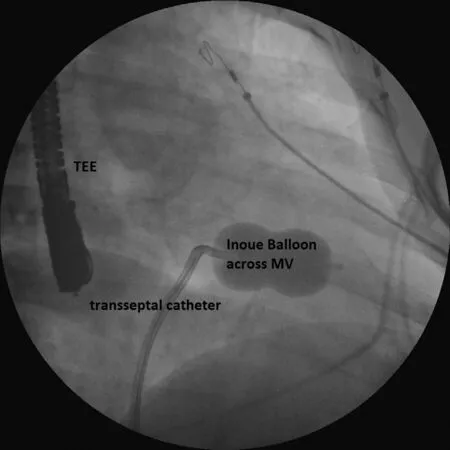
Figure 9 RAO Fluoroscopic Picture of Transseptal Technique to Perform Mitral Commisurotomy Using the Inoue Balloon (not Fully Expanded).
Take Home Messages
1. Not all patients with mitral stenosis give a history of acute rheumatic fever.
2. Mitral stenosis (MS) patients most commonly present with exertional dyspnea and/or easy fatigue. Less common clinical presentations include hemoptysis, stroke or other thromboembolic events.
3. Increasing cardiac output or heart rate can precipitate symptoms in patients with any risk of rheumatic heart disease and signs or symptoms suggestive of MS.
4. Cardiac ultrasound con firms the diagnosis of mitral stenosis.
5. Cardiac catheterization is not generally required for diagnosis of MS but is indicated when the diagnosis is not certain or coronary angiography is warranted.
6. The differential diagnosis of MS includes left atrial myxoma, prosthetic valve obstruction,Clot in the left atrium and pulmonary vein stenosis secondary to radio frequency ablation of atrial fibrillation.
7. Non-surgical therapy of mitral stenosis consists of B blockers to slow the heart and diuretics to decrease vascular volume. DC cardioversion is indicated in symptomatic patients with new onset of atrial fibrillation (preferrably done with TEE guidance).
8. Mitral commisurotomy with surgery or balloon valvuloplasty is indicated for patients refractory to medical therapy, if the valve is pliable and not heavily calci fied. If heavy calci fication is present, Mitral valve replacement is indicated.
FURTHER READING
1. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd,Guyton RA, O’Gara PT, Ruiz CE,Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63(22):e57.
2. Selzer A, Cohn KE. Natural history of mitral stenosis: a review.Circulation 1972;45(4):878–90.
3. Chandrashekhar Y, Westaby S,Narula J. Mitral stenosis. Lancet 2009;374(9697):1271–83.
4. Rowe JC, Bland EF, Sprague HB,White PD. The course of mitral stenosis without surgery: ten- and twenty-year perspectives. Ann Intern Med 1960;52:741.
 Cardiovascular Innovations and Applications2018年1期
Cardiovascular Innovations and Applications2018年1期
- Cardiovascular Innovations and Applications的其它文章
- Functional Tricuspid Regurgitation and Ring Annuloplasty Repair
- Misdiagnosed Aortic Intramural Hematoma and the Role of Intravascular Ultrasound Imaging in Detection of Acute Aortic Syndrome: A Case Report
- Management of Mitral Regurgitation in a Patient Contemplating Pregnancy
- An Asymptomatic Patient with Severe Mitral Regurgitation
- Clinical Evaluation of a Patient with Asymptomatic Severe Aortic Stenosis
- Low-Gradient, Low Ejection Fraction SevereAortic Stenosis: Still a Management Conundrum
