An Asymptomatic Patient with Severe Mitral Regurgitation
Blase A. Carabello, MD
1 East Carolina University, Greenville, NC, USA
Introduction
Case Description
A 52-year-old woman is referred for evaluation of a heart murmur. She is physically active, participating in spinning classes 4 days per week. She reports not having any symptoms, and takes no medications.
– Physical examination: pulse rate 64; blood pressure 110/70 mmHg.
– Neck: estimated central venous pressure 5 cm H2O.
– Heart: apical beat sixth interspace 1 cm left of the midclavicular line; grade 3/6 holosystolic apical murmur. S3.
– Extremities: no edema.
– Echocardiogram: P2 and A2 prolapse; large central regurgitant mitral jet. Regurgitant fraction 52%; effective regurgitant ori fice area 0.42 cm2;reversal of pulmonary vein flow.
Ejection fraction (EF) 65%; end-systolic left ventricular (LV) dimension 38 mm. No tricuspid regurgitation; brain natriuretic peptide concentration 47 pg/mL.
Classi fication
The mitral valve is a complex structure composed of its lea flets, the chordae tendineae, the papillary muscles, and the mitral annulus. Abnormalities in any of these structures can cause mitral regurgitation (MR) that is classi fied as primary because it is a defect in the valve itself that has caused it to leak. In secondary MR the valve is usually normal; it is disease of the left ventricle either from cardiomyopathy or from myocardial infarction that causes papillary muscle displacement tethering of the valve and annular dilatation that prevent coaptation of a normal valve. In primary MR the hemodynamic burden of volume overload from an incompetent valve eventually leads to ventricular damage, heart failure, and death. Restoration of valve competence cures the disease. In secondary MR, there is already severe LV dysfunction, and restoration of mitral competence does not completely restore LV function.
The patient described has every physical examination finding and every echocardiographic finding of severe primary MR. Physical examination finds an enlarged heart. There is a holosystolic apical murmur. The third heart sound is indicative of the large volume of blood stored in the left atrium during diastole. The echocardiogram shows anatomic evidence of bilea flet prolapse, a regurgitant fraction exceeding 50%, a large MR jet, an effective regurgitant ori fice area greater than 0.40 cm2, and pulmonary vein flow reversal during systole, con firming that the MR is severe. Her reported level of physical activity indicates that she is truly asymptomatic.This then raises the issue of the proper management of the patient with severe asymptomatic MR.
Assessment of MR Severity
Severe MR is that amount of regurgitation that causes enough hemodynamic burden to produce symptoms and LV dysfunction. Although the issue has never been studied prospectively, in an animal model and in clinical studies in which patients required surgery [1, 2], the regurgitant fraction (the percentage of blood going backward) was 50% or more. Thus a regurgitant fraction of 50% seems to be a reasonable de finition of severe MR. In a clinical study, a regurgitant ori fice area of 0.4 cm2or greater was associated with poor outcomes, and is also incorporated into the de finition of “ severe” MR[3], as are a regurgitant flow of more than 60 mL per beat, a vena contracta (the smallest jet diameter as it leaves the mitral valve) of 0.7 cm, ( Figure 1)systolic reversal of pulmonary vein flow, and a large color- flow left atrial jet. However, no single parameter should de fine “ severe” in isolation. All parameters should be integrated to form a severity judgment in concert with the physical examination findings and LV and left atrial size. The volumes of both chambers should be enlarged in chronic asymptomatic MR as enlargement of both chamber is required to maintain an adequate forward stroke volume at filling pressures low enough to prevent pulmonary congestion.
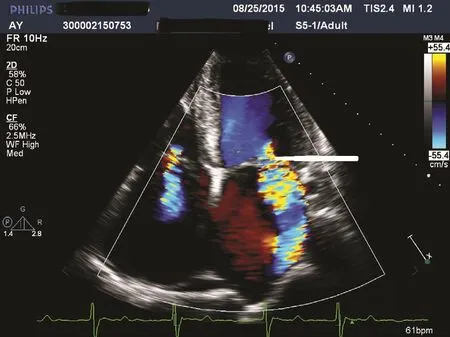
Figure 1 An Echocardiogram of a Patient with Severe Mitral Regurgitation.
Triggers for Intervention
Chronic MR may be tolerated for an uncertain period, but most patients reach the indication for intervention within about 6 years of the onset of severe disease, as demonstrated in Figure 2 [3– 8].The triggers for intervention are either the onset of symptoms attributable to MR [9] or the onset of LV dysfunction even in the absence of symptoms because the advent of either worsens prognosis if they are left unattended. The most frequent symptoms of MR are a gradual decline in exercise tolerance and a gradual increase in dyspnea on exertion. However, in the case of acute MR as might occur in chordal rupture, there may be sudden dyspnea or even pulmonary edema. As MR progresses, orthopnea and peripheral edema may also ensue. Symptom onset may be difficult to discern because symptoms may be unrecognized or may be attributed to aging, or the patient may alter his/her lifestyle to avoid symptoms. Exercise testing may be very useful in eliciting symptoms, and assessment of brain natriuretic peptide concentration may also lend objectivity to cardiac stress [10,11]. Indicators that LV dysfunction is occurring include reduced EF and increased end-diastolic LV dimension. Increased preload in MR increases EF such that “ normal” EF in MR is about 70%.As EF declines toward 65– 60%, LV dysfunction is developing in many patients, potentially negatively affecting outcome [12]. Thus EF falling toward 60% is an indication for surgery. Likewise,as LV function is compromised, the left ventricle becomes progressively larger at the end of contraction. Thus an end-systolic dimension increasing toward 40 mm is an indication for intervention[13]. However, it is likely that LV dysfunction is already developing by the time these thresholds are reached [14, 15].

Figure 2 The Natural History of Mitral Regurgitation Summarized from the Publications Noted in References[3– 7], the First Authors of which are Noted Here.As can be seen, within about 6 years of detection of severe mitral regurgitation an adverse event will have occurred in about half the patients. Taken from Bonow [8].
Timing of Intervention
The timing of intervention is determined by the triggers noted earlier and also by the type of correction that will performed. Waiting for triggers under close scrutiny has been demonstrated to be safe effective management [4]. However, in most cases of nonrheumatic MR, the valve can be repaired instead of replaced, sparing patients the risks inherent to prosthetic heart valves. If imaging finds valve pathoanatomy is such that the likelihood of valve repair is 95% or greater (e.g., P2 prolapse), many would opt for surgery before reaching a trigger [14,15]. This philosophy spares the patient frequent visits for follow-up surveillance and also the risk that a trigger will be missed, leading to potentially irreversible LV dysfunction, while avoiding the risks of a prosthetic valve. Further, the operative mortality for repair is about half that of replacement, and long-term survival is increased [16]. If repair is less likely to be performed, the risk of a prosthesis must be weighed, and surgery, either repair or replacement, is performed when the patients develops even mild symptoms or LV dysfunction. In inoperable symptomatic patients, percutaneous mitral repair is becoming an important less invasive option [17].
Our Patient
Although the patient was asymptomatic and had preserved LV function, her age made it certain that intervention was eventually inevitable [8]. Her surgeon felt con fident that a durable repair could be effected, and she underwent uneventful mitral valve repair, with no recurrence of MR at the 5-year follow-up.
Conclusion
When symptoms or early LV dysfunction occur in patients with primary MR, mitral valve repair or replacement must be performed to avoid irreversible LV dysfunction, heart failure, and death. However,primary nonrheumatic MR is usually treated in experienced hands with mitral valve repair instead of replacement, avoiding the complications of prosthetic heart valves. When there is 95% con fidence that a durable repair can be effected, early surgery becomes an important option instead of waiting for symptoms or LV dysfunction to occur, sparing the patient from frequent follow-up examinations and/or the possibility that one of these triggers for surgery will be missed, subjecting the patient to a poor outcome.
Conflict of Interest
The author declares no Conflict of interest.
REFERENCES
1. Carabello BA, Nakano K, Corin W, Biederman R, Spann JF Jr. Left ventricular function in experimental volume overload hypertrophy.Am J Physiol Heart Circ Physiol 1989;256(25):H974– 81.
2. Carabello BA. The relationship of left ventricular geometry and hypertrophy to left ventricular function in valvular heart disease. J Heart Valve Dis 1995;4(Suppl II):S132– 9.
3. Enriquez-Sarano M, Avierinos JF,Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation.N Engl J Med 2005;352(9):875– 83.
4. Rosenhek R, Rader F, Klaar U,Gabriel H, Krejc M, Kalbeck D. Outcome of watchful waiting in asymptomatic severe mitral regurgitation. Circulation 2006;113(18):2238– 44.
5. Grigioni F, Tribouilloy C, Avierinos JF, Barbieri A, Ferlito M, Trojette F,et al. Outcomes in mitral regurgitation due to flail lea flets: a multicenter European study. JACC Cardiovasc Imaging 2008;1:133– 41.
6. Kang DH, Kim JH, Rim JH, Kim MJ, Yun SC, Song JM, et al.Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation.Circulation 2009;119:797– 804.
7. Rosen SE, Borer JS, Hochreiter C,Supino P, Roman MJ, Devereux RB,et al. Natural history of the asymptomatic/minimally symptomatic patient with severe mitral regurgitation secondary to mitral valve prolapse and normal right and left ventricular performance. Am J Cardiol 1994;74:374–380.
8. Bonow RO. Chronic mitral regurgitation and aortic regurgitation: have indications for surgery changed? J Am Coll Cardiol 2013;61(7):693– 701.
9. Gillinov AM, Mihaljevic T,Blackstone EH, George K, Svensson LG, Nowicki ER, et al. Should patients with severe degenerative mitral regurgitation delay surgery until symptoms develop? Ann Thorac Surg 2010;90(2):481– 8.
10. Messika-Zeitoun D, Johnson BD,Nkomo V, Avierinos JF, Allison TG,Scott C, et al. Cardiopulmonary exercise testing determination of functional capacity in mitral regurgitation: physiologic and outcome implications. J Am Coll Cardiol 2006;20;47(12):2521– 7.
11. Mentias A, Patel K, Patel H, Gillinov AM, Rodriguez LL, Svensson LG,et al. Prognostic utility of brain natriuretic peptide in asymptomatic patients with signi ficant mitral regurgitation and preserved left ventricular ejection fraction. Am J Cardiol 2016;117(2):258– 63.
12. Enriquez-Sarano M, Tajik AJ,Schaff HV, Orszulak TA, Bailey KR,Frye RL. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation.Circulation 1994;90(2):830– 7.
13. Tribouilloy C, Grigioni F, Avierinos JF, Barbieri A, Rusinaru D,Szymanski C, et al. Survival implication of left ventricular end-systolic diameter in mitral regurgitation due to flail lea flets a long-term followup multicenter study. J Am Coll Cardiol 2009;54(21):1961– 8.
14. Tribouilloy C, Rusinaru D,Szymanski C, Mezghani S, Fournier A, L é vy F. Predicting left ventricular dysfunction after valve repair for mitral regurgitation due to lea flet prolapse: additive value of left ventricular end-systolic dimension to ejection fraction. Eur J Echocardiogr 2011;12(9):702– 10.
15. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd,Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.J Am Coll Cardiol 2017;70(2):252– 89.
16. Lazam S, Vanoverschelde JL,Tribouilloy C, Grigioni F, Suri RM,Avierinos JF, et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation: analysis of a large, prospective, multicenter,international registry. Circulation 2017;135(5):410– 22.
17. Feldman T, Kar S, Elmariah S,Smart SC, Trento A, Siegel RJ,et al. Randomized comparison of percutaneous repair and surgery for mitral regurgitation: 5-year results of EVEREST II. J Am Coll Cardiol 2015;66(25):2844– 54.
 Cardiovascular Innovations and Applications2018年1期
Cardiovascular Innovations and Applications2018年1期
- Cardiovascular Innovations and Applications的其它文章
- Mitral Stenosis: A Review
- Functional Tricuspid Regurgitation and Ring Annuloplasty Repair
- Misdiagnosed Aortic Intramural Hematoma and the Role of Intravascular Ultrasound Imaging in Detection of Acute Aortic Syndrome: A Case Report
- Management of Mitral Regurgitation in a Patient Contemplating Pregnancy
- Clinical Evaluation of a Patient with Asymptomatic Severe Aortic Stenosis
- Low-Gradient, Low Ejection Fraction SevereAortic Stenosis: Still a Management Conundrum
