Clinical Evaluation of a Patient with Asymptomatic Severe Aortic Stenosis
Jared G. Breyley, MD and Brian R. Lindman, MD, MSCI
1Vanderbilt University Medical Center, Nashville, TN, USA
Introduction
A 70-year-old man is seen for evaluation of a heart murmur heard by his primary care provider. The patient plays doubles tennis twice per week and claims to be asymptomatic.
– Medication: amlodipine for hypertension.
– Physical examination (PE): pulse 82 bpm; blood pressure 140/90 mmHg.
– Neck: neck veins flat. Carotids delayed.
– Chest: clear.
– Cardiovascular: grade 2/6 late peaking systolic ejection murmur.
– Extremities: normal pulses.
– Echocardiogram: heavily calci fied aortic valve.Peak jet velocity 4.6 m/s. Aortic valve area 0.7 cm2. Right ventricular systolic pressure not obtainable.
Commentary
Aortic stenosis (AS) is one of the most common valvular diseases, with a prevalence of 3.4% in adults older than 75 years [1]. AS is considered a surgical disease in that the only treatment known to reduce mortality is AVR, by either a surgical or a transcatheter approach. While current guidelines provide clear evidence-based recommendations for treatment of symptomatic patients, it remains less clear how to treat patients with severe AS who are asymptomatic [2–4]. This case describes an elderly man without a signi ficant medical history who is found to have severe AS. The patient reports no symptoms, has no evidence of heart failure on PE,and is noted to be physically active. Further evaluation is needed to determine the most appropriate treatment.
Symptomatic severe AS is a class I indication for AVR [2–4]. However, symptoms related to AS are often vague, and a thorough history is crucial in the evaluation of these patients. In the absence of classic symptoms such as angina, syncope, or heart failure, patients may report only fatigue. Commonly,older adults with AS may dismiss subtle symptoms as simply related to aging or may restrict their physical activity without realizing it as a means of compensating. Up to 50% of patients with severe AS are asymptomatic at the time of diagnosis [5]. Despite patients being asymptomatic, current guidelines provide class I indications for AVR in the setting of left ventricular ejection fraction less than 50%or the need for concomitant cardiac surgery. Our patient seems to be asymptomatic, presumably with normal left ventricular function; however, careful review of his physical activity (tennis) should be considered. Has he switched from singles to doubles tennis because of decreased exercise tolerance? Has he reduced the number of days he plays per week?
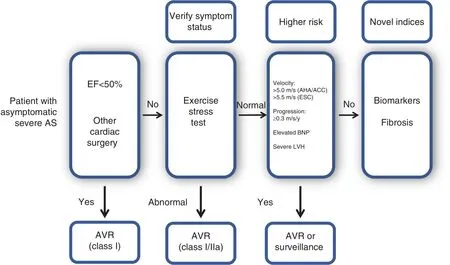
Figure 1 Evaluation and Treatment of the Patient with Asymptomatic Severe Aortic Stenosis (AS).
There are also several class II indications for AVR as depicted in Figure 1. Class IIa indications for AVR include patients with very severe AS de fined as a peak velocity of 5 m/s or greater(American Heart Association/American College of Cardiology) or 5.5 m/s or greater (European Society of Cardiology, ESC), assuming low operative risk. Our patient does not meet either of these thresholds for very severe AS. The American Heart Association/American College of Cardiology guidelines also include rapid progression (peak velocity increase 0.3 m/s or more per year) as a class IIb indication [2, 3]. However, the ESC guidelines report this as a class IIa indication [4]. The 2017 ESC guidelines included a class IIa indication for AVR in the setting of “markedly elevated BNP levels.” It has been shown that amino-terminal prohormone of BNP provides prognostic information regarding clinical events such as surgery, hospitalization, heart failure, syncope, and death [6, 7].Currently, there is no clear cutoff value for natriuretic peptide levels to prompt a recommendation for AVR in an asymptomatic patient. Left ventricular hypertrophy (LVH) is a compensatory response to the pressure overload created by severe AS, but there are adaptive and maladaptive aspects to this hypertrophic remodeling [8, 9]. It has been shown that patients with signi ficant LVH have increased operative mortality and morbidity [10, 11]. The 2012 ESC guidelines included “excessive LVH in the absence of hypertension” as a class IIb indication for AVR, but this was not included in the most recent guidelines [4, 12].
Historically, exercise testing has been considered dangerous in patients with severe AS, and remains contraindicated in patients who are symptomatic.However, it has been found to be helpful in providing prognostic information and unmasking symptoms in patients who are purportedly asymptomatic[13]. Despite being a class IIa recommendation,exercise testing remains underused in patients with severe AS. In one study it was reported that exercise testing was performed in only 5.7% of asymptomatic patients with severe AS [14]. The importance of exercise testing was demonstrated in a meta-analysis that reported no episodes of sudden cardiac death in asymptomatic patients with normal exercise treadmill test (ETT) results. However,patients with abnormal ETT results were found to have a 5% risk of sudden cardiac death after 1 year of follow-up. Additionally, an increased risk of adverse cardiac events in patients with abnormal ETT results was reported (21% vs. 66%) [15].The overall incidence of abnormal test results was reported to range from 28 to 67% (mean 49%).The criteria for a positive exercise test are debated but generally include development of symptoms, a decrease in blood pressure with exercise or failure to increase systolic blood pressure by 20 mmHg,inability to reach 80% of predicted exercise tolerance, development of signi ficant ST depression,and/or ventricular arrhythmias. The onset of symptoms during an ETT is a class I indication for AVR,and decreased exercise tolerance or a decrease in blood pressure with exercise are class IIa indications for AVR [2, 12].
Novel approaches to risk stratifying patients with asymptomatic severe AS include levels of circulating biomarkers and myocardial fibrosis. Multiple biomarkers have been extensively studied in patients with heart failure. BNP is an independent predictor of death in patients with AS [16]. We proposed the use of a multimarker panel to aid in risk strati fication of patients with severe AS. This panel included growth differentiation factor 15, soluble ST2, and amino-terminal prohormone of BNP. Patients with elevations of the levels of all three biomarkers were at signi fi-cantly increased risk of all-cause death after AVR(adjusted hazard ratio 4.59, 95% con fidence interval 1.97–10.71,P<0.001) [17]. Myocardial fibrosis has also been found to be an independent predictor of death in patients with moderate/severe AS [18].Unfortunately, evaluation of myocardial fibrosis with cardiac MRI is expensive and not available in many centers.
Our case presents an older man without a signi fi-cant medical history who is found to have severe AS without any apparent symptoms. If the history is convincing and detailed regarding the extent of exertion without change over a sustained period,many clinicians may not pursue a stress test for con firmation. However, if there is any doubt regarding the history (and, in most cases, there is some doubt), further evaluation with an ETT should be pursued. If the ETT findings are normal, there remains clinical equipoise for whether or not early AVR should be performed. Beyond stress testing, looking for additional “ flags of risk”will be helpful to inform the decision regarding the timing of AVR. These flags may include very severe AS, rapid progression, an elevated natriuretic peptide level, the presence of myocardial fibrosis, marked LVH, or exercise-induced pulmonary hypertension.
Advocates for AVR in the asymptomatic patient contend that valve replacement is inevitable and that we are only waiting for bad things to happen (e.g., sudden death, myocardial dysfunction).Unloading the heart with valve replacement sooner will prevent ongoing damage to myocardial structure and function, which may optimize long-term heart function and freedom from heart failure. Even with close follow-up, symptom onset can occur suddenly and be quite severe [19]. Progressive improvements in operative and postoperative care and the introduction of less invasive ways to replace the valve have decreased the risks of intervention. Nonetheless, complications, including stroke and death, occur as a result of AVR. Further,the implantation of a valve prosthesis introduces the possibility of valve dysfunction and degeneration, with associated morbidity and death. Both sides of this dilemma regarding the optimal timing of AVR for asymptomatic patients have been widely debated and advocated in the literature [20,21]. A strategy trial is needed to answer this important clinical question. Relevant to this, the EARLY TAVR trial (NCT03042104) has recently begun enrolling patients with severe asymptomatic AS.This multicenter trial will enroll 1109 participants and randomize them to undergo early valve replacement (with transcatheter AVR) versus clinical surveillance until the onset of symptoms, when AVR would be performed. Participants will be screened with an exercise stress test, and only those with normal exercise test results will be randomized. If our patient had normal ETT results, he would be a potential candidate for this important trial, which should provide critical guidance to decision making regarding the timing of valve replacement in asymptomatic patients with severe AS.
Conflict of Interest
Brian R. Lindman has received research grants from Edwards Lifesciences and Roche Diagnostics and has consulted for Medtronic and Roche Diagnostics.
REFERENCES
1. Osnabrugge RL, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, LeReun CM, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol 2013;62(11):1002–12.
2. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP,Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(23):e521–643.
3. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease:a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol2017;135(25):e1159–95.
4. Baumgartner H, Falk V, Bax JJ,De Bonis M, Hamm C, Holm PJ,et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease: the Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2017. Online publishahead-of-print 26 August 2017.
5. Genereux P, Stone GW, O’Gara PT, Marquis-Gravel G, Redfors B, Giustino G, et al. Natural history, diagnostic approaches, and therapeutic strategies for patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol 2016;67(19):2263–88.
6. Farre N, Gomez M, Molina L,Cladellas M, Blé M, Roqueta C, et al. Prognostic value of NT-proBNP and an adapted monin score in patients with asymptomatic aortic stenosis. Rev Esp Cardiol2014;67(1):52–7.
7. Bergler-Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G,Gabriel H, et al. Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 2004;109(19):2302–8.
8. Kupari M, Turto H, Lommi J.Left ventricular hypertrophy in aortic valve stenosis: preventive or promotive of systolic dysfunction and heart failure? Eur Heart J 2005;26(17):1790–6.
9. Carabello BA. Is cardiac hypertrophy good or bad? The answer, of course, is yes. JACC Cardiovasc Imaging 2014;7(11):1081–3.
10. Duncan AI, Lowe BS, Garcia MJ,Xu M, Gillinov AM, Mihaljevic T, et al. In fluence of concentric left ventricular remodeling on early mortality after aortic valve replacement. Ann Thorac Surg 2008;85(6):2030–9.
11. Mehta RH, Bruckman D, Das S,Tsai T, Russman P, Karavite D, et al.Implications of increased left ventricular mass index on in-hospital outcomes in patients undergoing aortic valve surgery. J Thorac Cardiovasc Surg 2001;122(5):919–28.
12. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology, European Association for Cardio-Thoracic Surgery,Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33(19):2451–96.
13. Redfors B, Pibarot P, Gillam LD,Burkhoff D, Bax JJ, Lindman BR,et al. Stress testing in asymptomatic aortic stenosis. Circulation 2017;135(20):1956–76.
14. Iung B, Baron G, Butchart EG,Delahaye F, Gohlke-Bärwolf C,Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: the Euro Heart Survey on Valvular Heart Disease.Eur Heart J2003;24(13):1231–43.
15. Ra fique AM, Biner S, Ray I,Forrester JS, Tolstrup K, Siegel RJ. Meta-analysis of prognostic value of stress testing in patients with asymptomatic severe aortic stenosis. Am J Cardiol 2009;104(7):972–7.
16. Clavel MA, Malouf J, Michelena HI, Suri RM, Jaffe AS, Mahoney DW, et al. B-type natriuretic peptide clinical activation in aortic stenosis: impact on longterm survival. J Am Coll Cardiol 2014;63(19):2016–25.
17. Lindman BR, Breyley JG, Schilling JD, Vatterott AM, Zajarias A,Maniar HS, et al. Prognostic utility of novel biomarkers of cardiovascular stress in patients with aortic stenosis undergoing valve replacement. Heart 2015;101(17):1382–8.
18. Dweck MR, Joshi S, Murigu T, Alpendurada F, Jabbour A,Melina G, et al. Midwall fibrosis is an independent predictor of mortality in patients with aortic stenosis. J Am Coll Cardiol 2011;58(12):1271–9.
19. Zilberszac R, Gabriel H, Schemper M, Laufer G, Maurer G, Rosenhek R. Asymptomatic severe aortic stenosis in the elderly. JACC Cardiovasc Imaging2017;10(1):43–50.
20. Carabello BA. Aortic valve replacement should be operated on before symptom onset. Circulation 2012;126(1):112–7.
21. Shah PK. Severe aortic stenosis should not be operated on before symptom onset. Circulation 2012;126(1):118–25.
 Cardiovascular Innovations and Applications2018年1期
Cardiovascular Innovations and Applications2018年1期
- Cardiovascular Innovations and Applications的其它文章
- Mitral Stenosis: A Review
- Functional Tricuspid Regurgitation and Ring Annuloplasty Repair
- Misdiagnosed Aortic Intramural Hematoma and the Role of Intravascular Ultrasound Imaging in Detection of Acute Aortic Syndrome: A Case Report
- Management of Mitral Regurgitation in a Patient Contemplating Pregnancy
- An Asymptomatic Patient with Severe Mitral Regurgitation
- Low-Gradient, Low Ejection Fraction SevereAortic Stenosis: Still a Management Conundrum
