Lesson Eighty-two Eccentric atrial activation during a narrow QRS tachycardia:what is the mechanism?
A 49-year-old woman presented with a 2-year history ofrecurrentpalpitationsand documented episodes of paroxysmal supraventricular tachycardia(SVT)terminated with adenosine.Resting 12-lead electrocardiogram (ECG)revealed normal sinus rhythm without preexcitation.She had a structurally normal heart on echocardiogram.After having obtained an informed consent,an electrophysiology study was performed using standard technique and a decapolar coronary sinus(CS)catheter was inserted with the distal pole positioned at the lateral mitral annulus(Figure 1A).Baseline measurements revealed a sinus cycle length of 804 milliseconds and an atrial-His(AH)interval and His-ventricular (HV)of 72 and 36 milliseconds,respectively.Incremental ventricular pacing showed eccentric retrograde atrialactivation with earliest activation noted at CS bipolar pair 3-4.Although atrial activation was earlier on the more distal CS electrodes versus the His bundle electrode,the difference in activation between CS 3-4 and CS 4-5 was minimal(Figure 1B).The ventricular-atrial(VA)conduction was decremental. Programmed atrial extrastimulation established the presence of anterograde dual AV nodal physiology with an AH jump of 78 milliseconds.A narrow QRS complex tachycardia with a cycle length varying between 440 and 460 millisecondswas reproducibly induced with programmed atrial stimulation.The retrograde atrial activation sequence was eccentric and identical to that observed during ventricular pacing.Overdrive ventricular pacing during the tachycardia resulted in a VAV response(Figure 1B).Premature ventricular complexes (PVCs)introduced during SVT to scan diastole preexcited the atrium with a preexcitation index of 125 milliseconds.What is the mechanism of the tachycardia?
Commentary
An eccentric retrograde atrial activation sequence with earliest atrial activation at or near the lateral mitral annulus suggests retrograde conduction over a concealed left free wall accessory pathway (AP) during atrioventricular reentrant tachycardia(AVRT).The atrial activation during ventricular pacing was also eccentric and identicalto thatduring the SVT.Although extremely uncommon,the possibility of an atypical atrioventricular nodal reentrant tachycardia(AVNRT)with eccentric retrograde atrial activation remains in the differential diagnosis.A left atrial focal tachycardia was eliminated by the V-A-V response during ventricular overdrive pacing.
Because the pattern of atrial activation alone,even when it is eccentric as in this case,does not definitively rule out AVNRT,other maneuvers are required to establish a diagnosis. Postpacing interval(PPI)-tachycardia cycle length(TCL)was 138 milliseconds,and stimulus to atrial interval-VA tachycardia(SA-VA)was 122 milliseconds with a basal right ventricular(RV)pacing site(Figure 1B),findings that are more consistent with AVNRT than AVRT.However,these observations do not exclude AVRT with a slowly conducting decremental AP.These ventricular entrainment criteria depend on nondecrementalretrograde conduction through an AP and are limited in differentiating atypical AVNRT from AVRT using decrementally conducting AP.Furthermore,in the setting of AVRT employing a left lateral AP,the PPI-TCL,and SA-VA interval differences may be longer simply by virtue of the distance of the RV pacing site from the circuit.The preexcitation index in this case was 125 milliseconds,a number usually suggesting AVNRT.However,studies utilizing the concept ofpreexcitation index to differentiate AVNRT from AVRT did not include patients with decremental pathways or atypical AVNRT and hence cannotbe used to differentiate the tachycardia mechanism in this case.Intravenous adenosine to differentiate nodal versus AP retrograde conduction was not used,as retrograde decremental pathways can be adenosine sensitive and the response would not have helped in elucidating the tachycardia mechanism.
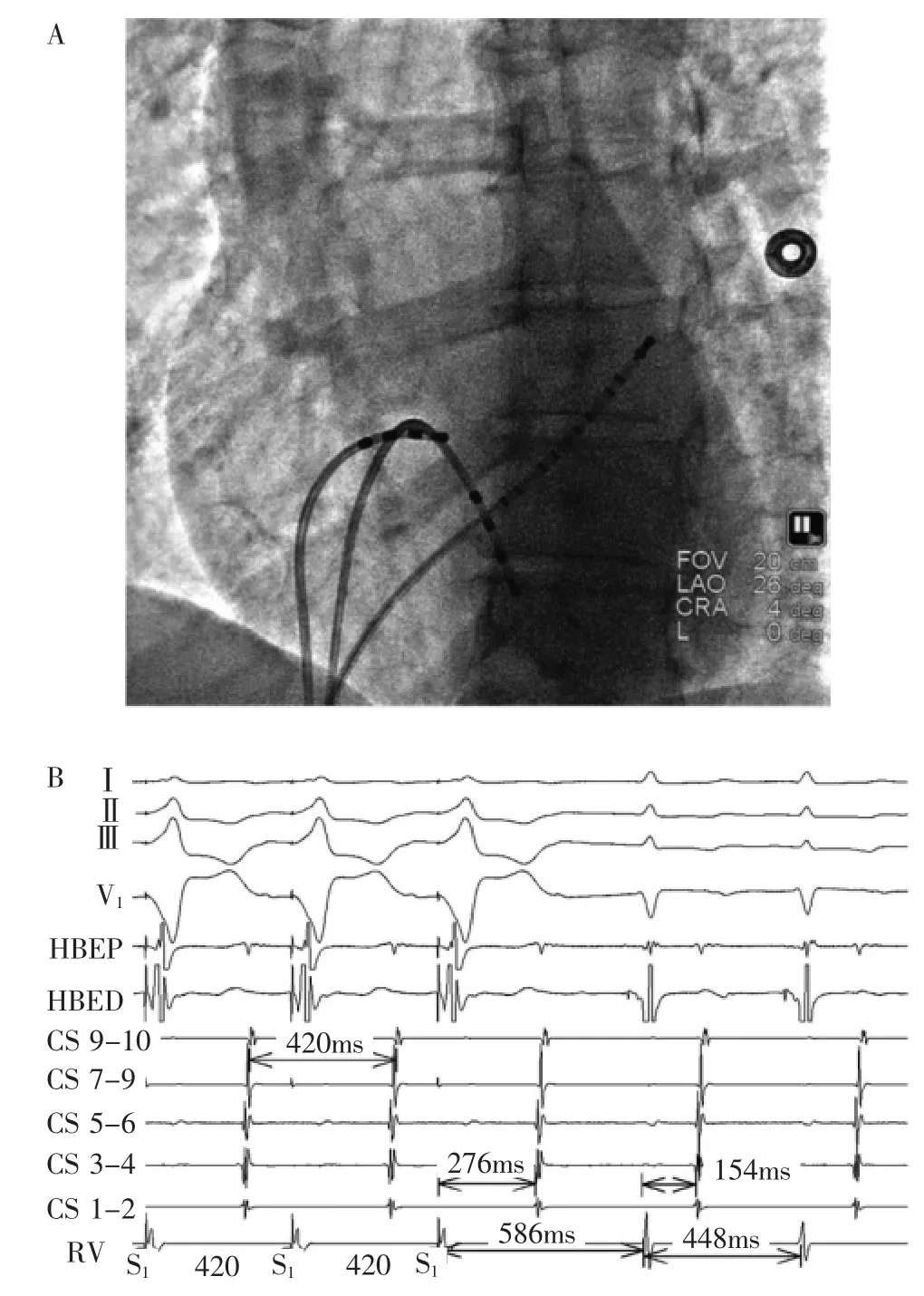
Figure1 A:The catheter positions during diagnostic electrophysiology study with the most distal pole of the CS catheter positioned at the lateral mitral annulus.B:Response to ventricular overdrive pacing during SVT with recordings from surface leads I,II,III,and V1 and intracardiac electrogramsfrom the proximalHis bundle,distal His bundle,proximal to distal coronary sinus (CS 9-10 to CS 1-2,respectively),and right ventricular(RV)apex are displayed.
How do we definitively establish the route of retrograde conduction?Lack of positive proofs of AP conduction including response to PVC timed to His,HV change predicting HA change and bundle branch block resulting in VA change do not rule out its presence.In the case of left free wall APs,the PVCs often need to be delivered early again,since the RV pacing site is often distant from the tachycardia circuit.As the retrograde conduction was eccentric and identical during SVT and ventricular pacing,we used maneuvers to establish whetherthe retrograde conduction was occurring through AV node or AP during ventricular pacing.Programmed ventricular stimulation at 600 milliseconds CL with a S2 of 330 milliseconds showed the sudden appearance of a retrograde His with the similar eccentric atrial activation.With progressively earlier ventricular extrastimuli the increase in VA interval paralleled the increase of retrograde ventricular to His(VH)interval with no change in HA interval(Figure 2).This pattern of VA conduction with the same eccentric atrial activation confirmed retrograde conduction over the AV node and not an AP.One would not expect a constant HA relationship during retrograde conduction over an AP unless there happened to be equal decrement in VH conduction and retrograde AP conduction,a highly unlikely possibility.Parahisian pacing resulted in an SA interval of 172 milliseconds with His bundle and local myocardium capture while SA intervalwas204 milliseconds with ventricular myocardium capture only without change in retrograde atrial activation sequence(Figure 3).This was highly suggestive of retrograde AV nodal conduction,but did not exclude the possibility of a left free wall AP.
Radiofrequency ablation(RFA)of AVNRT was attempted in the right posteroinferior septum near the CS ostium.Difficulty in tracking VA conduction during RFA resulted in switching to cryoablation.The successful site was slightly anterior to the CS ostium and was anatomically far off from earliest atrial activation.Postablation,the tachycardia could not be reinduced and there was no evidence of anterograde slow pathway conduction with absent VA conduction at all pacing cycle lengths.This case illustrates the importance of relying on electrophysiological evidence rather than patterns in establishing mechanisms of tachycardia.
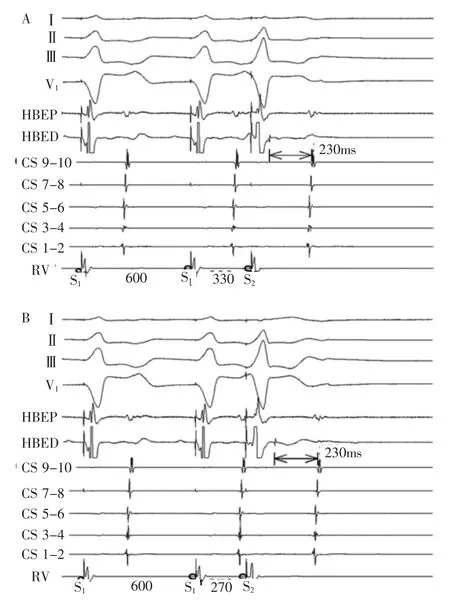
Figure 2 Programmed ventricular stimulation.In the lefthand panel with S1S2of 330 milliseconds,the H2A2interval is 230 milliseconds.In the right panel,a S1S2of 270 milliseconds prolongs the V2H2interval with H2A2 interval of 230 milliseconds.The abbreviations are as in Figure 1.
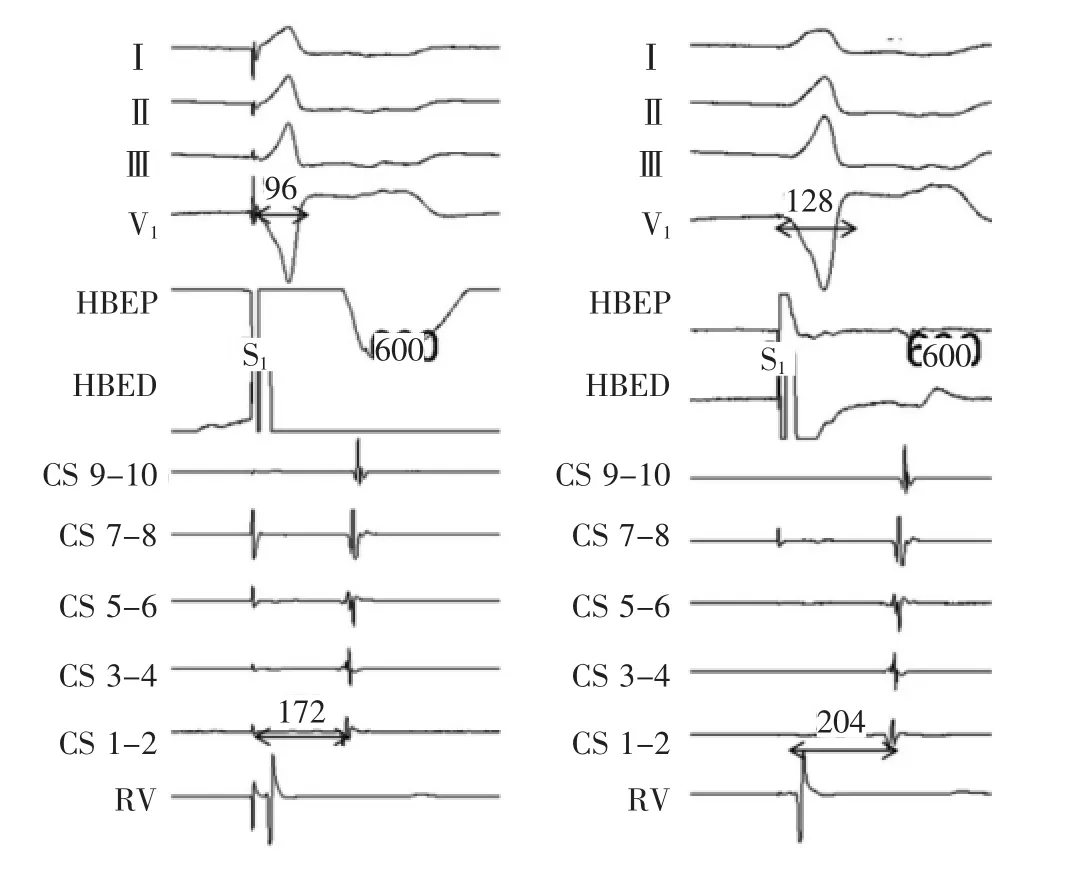
Figure 3 Parahisian pacing.In the lefthand panel with His and ventricular capture (narrow QRS complex),the SA interval is 172 milliseconds.In the righthand panel with ventricular capture only the SA interval is 204 milliseconds(see text for details).Abbreviations as in Figure 1.
词 汇
palpitation n.心悸,心慌,跳动
incremental adj.增加的,增值的,递增的
eccentric adj.偏心的,离心的,反常的,古怪的,n.古怪的人,偏心圆
decremental adj.减少的,递减的
conceal vt.隐藏;隐瞒
entrainment n.夹带,拖带,带走,生物的周期转换
elucidate vt.阐明,说明
proof n.&adj.&vt.证明,证据,校样,考验,验证,试验;防…的,不能透入的,证明用的,耐…的;试验,校对,使不被穿透
maneuver n.&vi.&机动,演习,策略,调遣;演习,调遣,用计谋;机动,演习,用计,调遣
track n.&vt.轨道,足迹,踪迹,小道;追踪,通过,循路而行,留下足迹
cryoablation n.冷冻消融术,冷冻剥脱术
anterograde adj.顺行的,前进的
注 释
1.preexcitation index预激指数,反映心动过速时刚能引起心房预激的期前心室刺激的提前程度,由心动过速周长减期前心室刺激的联律间期计算而得,单位ms。假设心动过速频率为150次/min,那么心动过速的周长为400ms。如刚能进入折返环并引起心房预激的期前心室刺激的联律间期为300ms,那么预激指数为400-300=100ms,即提前100ms的期前心室刺激能进入折返环,提前<100ms的心室刺激不能进入折返环。因此,预激指数常用来判断心室刺激部位与折返环的距离,距离越远,所需提前程度越大,有助于分析折返型心动过速的类型或旁道位置。通常房室结折返型心动过速的预激指数最大,左心室游离壁旁道折返型心动过速的预激指数略小,而间隔部旁道的折返型心动过速的预激指数最小。2.PPI-TCL interval指起搏后间期与心动过速周长之间的差值,其中PPI指最后1个起搏夺获至下一次起搏部位激动之间的时间,反映的是从起搏部位到折返环,通过折返环并返回起搏部位的传导时间,因此,如起搏点距离折返环越近,PPI越短,反之越长。TCL是指折返型心动过速的周长,反映的是通过折返环1周的传导时间。房室折返型心动过速为大折返环,心室肌参与其中,因此,右心室期起搏部位通常距离折返环较近,PPI与TCL间期的差值较小,常<115ms;而房室结折返型心动过速折返环较小,局限在房室结附近,右心室起搏部位通常距离折返环较远,PPI与TCL间期的差值较大,常>125ms。
参考译文
第82课 窄QRS波群心动过速时偏心性心房激动是什么机制?
患者女性,49岁,反复心悸2年,记录到阵发性室上性心动过速(SVT),腺苷中止。静息12导联心电图显示正常窦性心律,无预激。超声心动图检查提示心脏结构正常。签署知情同意书后,采用标准技术行电生理检查,十极冠状窦(CS)电极远端电极位于二尖瓣环外侧(图1A)。基础测试显示窦性心律周长804ms、心房-希氏束间期(AH)和希氏束-心室间期(HV)分别为72ms和36ms。递增心室起搏显示偏心性逆行心房激动,最早激动位于CS电极3-4电极对。虽然CS较远端电极心房激动早于希氏束电极,但CS电极3-4与4-5之间的激动差异最小(图1B)。室房(VA)传导呈递减性。程序心房期外刺激显示AH跳跃78ms,证实存在房室结前向双径路。程序心房刺激能重复诱发周长为440~460ms的窄QRS波群心动过速。逆行心房激动顺序呈偏心性,与心室起搏时见到的相一致。心动过速期间超速心室起搏引发VAV反应(图1B)。SVT期间扫描舒张期的期前室性刺激(PVCs)预激心房,预激指数为125ms。心动过速的机制是什么?
分析讨论
偏心性逆行心房激动顺序、最早心房激动位于或接近二尖瓣环外侧,提示房室折返型心动过速(AVRT)经左侧游离壁隐性旁道(AP)逆传。心室起搏时心房的激动也是偏心性的,与SVT时相一致。虽然极不常见,鉴别诊断中仍然要考虑不典型房室结折返型心动过速(AVNRT)的可能性。心室超速起搏时的VAV反应排除了灶性房性心动过速。
鉴于单一的心房激动图形,即使像本例一样呈偏心性顺序,不能确切排除AVNRT,因此,需要其他方法去确定诊断。右心室基底部起搏,起搏后间期(PPI)-心动过速周长(TCL)为138 ms,起搏刺激心房间期-VA心动过速(SA-VA)为122ms(图1B),这些数值与AVNRT的一致性高于AVRT。然而,这些观察不能排除经递减性AP缓慢传导的AVRT。这些心室拖带标准依赖经AP的非递减性逆行传导,对非典型AVNRT与经AP递减性传导AVRT的鉴别作用有限。此外,对于经左外侧AP的AVRT,PPI-TCL以及SA-VA间期可因右心室起搏部位与折返环的距离而较长。本例的预激指数为125ms,这一数值通常提示为AVNRT。然而,利用预激指数概念去鉴别AVNRT与AVRT的研究并非包含递减旁道或非典型AVNRT患者,因此,不能用于鉴别本例的心动过速机制。没有静注腺苷去鉴别房室结与旁道逆传,因为逆传递减旁道对腺苷敏感,其反应无助于阐明心动过速机制。
我们该如何确定逆传途径?缺乏AP传导的阳性证据包括对适配希氏束的PVC反应、预示HA变化的HV变化以及引起VA变化的束支阻滞,不能排除它的存在。存在左侧游离壁AP的情况下,常需要更早的PVC,因右心室起搏部位经常远离心动过速折返环。鉴于SVT与心室起搏时,逆行传导呈偏心性而且一致,我们设法确定心室起搏时是否通过AV结或AP逆行传导。采用600ms周长加330msS2程控心室起搏显示意外出现逆传希氏束和类似的偏心性心房激动。随着心室期外刺激的进行性提前,VA间期的增加与逆传的心室-希氏束间期(VH)增加相平行,而HA无变化(图2)。这一VA传导结合相同的偏心性心房激动图形证实经AV结逆传而非经AP逆传。人们无法期待经AP逆传时有恒定的HA关系,除非碰巧VH传导与逆行AP传导的递减相等,这是极不可能的。希氏束旁起搏引起SA间期172ms伴希氏束和局部心室夺获,而当SA间期204ms时只有心室夺获而无逆传心房激动顺序改变(图3)。这高度提示经AV结逆传,但不能排除左侧游离壁AP的可能性。
于右后下间隔近CS口处行AVNRT射频消融。射频消融期间难以跟踪VA传导,改用冷冻消融。成功消融部位位于CS口略前方,解剖上远离最早心房激动部位。消融后,于所有周长起搏下,不能再次诱发心动过速,无前向慢径传导和VA传导。本例阐明了依靠电生理依据而非图形确定心动过速机制的重要性。
图1 A:诊断性电生理检查中导管位置,冠状窦最远端电极位于二尖瓣环外侧。BSVT时对心室超速起搏的反应,记录顺序为体表Ⅰ、Ⅱ、Ⅲ和V1,心内电图为希氏束近端,希氏束远端,冠状窦由近及远(分别为 CS9-10到CS1-2),右心室(RV)尖。
图2 程控心室刺激。上图:S12300ms,H2A2间期为230ms,下图:S1S2270ms,延长 V2H2而 H2A2为 230ms。
图3 希氏束旁起搏。左图为希氏束和心室夺获(窄QRS波群),SA间期172ms,右图为只有心室夺获,SA间期204ms。
[1]Bagga S,Padanilam BJ,Prystowsky EN.Eccentric Atrial Activation During a Narrow QRS Tachycardia:What Is the Mechanism?[J].J Cardiovasc Electrophysiol,2016,27∶1353-1355.

