急进高原后男性官兵心功能的变化及其与AMS的关系*
易元月, 刘 宝, 吴 刚, 高钰琪
(第三军医大学高原军事医学系高原特需药品与卫生装备研究室, 高原环境医学教育部重点实验室, 全军高原医学重点实验室, 重庆 400038)
急进高原后男性官兵心功能的变化及其与AMS的关系*
易元月, 刘 宝, 吴 刚, 高钰琪△
(第三军医大学高原军事医学系高原特需药品与卫生装备研究室, 高原环境医学教育部重点实验室, 全军高原医学重点实验室, 重庆 400038)
目的评价驻平原官兵急进高原前后心功能的变化情况并探讨其与急性高山病(AMS)的关系。方法采用超声心动图评价42名健康青年男性官兵进入高原前及快速进入高原后(3 658 m,3 d)的心脏功能,同时观察心率、血压和血氧饱和度等生理指标的变化,以及进入高原后AMS的发病情况。结果与进入高原前相比,青年男性官兵急进高原后,左房收缩末期内径和左室舒张末期内径显著减小,右房收缩末期内径显著减小,右室流出道和肺动脉内径显著增宽,射血分数显著增大,心输出量显著增多,肺动脉收缩压及平均肺动脉压显著增高,二尖瓣E峰流速显著降低(P<0.05)。进入高原后,42人中有15人发生AMS(AMS组),27人未发病(non-AMS组)。比较2组官兵在平原的心功能发现,AMS组的主动脉窦部内径和左室舒张末期内径显著小于non-AMS组,肺动脉收缩压显著高于non-AMS组。比较2组官兵进入高原后的心功能发现,AMS组左房收缩末期内径显著小于non-AMS组(P<0.05)。AMS评分与进入高原前的心输出量呈显著负相关性(r=-0.3814,P<0.05)。结论青年男性官兵从平原快速进入高原后,右心功能受损合并左心功能代偿;在平原运用超声心动图进行肺动脉收缩压及心输出量的检查有助于AMS易感人群的筛选。
急性高山病; 左心室; 代偿; 超声心动图
近年来,随着高原地区社会经济发展和国防建设需要,越来越多的人从平原进入高原[1-3]。高原中大气压力随着海拔高度的增加而降低,大气中的氧分压也随之降低,引起动脉氧分压和氧饱和度降低[4-5]。为了习服高原的低气压低氧环境,机体会在神经体液内分泌的作用下,围绕着氧的摄取、运输和利用等,发生一系列代偿适应性变化,呼吸增快、通气量增加、心率增快及心输出量增多都是机体对高原低氧环境的习服性反应[6]。多数人通过代偿可获得对高原环境的良好习服,但也有部分人因习服不良发生各种高原病[7]。急性高山病(acute mountain sickness,AMS)又称急性高原反应,是最常见的急性高原病,影响人员健康,严重时可发展为高原脑水肿等重症急性高原病,危及生命,有关AMS的发病机制至今仍不十分清楚[5, 7-8]。为此,本文采用超声心动图等技术方法,比较观察了健康青年男性官兵从平原快速进入高原环境前后心功能的改变,并分析了其与AMS发病之间的关系,旨在为揭示AMS的发病机制提供实验依据。
材 料 和 方 法
1 实验对象
此项研究总共招募了42名健康青年男性官兵。42人中有5人在进入高原后二尖瓣舒张期峰值流速为单峰,因此在比较官兵二尖瓣舒张期峰值流速时只纳入了37例。42人中在进入高原前后超声心动图显示均有三尖瓣返流的共有23人,因此只有这23人可以通过三尖瓣返流情况估测肺动脉收缩压(pulmonary arterial systolic pressure, PASP)并比较自身进入高原前后PASP的变化。42人平均年龄、身高及体重分别是(24.31±4.44)(20~48)岁、(172.93±5.94)(162~188)cm和(66.07±7.52)(52~86)kg。本研究排除入选受试者有呼吸系统疾病、心血管疾病、恶性肿瘤、肝肾功能障碍和免疫系统疾病以及不能完成调查问卷的精神疾病患者。所有受试者均无高原暴露史。此外,所有受试者在入高原前1个月之内均无药物史及介入手术史。此项研究经第三军医大学第二附属医院伦理委员会批准。所有受试者均被告知此研究的背景、目的、步骤、风险和获益并签署了知情同意书。
2 方法
2.1实验设计 42名受试者耗时约43 h由平原(重庆,海拔500 m)乘火车到达高原(拉萨,海拔3 658 m)。研究者在急进高原前3天与到达高原第3天均对受试者进行体格检查[心率(heart rate, HR)、血压和动脉血氧饱和度(arterial oxygen saturation, SaO2)]与超声心动图检查(Philips CX50便携式彩色多普勒超声诊断仪,探头型号S5-1,探头频率2.5 MHz),并指导受试者进行路易斯湖评分(Lake Louise scoring,LLS)量表填写。
2.2超声检测 受试者取左侧卧位,操作者经二维超声心动图测量其主动脉窦部内径(aortic sinus diameter,AO)、左房收缩末期内径(left atrial end-systolic dimension,LADs)、左室舒张末期内径(left ventricular end-diastolic dimension,LVDd)、右室前后径(right ventricular anteroposterior dimension,RVDa)、室间隔厚度(interventricular septum thickness,IVS)、左室后壁厚度(left ventricular posterior width,LVPW)、右室流出道内径(right ventricular outflow tract diameter,RVOT)、肺动脉内径(pulmonary artery dimension,PAD)、右房收缩末期内径(right atrial end-systolic dimension,RADs)和右室收缩末期内径(right ventricular end-systolic dimension,RVDs);M型超声测量缩短分数(fractional shortening,FS)和射血分数(ejection fraction,EF);脉冲式多普勒测量主动脉流速(aortic velocity,AV)、肺动脉流速(pulmonary arterial velocity, PV)、二尖瓣E峰流速(mitral peak E velocity,MVE)和二尖瓣A峰流速(mitral peak A velocity, MVA)。根据测量数据及相关公式计算每搏输出量(stroke volume,SV)、心输出量(cardiac output,CO)、PASP及平均肺动脉压(mean pulmonary arterial pressure,MPAP)。每项数据采集均取3个心动周期的平均值。
2.3AMS的评估 AMS诊断根据LLS标准[8],包含头痛、头晕、胃肠道症状、睡眠困难以及疲劳和虚弱5个方面的症状。每种症状按照其发生的严重程度分为无、轻、中、重4个等级及相对应的4种评分(0、1、2、3)。发生头痛及总分≥3分可诊断为AMS,发生头痛及总分≥5分为重度AMS。
3 统计学处理
应用SPSS13.0统计软件进行数据分析。计量资料用均数±标准差(mean±SD)表示,在分析急进高原对男性官兵心功能影响时使用自身配对t检验;使用独立样本t检验分析心脏结构和心功能与AMS的关系;用Spearman相关分析考察心功能与AMS的相关性。以P<0.05为差异有统计学意义。
结 果
1 生命体征测量数据
青年男性官兵急进高原后与平原时相比,SaO2显著降低,HR、动脉收缩压(systolic arterial pressure,SAP)、动脉舒张压(diastolic arterial pressure,DAP)和平均动脉压(mean arterial pressure,MAP)均显著增高(P<0.01),见表1。年龄、身高和体重在non-AMS组与AMS组之间的差异没有统计学显著性。无论在平原还是高原,non-AMS组与AMS组之间SaO2、HR、SAP、DAP和MAP的差异均没有统计学显著性,见表2、3。
表1受试官兵在不同海拔的心脏参数比较
Table 1. Cardiac parameters at low and high altitudes (Mean±SD.n=42)
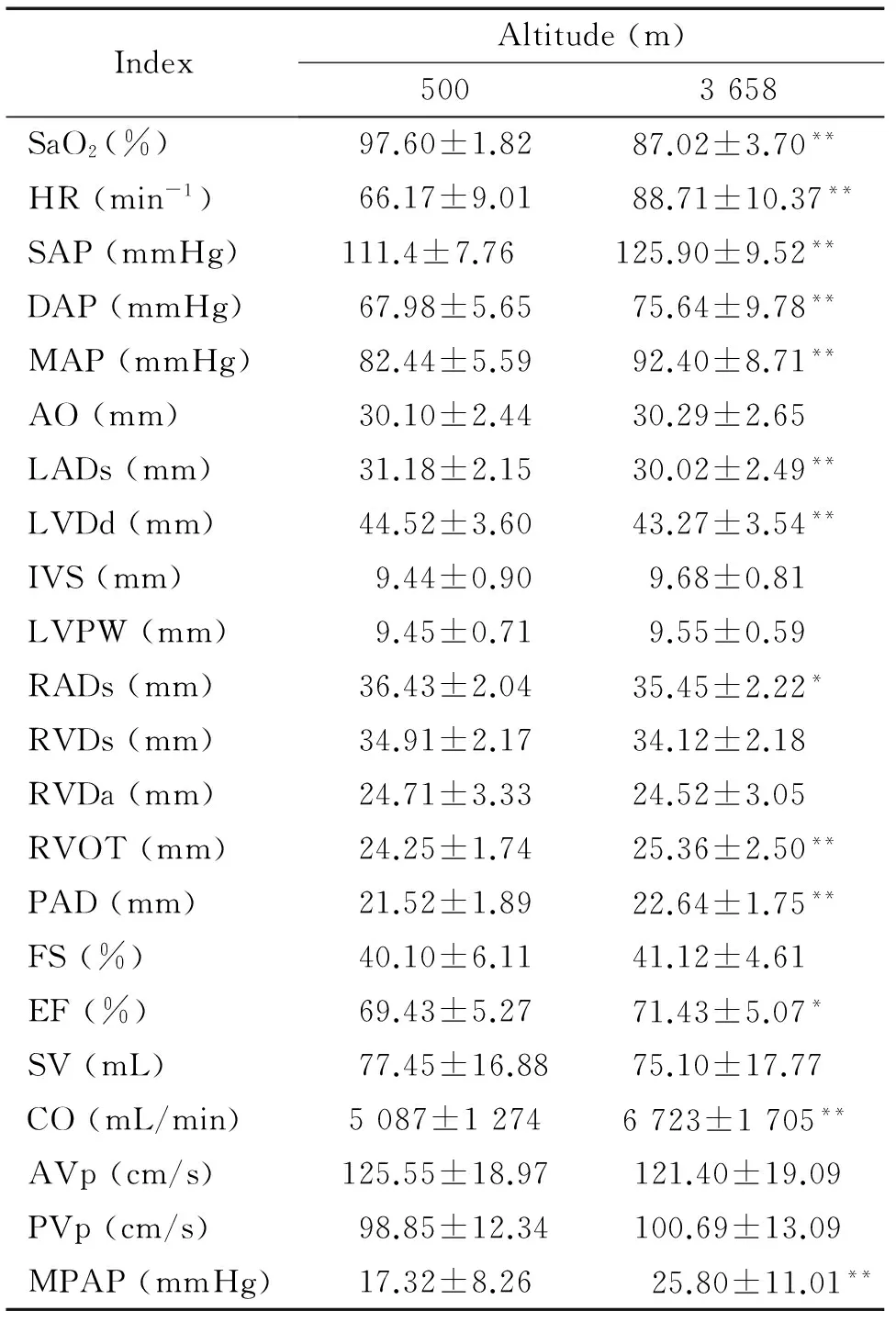
IndexAltitude(m)5003658SaO2(%)97.60±1.8287.02±3.70**HR(min-1)66.17±9.0188.71±10.37**SAP(mmHg)111.4±7.76125.90±9.52**DAP(mmHg)67.98±5.6575.64±9.78**MAP(mmHg)82.44±5.5992.40±8.71**AO(mm)30.10±2.4430.29±2.65LADs(mm)31.18±2.1530.02±2.49**LVDd(mm)44.52±3.6043.27±3.54**IVS(mm)9.44±0.909.68±0.81LVPW(mm)9.45±0.719.55±0.59RADs(mm)36.43±2.0435.45±2.22*RVDs(mm)34.91±2.1734.12±2.18RVDa(mm)24.71±3.3324.52±3.05RVOT(mm)24.25±1.7425.36±2.50**PAD(mm)21.52±1.8922.64±1.75**FS(%)40.10±6.1141.12±4.61EF(%)69.43±5.2771.43±5.07*SV(mL)77.45±16.8875.10±17.77CO(mL/min)5087±12746723±1705**AVp(cm/s)125.55±18.97121.40±19.09PVp(cm/s)98.85±12.34100.69±13.09MPAP(mmHg)17.32±8.2625.80±11.01**
*P<0.05,**P<0.01vs500 m.
2 LLS量表数据
在受试官兵到达海拔3 658 m第3天,根据LLS标准[8],15/42(35.7%)的受试者符合急性高原病标准;其中14/42(33.3%)符合轻微急性高原病标准,1/42(2.38%)符合严重急性高原病标准。所有受试者的平均LLS是1.95±1.79,均未发生高原肺水肿及高原脑水肿。
表2受试官兵的AMS与进入高原前心脏参数的关系
Table 2. Relationship between AMS and cardiac parameters at 500 m (Mean±SD)

IndexNon-AMSAMSSaO2(%)97.77±0.7698.00±0.65HR(min-1)67.33±7.0962.87±11.07SAP(mmHg)111.70±7.61110.70±8.23DAP(mmHg)68.37±5.4967.27±6.05MAP(mmHg)82.83±5.4181.73±6.03AO(mm)30.74±2.3828.93±2.15*LADs(mm)31.44±2.2230.70±2.00LVDd(mm)45.37±3.5443.00±3.27*IVS(mm)9.45±0.989.40±0.74LVPW(mm)9.41±0.809.53±0.52RADs(mm)36.19±2.0436.87±2.03RVDs(mm)34.81±2.3235.07±1.94RVDa(mm)25.04±3.6324.13±2.75RVOT(mm)24.22±1.6924.29±1.87PAD(mm)21.72±1.6921.17±2.22FS(%)39.89±7.0140.47±4.24EF(%)66.41±13.1171.07±5.13SV(mL)80.19±17.8772.53±14.17CO(mL/min)5386±13104549±1042AVp(cm/s)123.63±19.93129.00±17.23PVp(cm/s)99.87±13.4897.00±10.14PASP(mmHg)23.13±4.7227.42±3.00**MPAP(mmHg)17.95±8.3916.18±8.18
n=14 in non-AMS group andn=9 in AMS group for PASP determination;n=27 in non-AMS group andn=15 in AMS group for others.*P<0.05,**P<0.01vsnon-AMS group.
3 急性高原暴露对心功能的影响
青年男性官兵急进高原后与平原时相比,LADs和LVDd均减小,RADs减小,RVOT和PAD增宽,EF增大,CO增多,PASP与MPAP均增高(P<0.01)。而AO、IVS、LVPW、RVDs、RVDa、FS、SV、主动脉血流峰值流速(aortic peak velocity,AVp)和肺动脉血流峰值流速(pulmonary arterial peak velocity,PVp)差异无统计学显著性。官兵急进高原后与平原时相比,MVE降低(P<0.05),MVA的差异无统计学显著性,见图1、2及表1。
4 心功能与AMS评分的关系
AMS组与non-AMS组相比,处于平原时测定的AO数值减小,LVDd减小,PASP增高,差异有统计学意义(P<0.05),见表2。 AMS组与non-AMS组相比,处于高原时测定的LADs减小,差异有统计学意义(P<0.05),见表3。官兵在平原的CO与AMS评分具有负相关性,差异有统计学意义(r=-0.3814,P<0.05),见图3。
表3受试官兵的AMS与进入高原后心脏参数的关系
Table 3. Relationship between AMS and cardiac parameters at 3 658 m (Mean±SD)
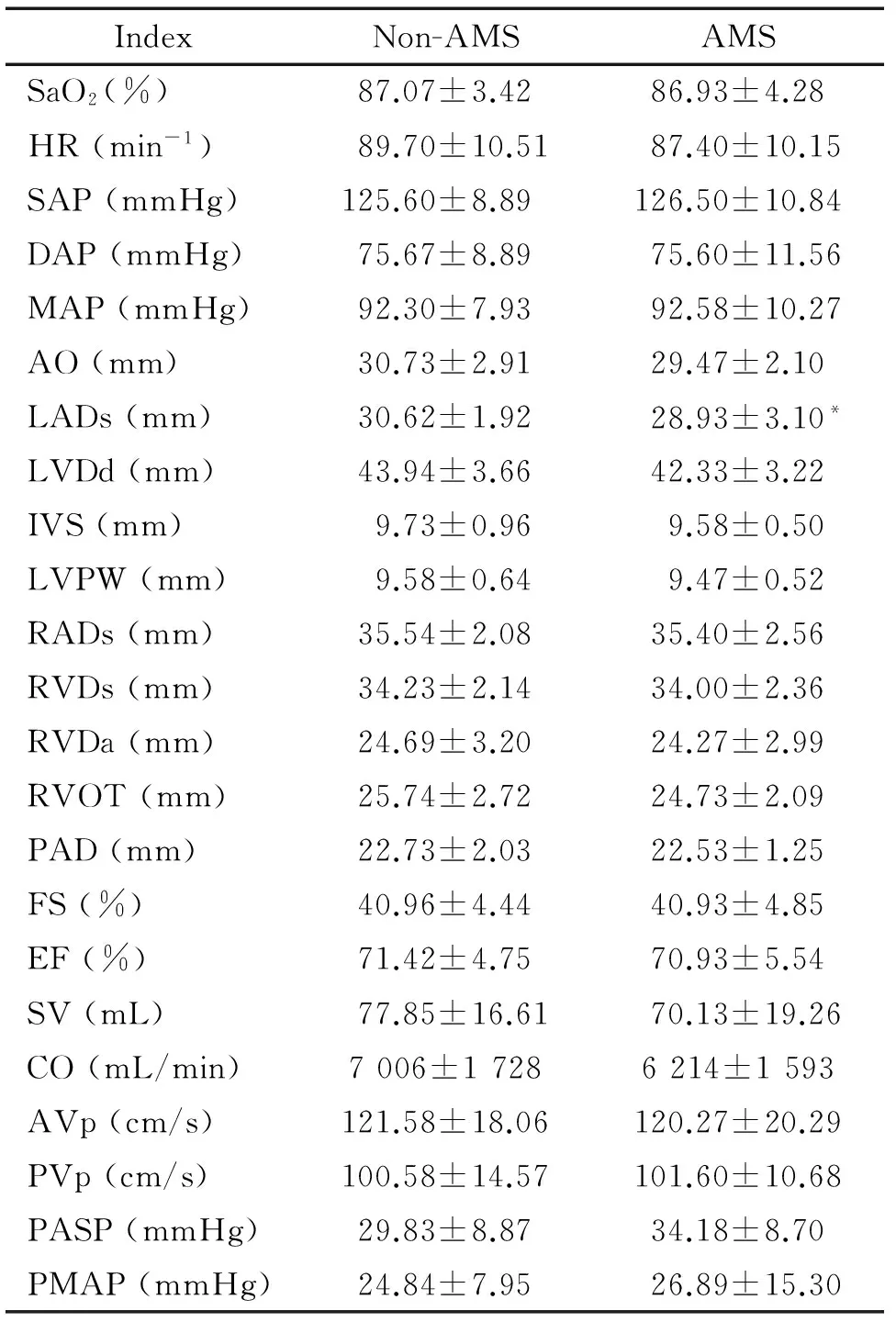
IndexNon-AMSAMSSaO2(%)87.07±3.4286.93±4.28HR(min-1)89.70±10.5187.40±10.15SAP(mmHg)125.60±8.89126.50±10.84DAP(mmHg)75.67±8.8975.60±11.56MAP(mmHg)92.30±7.9392.58±10.27AO(mm)30.73±2.9129.47±2.10LADs(mm)30.62±1.9228.93±3.10*LVDd(mm)43.94±3.6642.33±3.22IVS(mm)9.73±0.969.58±0.50LVPW(mm)9.58±0.649.47±0.52RADs(mm)35.54±2.0835.40±2.56RVDs(mm)34.23±2.1434.00±2.36RVDa(mm)24.69±3.2024.27±2.99RVOT(mm)25.74±2.7224.73±2.09PAD(mm)22.73±2.0322.53±1.25FS(%)40.96±4.4440.93±4.85EF(%)71.42±4.7570.93±5.54SV(mL)77.85±16.6170.13±19.26CO(mL/min)7006±17286214±1593AVp(cm/s)121.58±18.06120.27±20.29PVp(cm/s)100.58±14.57101.60±10.68PASP(mmHg)29.83±8.8734.18±8.70PMAP(mmHg)24.84±7.9526.89±15.30
n=14 in non-AMS group andn=9 in AMS group for PASP determination;n=27 in non-AMS group andn=15 in AMS group for others.*P<0.05vsnon-AMS group.
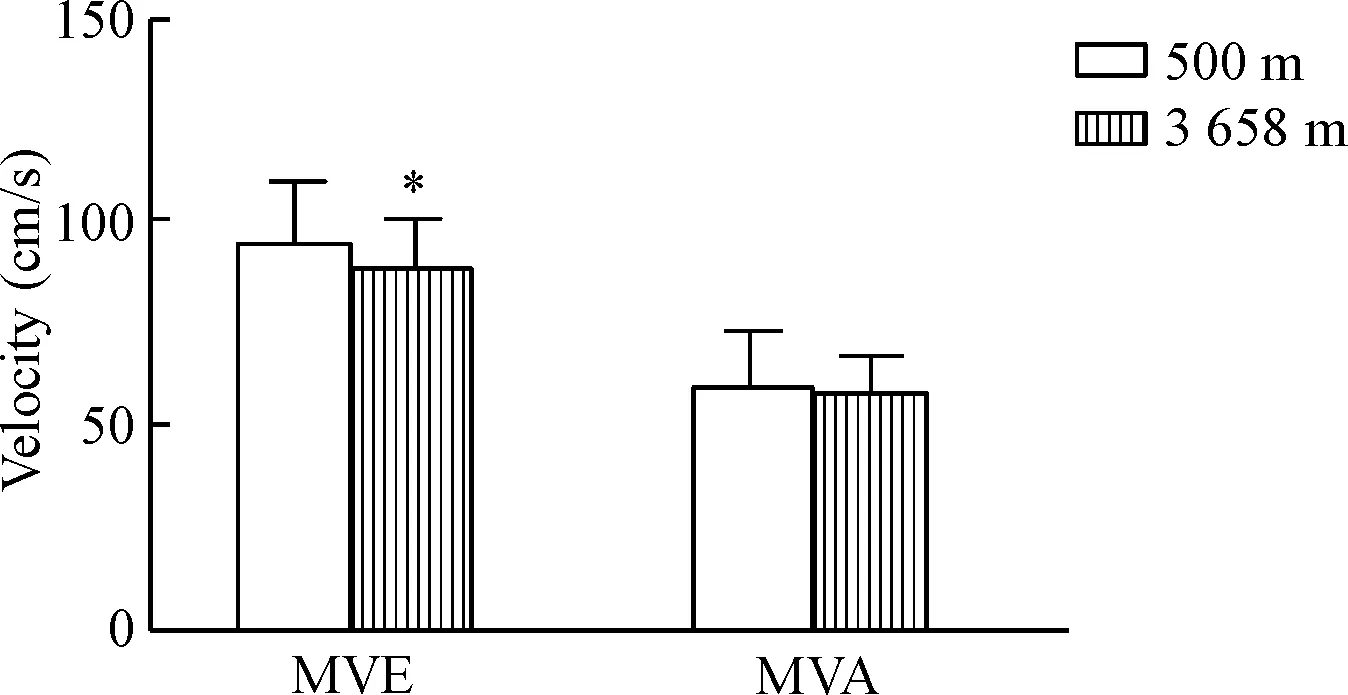
Figure 1. Comparisons of mitral peak E velocity (MVE) and mitral peak A velocity (MVA) in healthy young men at the altitudes of 500 m and 3 658 m. Mean±SD.n=37.*P<0.05vs500 m group.
图1健康青年男性MVE与MVA在急进高原的前后比较

Figure 2. Comparison of the pulmonary arterial systolic pressure (PASP) in healthy young men at the altitudes of 500 m and 3 658 m. Mean±SD.n=23.**P<0.01vs500 m group.
图2健康青年男性肺动脉收缩压在急进高原的前后比较

Figure 3. The correlation analysis of cardiac output (CO) at 500 m and AMS scores at 3 658 m (n=42).
图3AMS评分与进入高原前心输出量的相关性分析
讨 论
急进高原后人体心脏的最初反应是HR加快以及相伴随的CO增加。上世纪早期至今,考虑到高原对国家的社会、经济和军事等方面的重要作用,各国的研究者对人体急进高原前后心功能变化的精确描述问题一直保持着浓厚的兴趣[6]。之前的研究报告指出高原缺氧会使交感神经兴奋性增强从而导致HR的加快[9]。当心率增快时,心动周期(尤其是心室舒张期)缩短,因而心室充盈时间缩短,心室充盈减少(这也许是MVE降低的原因)[10],从而导致LADs、LVDd和RADs减小。
根据高钰琪[4]描述的标准,肺动脉高压是指肺动脉压的异常增高,收缩压>30 mmHg,舒张压>15 mmHg,平均肺动脉压>20 mmHg。此次受试者急进高原后PASP和MPAP增高,符合该诊断标准。急性缺氧可致肺动脉压升高,这一现象已经得到很多研究者证实,并称之为缺氧性肺动脉增压反应[4, 11-15];其原因是急性缺氧引起人体的肺动脉特别是肺小动脉收缩,肺循环阻力增加,引起肺动脉压的增高[16]。肺动脉压力的增高可使右室后负荷增加,即右心功能受损,从而导致RVOT和PAD增宽。以上理论与此次实验结果相符。
根据此次超声数据可知,到达高原后LVDd比平原时减小,提示左心前负荷减小,若是在左室心肌收缩能力不变的情况下,左室SV应该会降低。但此次实验结果是SV在急进高原前后差异不显著,左室EF增加。因此,可以推测出急性缺氧时在等长调节机制作用下,左室心肌收缩能力增强,即左心发挥了明显的代偿功能。多数研究也证实,低氧的直接影响表现为心脏功能特别是左室收缩功能保持不变或者轻度增高[6, 17]。查阅文献可知,左心发挥代偿功能的原因是:低氧作用于颈动脉体导致交感神经兴奋性提高,激动心肌细胞的β肾上腺素能受体后,可通过cAMP转导通路,激活细胞膜上的L型钙通道,增加钙离子内流,再通过钙触发钙释放机制促进心肌细胞胞质内钙离子浓度的增加。胞质内钙离子浓度增加后,活化的横桥数目增多促使心肌收缩能力增强[18]。
根据此次实验数据分析得知,在平原时,AMS组与non-AMS组相比PASP增高,CO与AMS评分具有负相关性,提示我们可在平原上运用超声心动图进行PASP检测及CO的检查并以此筛选AMS易感人群。在平原时PASP越高、CO越低的人越易感AMS。
[1] Yang T, Li X, Qin J, et al. High altitude-induced borderline pulmonary hypertension impaired cardiorespiratory fitness in healthy young men[J]. Int J Cardiol, 2015, 181:382-388.
[2] Chalkias A, Georgiou M, Böttiger B, et al. Recommendations for resuscitation after ascent to high altitude and in aircrafts[J]. Int J Cardiol, 2013, 167(5):1703-1711.
[3] 蔡秋瑾, 李筱玥, 张 欢, 等. 模拟急进高原过程对清醒和麻醉状态大鼠血压和呼吸的影响[J]. 中国病理生理杂志, 2015, 31(5):777-784.
[4] 高钰琪. 高原军事医学[M]. 第1版. 重庆:重庆出版社, 2005:5-54.
[5] Karinen HM, Peltonen JE, Kähönen M, et al. Prediction of acute mountain sickness by monitoring arterial oxygen saturation during ascent[J]. High Alt Med Biol, 2010, 11(4):325-332.
[6] Rao M, Li J, Qin J, et al. Left ventricular function during acute high-altitude exposure in a large group of healthy young chinese men[J]. PLoS One, 2015, 10(1):e116936.
[7] Tang E, Chen Y, Luo Y. Dexamethasone for the prevention of acute mountain sickness: systematic review and meta-analysis[J]. Int J Cardiol, 2014, 173(2):133-138.
[8] Chen GZ, Qin J, Yu J, et al. Incidence of acute mountain sickness in young adults at 3200 meters: comparison of the Lake Louise Scoring and Chinese Scoring Systems[J]. Genet Mol Res, 2013, 12(4):6790-6801.
[9] van Dijk AE, van Lien R, van Eijsden M, et al. Measu-ring cardiac autonomic nervous system (ANS) activity in children[J]. J Vis Exp, 2013(74):e50073.
[10] 刘庆军. 心脏彩色超声在冠心病左室舒张功能测定中的诊断价值[J]. 中国伤残医学, 2016, 24(1):99-100.
[11] Kizub IV, Strielkov IV, Shaifta Y, et al. Gap junctions support the sustained phase of hypoxic pulmonary vasoconstriction by facilitating calcium sensitization[J]. Cardiovasc Res, 2013, 99(3):404-411.
[12] Turner BE, Hodkinson PD, Timperley AC, et al. Pulmonary artery pressure response to simulated air travel in a hypobaric chamber[J]. Aerospace Med Human Perform, 2015, 86(6):529-534.
[13] Pagé M, Sauvé C, Serri K, et al. Echocardiographic assessment of cardiac performance in response to high altitude and development of subclinical pulmonary edema in healthy climbers[J]. Can J Cardiol, 2013, 29(10):1277-1284.
[14] Pavelescu A, Faoro V, Guenard H, et al. Pulmonary vascular reserve and exercise capacity at sea level and at high altitude[J]. High Alt Med Biol, 2013, 14(1):19-26.
[15] 崔 宇, 官立彬, 李晓栩, 等. 低氧促进Th17细胞浸润于肺组织并与肺血管改建相关[J]. 中国病理生理杂志, 2015, 31(2):250-255.
[16] Deuchar GA, Morecroft I, Dempsie Y, et al. Theinvivoeffects of human urotensin II in the rabbit and rat pulmonary circulation: effects of experimental pulmonary hypertension[J]. Eur J Pharmacol, 2006, 537(1-3):135-142.
[17] 朱永胜, 钱蕴秋, 孙 瑛, 等. 超声心动图观察急性高原反应和习服后心功能变化[J]. 西南国防医药, 2004, 14(5):492-494.
[18] Oikawa M, Wu M, Lim S, et al. Cyclic nucleotide phosphodiesterase 3A1 protects the heart against ischemia-reperfusion injury[J]. J Mol Cell Cardiol, 2013, 64:11-19.
Change of heart function and its relationship with AMS during acute high-altitude exposure at 3 658 m in Chongqing soldiers
YI Yuan-yue, LIU Bao, WU Gang, GAO Yu-qi
(InstituteofMedicineandHygienicEquipmentforHighAltitudeRegion,CollegeofHighAltitudeMilitaryMedicine,ThirdMilitaryMedicalUniversity;KeyLaboratoryofHighAltitudeEnvironmentalMedicine,MinistryofEducation;KeyLaboratoryofHighAltitudeMedicineofPLA,Chongqing400038,China.E-mail:gaoy66@yahoo.com)
AIM: To observe the cardiac function during high-altitude exposure in Chongqing soldiers and to discuss its relationship with acute mountain sickness (AMS) by echocardiography.METHODSThe changes of heart function were evaluated during acute high-altitude exposure (3 658 m, 3 d) in 42 healthy young male soldiers by echocardiography. At the same time, the heart rate, blood pressure, blood oxygen saturation, and the incidence of AMS after high-altitude exposure were observed and recorded.RESULTSThree days after arrival at 3 658 m, the left atrial end-systolic dimension (LADs), left ventricular end-diastolic dimension (LVDd) and right atrial end-systolic dimension were significantly decreased, but the right ventricular outflow tract diameter, pulmonary artery dimension, ejection fraction, cardiac output (CO), pulmonary arterial systolic pressure (PASP) and mean pulmonary arterial pressure were significantly increased compared with the baseline levels in all subjects. The mitral peak E velocity was significantly reduced (P<0.05). A total of 42 healthy young men were recruited and divided into AMS group with 15 subjects and non-AMS group with 27 subjects by Lake Louise scoring after high-altitude exposure. The cardiac function in the plain showed that aortic sinus diameter and LVDd in AMS group were significantly smaller, and PASP was significantly higher than those in non-AMS group. After high-altitude exposure, the LADs in AMS group was significantly smaller than that in non-AMS group (P<0.05). AMS scores and CO in the plain showed significant negative correlation (r=-0.3814,P<0.05).CONCLUSIONUpon acute high-altitude exposure, right ventricular functions of the young male soldiers are damaged with the compensation of the left ventricular functions. Using echocardiography to observe PASP and CO may be helpful for screening the susceptible people of AMS in the plain.
Acute mountain sickness; Left ventricle; Compensation; Echocardiography
1000- 4718(2017)12- 2233- 05
2017- 04- 26
2017- 09- 30
军队十二五重大课题(No. AWS14C007);第三军医大学高原医学特殊学科点项目(No. J1310001)
△通讯作者 Tel: 023-68752399; E-mail: gaoy66@yahoo.com
R363; R594.3
A
10.3969/j.issn.1000- 4718.2017.12.019
(责任编辑: 林白霜, 罗 森)