ACDF钢板内固定术治疗多节段颈椎病的疗效分析
陈志鹏 胡旭民 岑水忠 高梁斌
ACDF钢板内固定术治疗多节段颈椎病的疗效分析
陈志鹏 胡旭民#岑水忠 高梁斌*
目的探讨颈椎前路椎间盘切除植骨融合术(ACDF)钢板内固定术治疗三节段颈椎病的临床效果。方法回顾性分析2012年1月至2015年1月收治的于我院行ACDF钢板内固定术治疗的三节段颈椎病患者37例。比较术前,术后以及末次随访时的VAS评分、JOA评分、NDI指数评估治疗效果;比较术前,术后以及末次随访时颈椎Cobb's角(CA)、融合节段Cobb's角(SA)以及融合椎体高度评估患者的颈椎曲度及高度变化情况;记录手术时间、术中出血量;观察患者并发症的发生;通过末次随访时颈椎动力位片观察植骨后融合情况。结果随访时间为11~32个月,VAS评分:术前6.76±2.02分,术后3.24±1.53分,末次随访时3.0±0.9分。JOA评分:术前9.71±1.66分,术后13.26±2.14分,末次随访时15.97±16.79分。NDI评分:术前30.68±8.46分,术后6.68±3.85分,末次随访时4.14±1.27分。SA:术前8.65°±11.03°,术后18.65°±8.68°,末次随访时18.26°±8.59°。CA:术前12.35°±12.86°,术后21.45°±9.92°,末次随访时21.43°±9.97°。术后,末次随访上述随访指标与术前差异有统计学意义(P<0.05),末次随访时与术后的差异无统计学意义(P>0.05)。术椎高度:术前70.44±1.64mm,术后76.05±7.98mm,末次随访时70.83±4.71mm,术后术椎高度与术前差异有统计学意义(P<0.05),末次随访术椎高度与术前差异无统计学意义(P>0.05)。末次随访融合率为94.6%,发现1例患者出现神经根损伤;1例患者术后颈部血肿形成二次手术;3例患者出现术后吞咽困难但经治疗后改善;发现4例术后邻近节段退变,未发现内固定位置改变。结论ACDF钢板内固定术治疗三节段颈椎病疗效肯定,具有满意的临床治疗效果和较高的植骨融合率。
多节段颈椎病;减压术;骨折内固定术
多节段颈椎病(multi⁃level cervical spondylotic myelopathy,MCSM)是指影像学上存在连续或者不连续的三个及三个以上节段的颈椎体后缘骨赘形成以及椎间盘变性、突出等多种病理改变,造成颈髓以及硬膜囊的多个平面受压的退行性疾病[1],逐渐成为脊髓功能异常的最主要原因,病情严重者可致残,被视为一类严重威胁着广大患者健康生活的公共卫生问题。随着对此类疾病的深入探究,各类手术方式、方案也越发优化,临床效果越来越好[2],未来将有越来越多需要手术干预的病例。本文回顾性分析自2012年1月到2015年1月采用ACDF(anterior cervical discectomy and fusion)钢板内固定术的37例多节段颈椎病,对其治疗效果及并发症进行临床观察,探讨该种手术方式的有效性及安全性。
1 资料与方法
1.1 患者情况
中山大学孙逸仙纪念医院骨科,从2012年1月至2015年1月收治的37例多节段颈椎病,纳入标准为:①经CT和MRI确诊为颈椎病,颈椎间盘三个及三个以上节段突出,病变节段C3~T1;②合并有脊髓或神经根受压等临床症状和体征,自觉痛苦或日常生活动作发生障碍者;③非手术治疗3个月无效或复发;④坚持随访至少六个月。排除标准为:①C1~2或者C2~3椎间病变、颈椎外伤、先天性异常,肿瘤,或早期颈椎手术;②孕产妇、哺乳期妇女;③严重心血管疾病或肝肾功能不全者;④严重神经官能症和精神病者;⑤有其他可能影响本研究结果的疾病如骨质疏松症、风湿性关节炎、颈椎感染等疾病。
1.2 手术方法
气管内麻醉实施成功后取仰卧位,于后伸位固定头部,术野常规消毒、铺巾。
作左颈前纵向切口约8 cm,逐层切开皮肤、皮下组织,钝性分离颈阔肌,自胸锁乳突肌内侧在颈血管鞘和内脏鞘之间入路,直达颈前方。将气管、食管向一侧牵开,经C形臂影像增强器透视确定手术间隙;剥离椎前筋膜和前纵韧带,显露手术椎体前方,首先处理主要责任节段,用磨钻或椎板咬骨钳将椎体前缘骨赘,尖刀切开前缘纤维环,直视下取出病变的椎间盘。于减压椎间隙相邻的上下椎体置人椎体钉,以Caspar撑开器适度撑开椎间隙,至椎体周围软组织有一定张力,恢复至正常椎间隙的高度。以枪式咬骨钳小心去除椎体后缘骨赘及突入椎管内退变的椎间盘,两侧达钩椎关节,必要时切除增生肥厚的后纵韧带,减压至硬膜囊无明显受压。彻底减压后用刮匙刮除软骨终板至骨面渗血,注意保留椎间盘上下骨性终板的完整,取与椎间高度和形状一致的Cage试模置人椎间隙,大小松紧合适,取出试模,重新植入椎间融合器,松开Carspar撑开器;同样的方法处理余下的责任椎体。选择适合长度的预弯后的钢板固定于椎体前方,每个椎体用2枚单皮质螺钉固定,锁定螺钉锁紧钛板。经C形臂透视位置理想后,创面冲洗,放置引流,逐层缝合。复苏后,戴颈托返回病房。
1.3 术后治疗与随访
术后积极行康复锻炼,序贯无痛治疗。立即评价VAS评分、JOA评分以及NDI评分,影像学行X线、CT和MR检查。佩戴支具3个月,计划术后3个月行X线检查,之后若无不适则每半年返院复诊,每次复查评价VAS评分、JOA评分及NDI评分,行X线及CT检查。
1.4 术后评价与方法
①记录并比较术前、术后和末次随访时VAS评分、JOA评分以及NDI评分评估患者术后改善情况;②记录并比较术前、术后和末次随访时融合颈椎曲度以及椎体高度变化:颈椎Cobb's角(Cervical alignment,CA):C2以及C7椎体下终板延长线夹角;Cobb's角(Segmental Angle,SA):融合节段上位椎体上终板与下位椎体下终板的延长线夹角,前凸为正数,后凸为负数;颈椎高度以上位螺钉所固定的椎体的上缘至下位螺钉所固定椎体的下缘之间的距离,测量术前及术后不同时间的数据,颈前柱高度增加的百分数=(术后高度⁃术前高度)/术前高度*100%;③判断椎间植骨融合情况,采用Vaccaro等[3]的标准:融合器或植骨块与上下椎体间有明确的骨小梁通过;融合器周围不存在透亮带,伸屈位X线平片融合节棘突间无明显移位。④统计手术时间、出血量等数据;记录术后并发症发生情况。
1.5 数据分析与统计方法
统计指标是痛区VAS评分、JOA评分及NDI评分,骨性融合率、CA、SA、出血量、手术时间,以及并发症情况。采用SPSS 20.0统计软件,同组术前术后连续变量用配对t检验,并发症等多分类变量采用卡方检验;P<0.05为差异有统计学意义。
2 结果
符合入选标准的患者包括男20例,女17例,年龄32~76岁,平均57.6±10.1岁;病程8~25 d,平均15.11±4.87 d;累及C3~6的15例,累及C4~7的12例;手术时间175.2±47.1min,术中出血量47.6± 28.3mL。
术后一个月VAS评分同术前患者的VAS评分相比下降3.53±2.29分(P<0.01),末次随访VAS评分相比术后下降0.24±1.08(P>0.05)。术后一个月NDI评分同术前患者的NDI评分相比下降24±9.13分(P<0.01),末次随访NDI评分相比术后下降2.5± 4.20(P>0.05)。术后一个月JOA评分同术前患者的JOA评分相比增加3.55±2.42分(P<0.01),改善率为47.9%士3.20%,末次随访JOA评分同术后一个月患者的JOA评分相比增加0.47士1.27分;术后一周SA相比术前增加10.30士7.60(P<0.01),末次随访SA相比术后一周减少1.02士1.71(P>0.05);术后一周CA相比术前增加9.09士8.47(P<0.01),末次随访CA相比术后一周减少0.52士1.27(P>0.05)。术后高度相比术前增加5.61±5.03mm(P<0.01),较术前改善8.09%±6.64%。术后术椎高度与术前差异有统计学意义(P<0.05),末次随访术椎高度与术前差异无统计学意义(P>0.05)。末次随访融合率为94.6%,发现1例患者出现神经根损伤;1例患者术后颈部血肿形成二次手术;3例患者出现术后吞咽困难但经治疗后改善;发现4例术后邻近节段退变,未发现内固定位置改变。
表1 ACDF钢板内固定术治疗多节段颈椎病术后评价(±s)
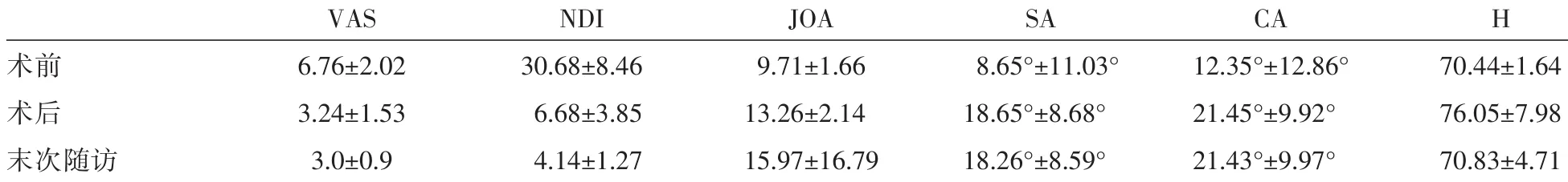
表1 ACDF钢板内固定术治疗多节段颈椎病术后评价(±s)
VASNDIJOASACAH术前6.76±2.0230.68±8.469.71±1.668.65°±11.03°12.35°±12.86°70.44±1.64术后3.24±1.536.68±3.8513.26±2.1418.65°±8.68°21.45°±9.92°76.05±7.98末次随访3.0±0.94.14±1.2715.97±16.7918.26°±8.59°21.43°±9.97°70.83±4.71
3 讨论
多节段颈椎病是颈椎三个或三个以上节段退变及其继发性改变刺激或压迫脊髓[1],引起各种症状或体征的常见病[4],常合并颈椎节段不稳、颈椎生理曲度变直、后纵韧带增厚或者钙化,严重地影响着患者的身体健康和生活质量[5]。对于症状较轻的患者,保守治疗,包括制动、佩戴颈托或者牵引[6],往往可有效缓解症状。但是保守治疗仅仅对轻度颈椎病有效且效果因人而异[7,8]。对于中重度、保守治疗无效的颈椎病,尤其是脊髓型颈椎病,手术治疗是唯一的选择[9,10]。
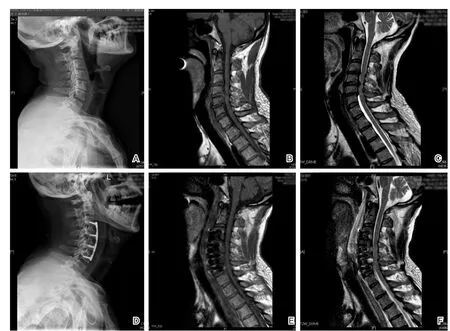
图1 男性患者,57岁,C3~C6脊髓型颈椎病,行C3⁃6椎间盘切除减压,cage融合钢板内固定术A术前颈椎侧位X线片示颈椎稍后凸,C3⁃6椎间隙狭窄;B、C术前颈椎矢状位MRl T1W1、T2W1示C3⁃6椎间盘突出压迫脊髓,颈椎前凸消失;D术后颈椎侧位X线片示C3⁃6三节段cage融合钢板内固定,颈椎前凸存在;E、F术后颈椎矢状位MRIT1W 1、T2WI示脊髓减压彻底,颈椎前凸存在
文献报道[11⁃13],对于三节段颈椎退行性病变,当脊髓压迫来自前方,前路可直接彻底减压,尤其是当颈椎生理曲度变直甚至呈后凸畸形时,可维持正常的椎间高度和生理曲度。得益于脊髓神经的减压和脊柱的稳定与脊柱序列的维持,自从50年代由Smith[14]及Cloward[15]报道应用于颈椎病的治疗以来,ACDF钢板内固定术被广泛用于治疗多节段颈椎病[16],并取得不错的临床效果。本组随访结果表明,ACDF钢板内固定术手术时间短,术中出血量少,并且能明显改善脊髓神经功能,术后评分明显增加,平均改善率较高。颈椎生理曲度及融合椎体高度较术前有明显恢复,末次随访时椎间融合率较高,颈椎稳定性好,无钢板松动、螺钉折断等并发症发生,疗效满意。得益于椎间融合器cage[17]以及椎前钢板的应用,ACDF钢板内固定术被认为是多节段颈椎手术最好的手术方式。过去,自体骨是最常用的支撑融合材料,但是自体取骨并发症较多,影响患者的术后恢复,并且随访过程中出现较高的沉降率。相比自体骨,颈椎融合器的承载负荷能力明显增高,与终板形态有较好的吻合度,可减少发生塌陷、吸收的风险,术后颈椎曲度得到明显改善可促进植骨融合,被认为是自体骨良好的替代物[18],广泛应用于ACDF术中。辅以前路钢板明显可以提高其融合率:生物力学研究表明,钢板可减少Cage与椎体终板之间的移动,增加手术节段的稳定性,同时起到应力分担的作用,融合器上下界面仍然能承受足够的压应力,从而增加融合的概率。研究表明双节段和多节段ACDF钢板内固定术的融合率为70%~100%。与单节段ACDF钢板内固定术融合率相似。有学者认为,前路钢板固定可加速邻近节段退变疾病,韩国Ulsan医科大学的Lee等[19]证实颈前路邻近节段骨化形成被认为是一种异位骨化,钢板与椎间隙的距离是邻近节段骨化形成的关键因素。因此在颈椎前路手术中应用适当的的钢板来降低邻近节段骨化形成。在前路钢板的规范化cage和钛板的共同作用,解决了长节段融合术后假关节发生率较高的难题[20]。
颈椎曲度以及高度与融合术后的生活质量以及术后脊髓病症状恢复密切相关,椎间高度降低和颈椎生理前凸丢失会造成椎管容积变小,可致脊髓内张力增高、脊髓或神经根受压。研究证明,当椎间盘高度减少1mm时,相应椎间孔面积减少20%~30%;在椎间盘高度减少2 mm、3 mm时,相应椎间孔面积则分别减少30%~40%、35%~45%:超过3mm的椎间盘高度丢失会出现严重的神经根压迫症状。Kawatam等[21]及Goto等[22,23]认为融合节段曲度不良易造成临近节段退变,颈椎生理曲度的恢复防止神经症状恶化的重要因素之一[24],已经成为除植骨融合率以外的新标准。因此,重建及维持颈椎生理曲度以及高度对维持颈椎的远期稳定性及恢复颈椎本身的生物力学环境有重要意义。ACDF钢板内固定术通过椎间盘切除、撑开病变椎间隙,既扩大了椎间孔的大小,又恢复了周围软组织的张应力,在重建颈椎生理曲度、高度方面更有优势[25⁃27],当恢复的颈前柱高度恰当时,由于病变节段后纵韧带在植入骨和内固定支撑的纵向力作用下向椎体内收,椎管扩大,达到减压目的。临床及影像学数据提示本组37例患者颈椎生理曲度、高度较手术前相比有明显的恢复,这与既往研究结果相符[26,28]。因此我们认为ACDF钢板内固定术是重建及维持颈椎生理曲度、高度的有效办法。
经过半个世纪的发展ACDF钢板内固定术的临床效果已得到巨大的提升,然而,涉及多节段的颈椎病手术治疗与不太可预测的结果和较高的并发症发生频率有关[29],如假关节形成、临近椎体退变、吞咽困难以及颈椎内固定物相关的并发症包括内固定物的移位、断裂等[30]。Fountas等[31]对1015例实施ACDF钢板内固定术的患者曾经进行过统计,其中吞咽困难发生率9.5%、皮下血肿5.6%、喉返神经麻痹3.1%、食道破裂0.3%、术后Horner综合征0.1%、内置物取出0.1%、浅部感染0.1%。在本次回顾性分析37例手术患者中本组病例无死亡,未发生食道瘘、感染和神经症状加重等并发症。发现1例患者出现神经根损伤,术后予营养神经、康复锻炼后好转;1例患者术后颈部血肿形成二次手术治疗后均好转,未出现脊髓损伤、死亡等严重并发症。3例患者出现术后吞咽困难但经治疗后改善;发现4例术后邻近节段明显退变,未发现假关节形成及内固定位置改变。并发症发生率与同类型研究相近。1999年,Matsunaga等[32]报道,多节段融合1年后,邻近节段剪力增加20%。因此,多节段融合术后临近节段退变是常见并发症,总体而言,颈椎融合后,邻近节段退变可高达92%。椎前钢板被认为是相邻节段退变的危险因素,Park等[33]认为钢板末端距离相邻椎间盘小于5mm可大大提高相邻椎体退变的概率。因此在手术过程中需要手术医生注意选择适当的钢板长度。
总之,ACDF钢板内固定术具有较好的临床疗效评价,虽然可引起术后吞咽困难等并发症,但是只要适应症选择得当,手术技巧娴熟,术后护理到位,不失为一种安全有效的手术方式,对颈椎曲度的重建与维持产生一定的正面影响。本研究的不足之处为回顾性研究,而非随机对照以及前瞻性研究。患者总病例数为37例,病例数相对偏少,且随访时间为11~32个月,对于此种手术的中远期疗效未做研究。
[1]贾连顺.颈椎病的现代概念[J].脊柱外科杂志,2004,2(2):123-126.
[2]Reitman CA,Hipp JA,Nguyen L,et al.Changes in segmental intervertebral motion adjacent to cervical arthrodesis:a prospective study[J].Spine(Phila Pa 1976),2004,29(11):E221-E226.
[3]Vaccaro AR,Carrino JA,Venger BH,et al.Use of a bioabsorbable anterior cervical plate in the treatment of cervical degenerative and traumatic disc disruption[J].J Neurosurg,2002,97(4 Suppl):473-480.
[4]FehlingsMG,Wilson JR,Kopjar B,etal.Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy results of the AOSpine North America Prospective multi⁃center study[J].JBone Joint Surg Am,2013,95A(18):1651-1658.
[5]Irvine DH,Foster JB,Newell DJ,et al.Prevalence of cervical spondylosis in a general practice[J].Lancet(London,England),1965,1(7395):1089-1092.
[6]Parikh CK.Management of cervical spondylosis with a new appliance—vissco cervical traction kit[J].Indian med J,1964,58:25-27.
[7]Rhee JM,Sham ji MF,Erwin WM,et al.Nonoperative management of cervical myelopathy a systematic review[J]. Spine,2013,381(22):S55-S67.
[8]Ghobrial GM,Harrop JS.Surgery vs conservative care for cervical spondylotic myelopathy:nonoperative operative management[J].Neurosurgery,2015,62(Suppl1):62-65.
[9]Fehlings MG,Wilson JR,Yoon ST,et al.Symptomatic progression of cervicalmyelopathy and the role of nonsurgical management a consensus statement[J].Spine,2013,381(22):S19-S20.
[10]Ghogawala Z,Benzel EC,Riew KD,et al.Surgery vs conservative care for cervical spondyloticmyelopathy:surgery is appropriate for progressive myelopathy[J].Neurosurgery,2015,62(Suppl1):56-61.
[11]Zhu B,Xu Y,Liu X,et al.Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy:a systemic review and meta-analysis[J].Eur Spine J,2013,22(7):1583-1593.
[12]Liu X,Wang H,Zhou Z,et al.Anterior decompression and fusion versus posterior laminoplasty for multilevel cervical compressive myelopathy[J].Orthopedics,2014,37(2):E117-E122.
[13]Sun Y,Li L,Zhao J,Gu R.Comparison between anterior approaches and posterior approaches for the treatment of multilevel cervical spondylotic myelopathy:A meta-analysis[J].Clin NeurolNeurosurg,2015,134:28-36.
[14]Smith GW,Robinson R A.The treatment of certain cervicalspine disorders by anterior removal of the intervertebral disc and interbody fusion[J].JBone Joint Surg Am,1958,40-A(3):607-624.
[15]Cloward RB.Cervical diskography;technique,indications and use in diagnosis of ruptured cervical disks[J].Am J RoentgenolRadium Ther NuclMed,1958,79(4):563-574.
[16]Zhu B,Xu Y,Liu X,et al.Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy:a systemic review and meta⁃analysis[J]. European Spine J,2013,22(7):1583-1593.
[17]Faber E,Bohler J.The adjustment of hearing aids in luxembourg.study carried out according to data gathered in the audiometry center from 1958 to 1963[J].Bulletin de la Societe des sciencesmedicales du Grand⁃Duche de Luxembourg,1964,101:21-30.
[18]张蒲,李华,李慧武,等.聚醚醚酮融合器与自体髂骨块植骨在颈椎融合术中的对照研究[J].脊柱外科杂志,2007,5(4):198-201.
[19]Lee DH,Lee JS,Yi JS,et al.Anterior cervical plating technique to prevent adjacent⁃level ossification development[J].Spine J,2013,13(7):823-829.
[20]杨有庚,刘钦毅,白云深.多节段颈椎间盘突出症的外科治疗[J].中国脊柱脊髓杂志,2003,13(7):424-426.
[21]Epstein NE.Laminectomy with posterior wiring and fusion for cervical ossification of the posterior longitudinal ligament,spondylosis,ossification of the yellow ligament,stenosis,and instability:a study of 5 patients[J].JSpinal Disord,1999,12(6):461-466.
[22]Goto S,Mochizuki M,Kita T,et al.Anterior surgery in four consecutive technical phases for cervical spondyloticmyelopathy[J].Spine,1993,18(14):1968-1973.
[23]Goto S,Kita T.Long⁃term follow⁃up evaluation of surgery for ossification of the posterior longitudinal ligament[J].Spine,1995,20(20):2247-2256.
[24]Scheer JK,Tang JA,Smith JS,etal.Cervical spine alignment,sagittal deformity,and clinical implications A review[J].J Neurosurg Spine,2013,19(2):141-159.
[25]Albert TJ,Vacarro A.Postlaminectomy kyphosis[J].Spine(Phila Pa 1976),1998,23(24):2738-2745.
[26]KawakamiM,Tamaki T,IwasakiH,etal.A comparative study of surgical approaches for cervical compressivemyelopathy[J]. Clin Orthop RelatRes,2000,381:129-136.
[27]Uchida K,Nakajima H,Sato R,et al.Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment:outcome after anterior or posterior decompression[J].JNeurosurg Spine,2009,11(5):521-528.
[28]Edwards CN,Heller JG,Murakami H.Corpectomy versus laminoplasty formultilevel cervicalmyelopathy:an independent matched⁃cohortanalysis[J].Spine(Phila Pa 1976),2002,27(11):1168-1175.
[29]Danto J,Dicapua J,Nardi D,et al.Multiple cervical levels:increased risk of dysphagia and dysphonia during anterior cervical discectomy[J].J Neurosurg Anesthesiol,2012,24(4):350-355.
[30]Tetreault L,Ibrahim A,Cote P,et al.A systematic review of clinical and surgical predictors of complications following surgery for degenerative cervicalmyelopathy[J].J Neurosurg Spine,2016,24(1):77-99.
[31]Fountas KN,Kapsalaki EZ,Nikolakakos LG,et al.Anterior cervical discectomy and fusion associated complications[J]. Spine,2007,32(21):2310-2317.
[32]Matsunaga S,Kabayama S,Yamamoto T,et al.Strain on intervertebral discs after anterior cervical decompression and fusion[J].Spine(Phila Pa1976),1999,24(7):670-675.
[33]Park JB,Cho YS,Riew KD.Development of adjacent⁃level ossification in patients with an anterior cervical plate[J].J Bone JointSurg Am,2005,87(3):558-563.
Study on conventional cage p late internal fixation in treating multi⁃level cervical spondylotic myelopathy
CHEN Zhipeng,HU Xumin#,CEN Shuizhong,GAO Liangbin.
Orthopaedic Department,Sun Yet⁃sen Memorial Hospital,Sun Yat⁃sen University,Guangzhou 510120,China.Corresponding author:Gao Liangbin,gaoliangbin@yeah.net #co⁃firstauthors
Objective To discuss the clinical outcome of anterior cervical discectomy and fusion(ACDF)with internal fixation in treating multi⁃level cervical spondylotic myelopathy.M ethods Thirty⁃seven cases suffer from multi⁃level cervical spondylotic myelopathy were treated with anterior cervical decompression and fusion with internal fixation by titanium plate in our hospital from Jan.2012 to Jan.2015.The clinical outcomeswere evaluated by the parameters including improvement of Japanese Orthopaedic Association(JOA)score and neck disability index values(NDI)before operation,one months after operation and at the last follow up,measured cervical Cobb Angle(CA)and Segmental Angle(SA)on X⁃ray film.Record operation time,intraoperative blood loss,and the incidence ofcomplications.Bony fusion was verified by X⁃ray at the final follow⁃up.Results The patients were followed up for 11 to 30months.VAS scoreswere decreased from 6.76±2.02 preoperatively to 3.24±1.53 postoperation and 3.0±0.9 at the final follow⁃up.JOA scores were increased from 9.71±1.66 preoperatively to 13.26±2.14 postoperation and 15.97±16.79 at the final follow⁃up.NDI scores were decreased from 30.68±8.46 preoperatively to 6.68±3.85 postoperation and 4.14±1.27 at the final follow up.SA were increased from 8.65°±11.03°preoperatively to 18.65°±8.68°postoperation and 18.26°±8.59° at the final follow up.CA were increased from 12.35°±12.86°preoperatively to 21.45°±9.92° postoperation and 21.43°±9.97°at the final follow up.There were significant improvement for all postoperatively and at the final follow up compared with those preoperatively.There were no significant difference between postoperation and at final follow up for all.Heightwere increased from 70.44±1.64 mm preoperatively to 76.05±7.98mm postoperation and 76.05±7.98mm at the final follow up.Therewas significant improvement for postoperatively compared with that preoperatively.There were no significant difference between that at final follow up and preoperatively.Bony fusion rate was 94.6%,and one case complicated with nerve root injury,one case had a secondary surgery because of cervical haematoma,three had dysphagia after surgery but was improved after treatment,four cases had adjacent segment degeneration.No complications of internal fixation was found.Conclusion The clinical outcomes of anterior cervical decompression and fusion with internal fixation in treating MCSM is affirmative,and it makes spinal canal decompression and neurologic symptoms ease and fusion rate increase.
multi⁃level cervical spondyloticmyelopathy;decompression;fracture fixation
R681.5
A
10.3969/j.issn.1009⁃976X.2017.04.021
2017-06-15)
卫生部医药卫生科技发展研究中心项目(W2013ZT081)
510120广州中山大学孙逸仙纪念医院骨科
*通讯作者:高梁斌,Email:gaoliangbin@yeah.net
#共同第一作者