先天性双主动脉弓畸形的诊断与外科治疗
刘彩霞,马新平,杨 辉,陈 瑞
(山西省儿童医院,山西 太原 030013)
·临床医学·
先天性双主动脉弓畸形的诊断与外科治疗
刘彩霞,马新平,杨 辉,陈 瑞
(山西省儿童医院,山西 太原 030013)
目的:总结婴幼儿先天性双主动脉弓畸形的诊断与手术治疗经验,分析漏误诊的原因,以进一步提高该疾病的诊治效果。方法:对7例先天性双主动脉弓畸形的诊断过程及外科治疗进行回顾性分析和总结研究。结果:全组7例中伴有咳喘或气促等呼吸系统症状的有6例,进食固体食物困难的1例。合并心内畸形的1例,合并肺动脉吊带畸形的1例,单纯性双主动脉弓畸形5例。超声确诊1例,发现主动脉弓畸形可疑建议CT检查的2例,发现肺动脉走形异常建议CT检查发现同时合并双主动脉弓畸形的1例,漏诊3例。7例均经心脏大血管螺旋CT及三维重建检查确诊。7例中于不同医院就诊3次以上才得以确诊的有6例。7例中6例行手术矫治,其中正中开胸手术2例,后外侧开胸手术4例,无围术期死亡。1例合并肺动脉吊带的患儿因并发“环-吊带复合体”畸形术后脱离呼吸机困难家长放弃治疗。术后出院时4例患儿无残余症状,1例哭闹后有轻微残余呼吸道症状。随访发现该患儿呼吸道症状半年后消失。无需再手术病例。另1例未手术者仍在随访中。结论:对于反复呼吸道感染、咳喘或吞咽困难的患儿,儿科及影像科医生应注意除外双主动脉弓畸形,避免误诊误治;螺旋CT增强扫描和三维重建是诊断双主动脉弓畸形的可靠方法。单纯双主动脉弓畸形手术效果良好。
双主动脉弓;先天性;血管环;反复呼吸道感染;气管压迫
先天性双主动脉弓(Double Aortic Arch,DAA)是较罕见的先天性血管畸形,由于主动脉弓及其分支发育异常造成左、右侧主动脉弓并存形成一血管环环绕气管和食管并对其造成压迫导致呼吸道或消化道症状。关于该畸形的报道较少,2009年9月~2016年6月山西省儿童医院诊治7例婴幼儿先天性双主动脉弓畸形(见图1),现将诊治体会总结报告如下。
1 资料与方法
1.1 一般资料
本组男4例,女3例,年龄5月~4岁7月,平均(18.3±6.8)月,体重5.6~16.5Kg,平均(11.2±2.8)kg。伴有咳喘或气促等呼吸系统症状的有6例,1例进食固体食物时经常出现气促、青紫,甚至呼吸窘迫,而且症状逐渐加重。7例患儿均在安静状态下应用Philip iE33和iE Elite彩色多普勒超声诊断仪,经胸探头S5-1、S8-3、S12-4、X7-2行常规心脏超声心动图检查。伴有消化道症状的1例患儿行上消化道钡剂造影检查。所有患儿均经螺旋增强CT检查确诊,采用Philip Brilliance16排螺旋CT(multislice computed tomography,MSCT),扫描层厚3 mm,管电压120 kV、管电流100 mA,对比剂采用碘海醇(300 mg/mL),剂量1.5~3mL/kg,注射速度0.5~3.5 mL/s,延迟扫描时间为15~20s。不配合的患儿需要在检查前镇静。7例中单纯性双主动脉弓畸形5例,合并心内畸形室间隔缺损1例,合并肺动脉吊带畸形1例,该例患儿同期作了电子纤维支气管镜检查发现同时并发“环-吊带复合体”畸形。
1.2 研究方法
1.2.1 追踪确诊过程 对7例患儿的临床症状、体征、确诊前到医院就诊的次数、确诊前的诊断、初次就诊到确诊所经历的时间分别进行了追踪统计和分析。
1.2.2 手术方法 手术前请麻醉师分别留置上、下肢动脉测压管和上、下肢血氧饱和度检测。单纯性双主动脉弓手术在常温非体外循环下进行,经胸部后外侧切口第四肋间入胸,切开纵膈胸膜,充分游离发育不良的非优势弓,先在非优势弓汇入降主动脉处试行阻断,观察上、下肢血压及氧饱和度无变化后将其阻断、切断缝合。同时结扎并切断动脉导管或动脉韧带,并松解气管、食管周围组织,彻底解除对气管、食管的压迫。术中同时注意保护喉返神经和膈神经。
合并室间隔缺损和肺动脉吊带的患儿采用正中开胸,中低温体外循环下行手术矫治(见图2,3)。
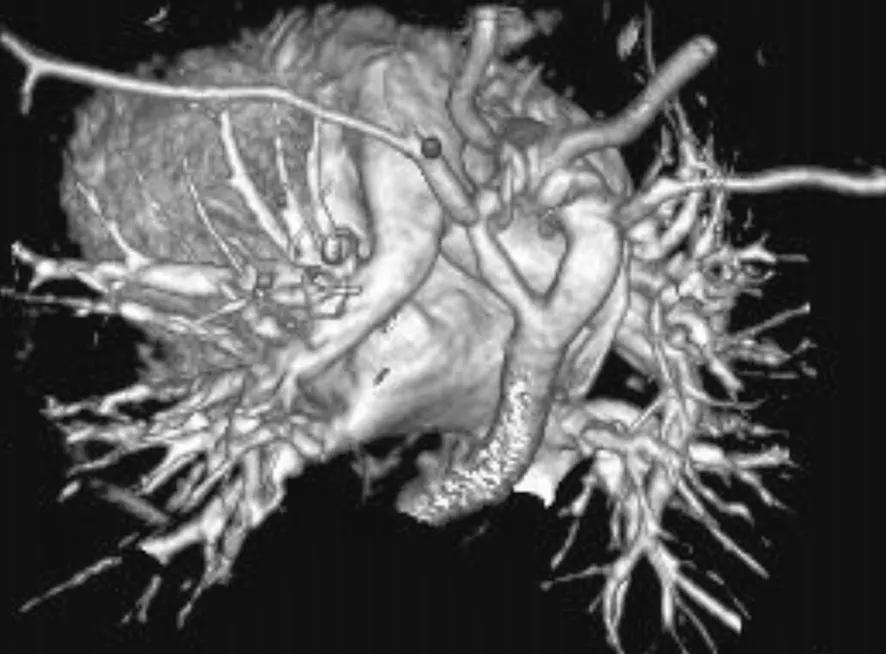
图1 双主动脉弓畸形的螺旋CT三维重建影像,升主动脉先分为左(前)弓和右(后)弓,两弓再汇合形成降主动脉。Fig.1 Spiral CT Three -dimensional Reformatted Image of Congenital Abnormality of Double Aortic Arch

图2 经胸骨正中切口手术中显示升主动脉分为左弓和右弓Fig.2 Ascending Aorta Combined with Left Arch and Right Arch Showed through the Mid-sternal Incision Operation

图3 双主动脉弓手术切断次弓(左前弓)后复查的CT影像Fig.3 CT Image of Check for Division of Left Anterior Aortic Arch through Double Aortic Arch
2 结果
本组患儿曾先后在多家医院以支气管肺炎、喘息性支气管炎、喉气管支气管炎、喉软管发育不良或气管异物,甚至支气管哮喘诊治,7例中于不同医院就诊3~4次以上才得以确诊的有6例(86%,6/7)。本组病例中心脏超声确诊1例(14%,1/7),发现主动脉弓畸形可疑建议CT检查的2例(29%,2/7),发现肺动脉走形异常建议CT检查发现同时合并双主动脉弓畸形的1例,漏诊3例(43%,3/7)。7例均经心脏大血管螺旋CT及三维重建检查确诊。7例中6例行手术矫治,其中正中开胸手术2例,后外侧开胸手术4例,无围术期死亡。术后呼吸机辅助5~68 h,平均(12.3±4.8)h。1例合并肺动脉吊带畸形的患儿因并发“环-吊带复合体”畸形术后脱离呼吸机困难家长放弃治疗。术后出院时4例无残余症状,1例哭闹后有轻微残余呼吸道症状。随访发现该患儿呼吸道症状半年后消失。无需再手术病例,也无主动脉弓梗阻征象。另1例未手术患儿仍在随访中,建议尽早手术。
3 讨论
若胚胎发育时期左右第四弓均持续存在则形成双主动脉弓畸形。双主动脉弓是完全性血管环畸形的一种[1],双弓均起源于升主动脉,在气管和食管两侧通过,然后结合形成降主动脉,形成完全性血管环,气管和食管被双弓环绕和压迫,有的会出现严重的呼吸道和食道压迫症状。
1737年Hommel首先报道了双主动脉弓的病例。1939年Wolman描述了一例双主动脉弓病例伴有气管和食管压迫综合症[2]。直到1945年Gross首次对一例双主动脉弓病例进行外科手术并获得成功[3]。
双主动脉弓畸形的临床表现与气管、食管受压程度密切相关,症状一般出现在6个月内,重者1个月甚至出生时即有吸气喘鸣表现。严重者甚至发生呼吸暂停、发绀、意识不清。反复呼吸道感染也是较为常见的症状。气道梗阻不太严重的患儿,以上表现常间歇出现。如果存在食管压迫,主要表现为喂养、吞咽困难[4],甚至在进食时因压迫气管而发生气道梗阻出现休克,这在进固体食物时尤为明显。本组中有1例即是因严重喂养困难,进食时经常青紫,甚至休克就诊发现的。因其临床表现易与一些内科呼吸道疾病相混淆,本组7例中有6例(86%,6/7)先后于不同医院就诊三次以上才得以确诊。Krzystolik Ladzinska报道[5]因症状相似一男孩一直被误诊为支气管哮喘进行治疗,直到15岁时才确诊为双主动脉弓畸形。因此在诊疗中遇到反复咳喘、喉鸣、呼吸困难、呼吸道感染迁延不愈或喂养困难者要想到本病,早诊断早治疗,避免误诊误治,延误最佳治疗时机[6]。
诊断方面,从本组病例的影像检查来看,多层螺旋CT同时行三维重建是诊断双主动脉弓畸形的有效手段,弥补了超声心动图对心外畸形诊断的不足,而且可以直观显示左、右弓的大小形态,有助于区别主、次弓,对手术方案的拟定意义重大。但是超声心动图检查对于该畸形的诊断没有优势,容易造成误诊和漏诊。本组7例漏诊3例(43%,3/7)。
所有的双主动脉弓畸形都有手术指征[7],早期正确手术极为重要,延迟治疗可能会造成猝死。本研究手术经验与文献报道相同,只要不伴有心内畸形,不论左弓、右弓为主弓均选择经降主动脉侧的胸部切口矫治,而且术前要分别放置上、下肢动脉测压管和血氧饱和度监测,术中离断次弓前要先试行阻断,观察数分钟,上、下肢血压和血氧饱和度无明显变化方可离断。
手术中彻底解除异常双主动脉弓的环绕,并充分松解气管、食管周围粘连的组织,并保持纵膈胸膜开放避免远期粘连[8],对于单纯双主动脉弓畸形都能取得满意的手术疗效。本组患儿出院时4例无残余症状,1例哭闹后仍有轻微喘息和喉鸣症状。随访发现该患儿呼吸道症状半年后消失。无需再手术病例,也无主动脉弓梗阻征象。另1例未手术者仍在随访中。Khalfan Alsenaidi等[9]对81例双主动脉弓手术患者进行了随访,认为手术结果良好,死亡率低。有部分患者远期持续存在呼吸道症状,但考虑可能与先前压迫所致的气管软化和大气道发育不良有关,但均无需外科处理。有学者认为合并气管软化的患者呼吸道症状可能会持续数月,但随着时间推移,都能长期缓解。近年来提倡采用微创胸腔镜技术(VATS)治疗血管环[10]。Koontz等[11]认为VATS对双主动脉弓伴左弓闭锁安全、有效。
[1] Backer CL, Mavroudis C: Congenital Heart Surgery Nomenclature and Database Project:vascular rings, tracheal stenosis, pectus excavatum[J]. Ann Thorac Surg, 2000,69(4):S308-318.
[2] Wolman IJ. Syndrome of Constricting Double Aortic Arch in Infancy: report of a case[J]. J Pediatr, 1939,14:527-533.
[3] Gross RE. Surgical Relief for Tracheal Obstruction from a Vascular Ring[J]. N Engl J Med, 1945,233:586-590.
[4] Kondo C, Takabayashi S, Miyake Y, et al. Successful Surgical Treatment for an Adult Case of Double Aortic Arch[J]. Jpn J Thorac Cardiovasc Surg, 2005,53(4):223-226.
[5] Krzystolik adzińska J, Goc B, Rokicki W, et al. Undiagnosed Double Aortic Arch Causing Respiratory Disturbances after 15-years[J]. Pneumonol Alergol Pol, 2001,69(1-2):97-101.
[6] Ullmann N,Menchini L,Salerno T,et al. Late Diagnosis of Double Sortic Arch: consequences on long-term follow-up[J]. Pediatr Pulmonol,2014,49(3):75-77.
[7] Van son JA, Julsrud PR, Hagler DJ, et al: Surgical Treatment of Vascular rRings: the mayo clinic experience[J]. Mayo Clin Proc, 1993,68(11): 1056-1063.
[8] Backer CL,Mongé MC,Russell HM,et al. Reoperation after Vascular Ring Repair[J]. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu,2014,17(1):48-55.
[9] Khalfan Alsenaidi, Rebecca Gurofskya, Tara Karamlou, William G. Williams, Brian W. McCrindle. Management and Outcomes of Double Aortic Arch 81 Patients[J]. Pediatrics, 2006,118(5):1336-1341.
[10] Al-Bassam A, Saquib Mallick M, Al-Qahtani A, et al. Thoracoscopic Division of Vascular Rings in Infants and Children[J]. J Pediatr Surg, 2007,42(8):1357-1361.
[11] Koontz CS, Bhatia A, Forbess J. Video-assisted Thoracoscopic Division of Vascular Rings in Pediatric Patients[J]. Am Surg, 2005,71(4):289-291.
本文编辑:王 霞
Diagnosis and Surgical Treatment of Congenital Abnormality of Double Aortic Arch
LIU Caixia,MA Xinping,YANG Hui,CHEN Rui
(ShanxiChildren'sHospital,Taiyuan030013,Shanxi,China)
Objective: To summarize the diagnostic methods and surgical experience of congenital abnormality of double aortic arch and to analyze the causes of missed diagnosis and misdiagnosis in infants for the sake of curtive effects. Methods:7 cases of diagnostic process and the surgical treatment experience for the patients with double aortic arch diagnosed between September 2009 and June 2016 in Shanxi Children's Hospital were studied retrospectively.Results:6 cases in the group had respiratory symptoms such as cough, stridor, or shortness of breath. One case had difficulty in taking solid food,with one case combined with intracardiac anomalies. One case was showed pulmonary artery sling as well. 5 cases were only with double aortic arch. One case with double aortic arch was diagnosed definitely by echocardiography. Two cases suggested for CT scan were doubted with aortic anomalies by echocardiography. Double aortic arch was also found by CT except for pulmonary artery sling in one case who was found with pulmonary artery anomaly by echocardiography. 3 cases of double aortic arch were missed. Diagnoses of the above 7 cases were all confirmed by spiral CT scan. In the group,6 cases had definite diagnoses after visiting doctor for 3 times or more in different hospitals. Six cases were undergone surgical treatment and no perioperative death. Two cases were through mid-sternal incision and 4 ones through posterolateral thoracotomy. One case with pulmonary artery sling had difficulty in being extubated postoperatively, so his parents initiated discontinued treatment. At discharge 4 cases were asymptomatic after half a year and one had mild residual respiratory symptom after crying. During follow-up the symptom in this case disappeared. No one needed reoperations. The one with no procedure was still in follow-up.Conclusions:Pediatricians and imaging doctors should pay more attention and exclude double aortic arch in the patients with recurrent respiratory infection or cough and stridor. Enhanced CT scanning and three-dimensional reconstruction are reliable diagnostic methods to double aortic arch. Surgical treatment is effective for cases with simple double aortic arch.
double aortic arch;congenital abnormality;vascular ring;recurrent respiratory infection;tracheal compression
山西省儿童医院资助项目(201028)
刘彩霞,女,副主任医师,从事小儿心胸外科临床工作
R725.4
A
1671-0126(2017)02-0004-04