白内障患者术后联用激素和非甾体抗炎药的临床效果考察
刘晖,刘刚,罗莉丽
(四川省内江市第一人民医院眼科,四川 内江 641000)
白内障患者术后联用激素和非甾体抗炎药的临床效果考察
刘晖,刘刚,罗莉丽
(四川省内江市第一人民医院眼科,四川 内江 641000)
目的 研究白内障患者术后应用激素联合非甾体抗炎药治疗的临床效果。方法将200例白内障患者随机分为观察组(妥布霉素地塞米松+普拉洛芬)和对照组(妥布霉素地塞米松),每组100例,观察记录患者围治疗期的各项症状和体征的评分及综合评分。结果观察组黄斑囊样水肿发生率和前房闪辉评分明显小于对照组,差异有统计学意义(P<0.05),尽管观察组患者的眼压评分小于对照组,差异无统计学意义;此外在术后4 d和7 d时[(7.1±0.8)vs(8.3±0.9),(5.2±0.9)vs(6.6±0.7)],观察组综合评分显著低于对照组,差异具有统计学意义(P<0.05),而在术后14 d和30 d时[(3.2±0.7)vs(3.3±0.8),(1.1±0.5)vs(1.1±0.6)],差异无统计学意义。结论白内障患者术后联用妥布霉素地塞米松和普拉洛芬可以有效地起到早期抗炎和缓解术后不良反应的作用,具有良好的临床应用价值。
白内障;激素类药物;非甾体抗炎药
白内障在眼科治疗中普遍使用的手术疗法是超声乳化联合人工晶体植入术,但是该疗法在治疗过程中较易使前房发生不同程度的炎症反应[1]。现阶段白内障患者术后抗炎的主要方法即为在患处进行糖皮质激素和非甾体抗炎药的联合给药疗法[2],但是对于部分炎症反应较轻的患者能否进行非激素类药物给药治疗还有待于进一步研究[3]。本文选取200例白内障患者进行了短期的糖皮质激素和非甾体类抗炎药联合给药,现将结果报道如下。
1 资料与方法
1.1 临床资料 选取2015年1月~2016年6月在四川省内江市第一人民医院接受白内障超声乳化联合人工晶体植入术治疗的200例白内障患者为治疗对象,按随机数字表将其分为对照组和观察组,每组100例,对照组中有男71例,女29例,年龄51~85岁,平均(68.16±9.75)岁;观察组中有男64例,女36例,年龄50~89岁,平均(71.35±8.69)岁。两组临床资料差异无统计学意义。所有治疗对象的准入标准为[4]:(1)年龄相关性白内障患者;(2)眼压在2.80 kPa以下;(3)诊断未见其他眼科前后节疾病;(4)无糖尿病病史;(5)无眼科手术病史;(6)术中未见并发症;(7)签署知情同意书。
1.2 方法 所有患者均由同一组医护人员进行同等的白内障标准超声乳化联合人工晶体植入术进行治疗[5],其术后的总疗程均为1个月。其中对照组进行常规白内障术后给药治疗:即妥布霉素地塞米松滴眼液,6次/d,连续滴眼4 d,其后改为每天给药3次;观察组在进行上述常规给药的基础上,同时联用非甾体类抗炎药普拉洛芬滴眼液给药,6次/d,连续滴眼4 d,其后单用普拉洛芬进行给药,3次/d。
1.3 治疗指标 观察记录患者围治疗期的各项症状和体征变化并进行评分,两者相加可得综合评分,观察方法为在术后4 d、7 d、14 d和30 d分别观察记录患者症状和体征的治疗情况,并检查测量患者眼底和眼压的改变情况,对其进行评分的总体范围为0~4分:无症状评0分,轻度症状评1分,中度症状评2分,重度症状评3分,极重症状评4分[6]。
1.4 统计学方法 本文实验数据均采用SPSS 19.0来处理,计量资料采用“±s”表示,组间比较采用t检验;计数资料用“n,%”表示,组间比较采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 黄斑囊样水肿 黄斑囊样水肿患者在观察组发现1例,对照组发现11例,差异有统计学意义(χ2=8.865,P<0.05)。
2.2 前房闪辉评估 在术后各个检查时间点,观察组患者的前房闪辉评分数据均明显小于对照组,差异有统计学意义(P<0.01)。见表1。
2.3 眼压评估 在术后各个检查时间点,观察组患者的眼压评分数据均小于对照组,差异无统计学意义。见表2。
2.4 症状和体征的综合评分比较 所有患者治疗后的综合评分均随着治疗时间的增加而降低,在术后4 d和7 d时,观察组的综合评分显著低于对照组,差异具有统计学意义(P<0.05),而在术后14 d和30 d时,差异无统计学意义。见表3。
表1 两组患者前房闪辉评分比较(±s,pc/ms)Table 1 The comparison between two groups about the scores of anterior chamber flare(±s,pc/ms)

表1 两组患者前房闪辉评分比较(±s,pc/ms)Table 1 The comparison between two groups about the scores of anterior chamber flare(±s,pc/ms)
项目术后4 d术后7 d术后14 d术后30 d t值7.700 5.108 7.214 3.211观察组(n=100) 6.3±3.1 6.4±2.7 5.6±2.4 5.5±2.3对照组(n=100) 9.9±3.5 8.5±3.1 8.1±2.5 6.5±2.1 P值<0.01<0.01<0.01<0.05
表2 两组患者眼压评分比较(±s,mmHg)Table 2 The comparison between two groups about the scores of intraocular pressure(±s,mmHg)
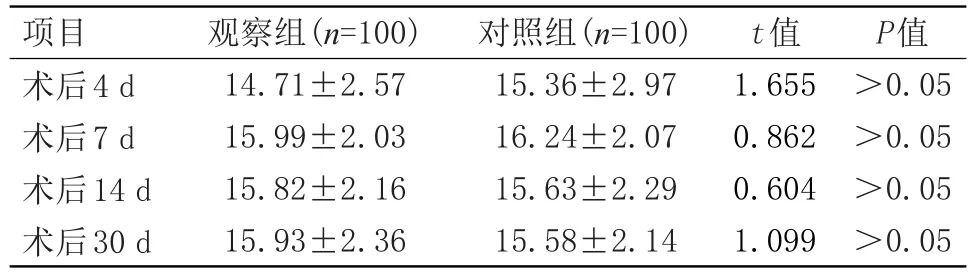
表2 两组患者眼压评分比较(±s,mmHg)Table 2 The comparison between two groups about the scores of intraocular pressure(±s,mmHg)
P值>0.05>0.05>0.05>0.05项目术后4 d术后7 d术后14 d术后30 d观察组(n=100) 14.71±2.57 15.99±2.03 15.82±2.16 15.93±2.36对照组(n=100) 15.36±2.97 16.24±2.07 15.63±2.29 15.58±2.14 t值1.655 0.862 0.604 1.099
表3 两组患者综合评分比较(±s,分)Table 3 The comparison between two groups about the comprehensive scores(±s,score)

表3 两组患者综合评分比较(±s,分)Table 3 The comparison between two groups about the comprehensive scores(±s,score)
P值<0.01<0.01>0.05>0.05项目术后4 d术后7 d术后14 d术后30 d观察组(n=100) 7.1±0.8 5.2±0.9 3.2±0.7 1.1±0.5对照组(n=100) 8.3±0.9 6.6±0.7 3.3±0.8 1.1±0.6 t值9.965 12.279 0.941 0
3 讨论
白内障患者术后炎症反应的常见影响因素源于手术操作导致的组织器官机械性损伤、超声能量影响或晶体植入体内后的异物反应等[7],由于物理化学因素会导致前列腺素分泌而对血液房水屏障造成影响和损坏,最终很容易诱发白内障术后炎症,同时蛋白会极易进入房水内而造成房水闪烁,房水中若出现炎症细胞等细胞则会引起房水细胞反应,由此可见对该病患者进行术后给药以控制炎症的关键点为抑制患者前列腺素等细胞因子的作用[8]。一般来讲,对此类患者在术后合理应用抗炎药物则能有效的消退炎症反应,进而减轻或者治愈超声乳化术后的前房反应,该疗法目前在临床上已经受到了广大医务工作者的普遍认可[9]。
随着超声乳化手术的不断发展完善,临床上对于白内障患者的术后炎症反应已经相对大大减轻,因此对于该术式联合人工晶体植入的患者可缩短糖皮质激素的给药疗程至两周以内,对于术后未见炎症反应的患者可以不用糖皮质激素药物治疗[10]。非甾体类抗炎药在使用中虽可见一定程度的眼压升高等不良反应,作用效率不如激素类药物迅速,但其在局部给药时并不会明显地损害患者眼角膜上皮细胞,且适应症更广泛疗效更良好,这就能很较好的弥补长期使用激素类药物会产生药物角膜毒性反应的缺憾[11]。本文研究结果与上述文献报道一致,在术后4天和7天时,观察组综合评分显著低于对照组,差异具有统计学意义(P<0.05),而在术后14天和30天时,差异无统计学意义。
综上所述,白内障患者术后联用妥布霉素地塞米松和普拉洛芬可以有效地起到早期抗炎和缓解术后不良反应的作用,具有良好的临床应用价值。
[1]Hu H,Fang M,Luo K,et al.Phacoemulsification and intraocular lens implantation for cataract induced by ocular ischemic syndrome:30-month follow-up[J]. Jcrs Online Case Reports,2015,3(1):22-26.
[2]Kessel L,Tendal B,Jørgensen KJ,et al.Post-cataract prevention of inflammation and maculared ema by steroid and nonsteroid alanti-inflammatory eye drops: a systematic review[J].Ophthalmology,2014, 121(10):1915-1924.
[3]Malik A,Sadafale A,Gupta YK,et al.A comparative study of various topical nonsteroidal anti-inflammatory drugs to steroid drops for control of post cataract surgery inflammation[J].Oman Journal of Ophthalmology,2016,9(3):150.
[4]黄霞,吴密,陈晓红.白内障超声乳化联合人工晶体植入治疗的临床护理[J].局解手术学杂志,2015,24(1):99-100.
[5]董立红.超声乳化联合人工晶体植入治疗超高度近视白内障疗效观察[J].临床和实验医学杂志,2012,11(20):1613-1615.
[6]白景山,张涛,张杰.手术治疗白内障对患者临床症状和生活质量的影响[J].现代医药卫生,2012,28(19):2921-2922.
[7]Zhang CH,Li N,Wang XY,et al.Influence of Lipoplus fat emulsion on postoperative nutritional status and early inflammatory response in patients with gastrointestinal malignancies[J]. Chinese journal of gastrointestinal surgery,2012,15(5):448-451.
[8]Takács AI,Kovács I,Miháltz K,et al.Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification[J]. Journal of Refractive Surgery,2012,28(6):387-391.
[9]Ji WJ,Chung BH,Kim EK,et al.The Effects of Two Non-Steroidal Anti-Inflammatory Drugs, Bromfenac 0.1%and Ketorolac 0.45%,on Cataract Surgery[J]. Yonsei Medical Journal,2015,56(6):1671-1677.
[10]Baiula M,Spampinato S.Mapracorat,a Novel Non-Steroidal Selective Glucocorticoid Receptor Agonist for the Treatment of Allergic Conjunctivitis[J].Inflammation&allergy drug targets,2014,13(5):289-298.
[11]Kim SJ,Schoenberger SD,Thorne JE,et al.Topical Nonsteroidal Anti-inflammatory Drugs and Cataract Surgery:A Report by the American Academy of Ophthalmology[J].Ophthalmology,2015,122(11):2159-2168.
Study of the clinical effect about the combination of the drugs hormonal and nonstemidal anti-imqammatory for patients with cataract after operation
Liu Hui,Liu Gang,Luo Li-li
(The First People’s Hospital of Neijiang,Neijiang,Sichuan,641000,China)
ObjectiveTo explore the clinical effect about the combination of the drugs hormonal and nonstemidal anti-imqammatory for patients with cataract after operation.MethodsTwo hundred patients with cataract received operation were divided randomly into the observation group which employed the combination of the drugs tobramycin dexamethasone and pranoprofen and the control group which employed tobramycin dexamethasone.Each group was containing 100 patients.The scores of every symptom,physical sign and general should be statistical record.ResultsAmong two hundred patients with cataract received operation,it is with significantly difference on the cystoid macular edema incidence rate and anterior chamber flare scores between the observation group and the control group,besides,the former numerical value is less than the latter(P<0.05). There is no significantly difference on the intraocular pressure scores between the observation group and the control group although the former numerical value is also less than the latter.In additon,it is with significantly difference on the general scores between the observation group and the control group,besides,the former numerical value is less than the latter after four days and seven days for the operation[(6.3±3.1)vs(9.9±3.5),(6.4± 2.7)vs(8.5±3.1)](P<0.05).There is no significantly difference on the general scores between the observation group and the control group although the former numerical value is also less than the latter after fourteen days and thirty days for the operation[(5.6±2.4)vs(8.1±2.5),(5.5±2.3)vs(6.5± 2.1)].Conclusion It is effective and valuable to resist inflammatory and adverse reaction with the combination of the drugs tobramycin dexamethasone and pranoprofen for patients with cataract after operation.
Cataract;Hormonal drugs;Nonstemidal anti-imqammatory drugs
10.3969/j.issn.1009-4393.2017.11.007