Supercapsular percutaneously-assisted total hip approach for the elderly with femoral neck fractures: study protocol for a prospective, open-label, randomized, controlled clinical trial
Liang-hao Wu, Bao-qing Yu*, Fan-cheng Chen
Department of Orthopedics, Pudong Hospital of Fudan University, Shanghai, China
Introduction
Femoral neck fracture is one of the most common types of fracture in the elderly.1-3Arti ficial hip replacement is currently the preferred treatment for femoral neck fractures,and is characterized by the lack of postoperative bone nonunion, femoral head necrosis and other complications, although longer operative time and larger surgical incision are unavoidable. Patients undergoing arti ficial hip replacement can recover to perform weight-bearing walks early after surgery, making rehabilitation rapid, therefore avoiding a variety of complications, such as bed rests. Hip replacement by posterolateral approach is generally used,but it is limited by large incision, cutting off the extortor,and postoperative hip dislocation.4-8
A minimally invasive approach for hip replacement has the advantages of reduced blood loss and trauma compared with conventional approaches.9The supercapsular percutaneously-assisted total hip (SuperPATH) approach (Appendix 1) is consistent with the posterolateral approach in the anatomical landmark, preserving all the advantages of the posterior approach.10Compared with the conventional approaches, SuperPATH has no neurovascular interface therefore reducing the risk of damaging blood vessels and nerves during surgery, reducing intraoperative blood loss, but retaining all of the joint capsules and supinator muscles, signi ficantly reducing the probability of postoperative dislocation of the hip. Osteotomy using this approach can be completed without hip dislocation, thus reducing the incidence of vascular distortion and postoperative deep vein thrombosis. Hip replacement via SuperPATH can be completed under direct vision rather than perspective inspection, and the surgical incision of the femur is made according to the femoral anteversion angle. In addition,this approach is also used for femoral intramedullary nail implantation. Therefore, these surgical procedures are more likely to be quickly learnt by clinicians. Preservation of the joint capsule and supinator muscles reduces the restriction of physical activity and speeds up rehabilitation.Moreover, there is a corresponding reduction in hospital stays and cost. However, SuperPATH technology is rarely reported in China because it was only recently introduced in few hospitals.
Previous studies reported that SuperPATH for arti ficial hip replacement exhibits a better short-term effect on elderly femoral neck fractures.11,12In this trial, the follow-up period will be prolonged to 6 months to observe the shortto-midterm effect in the elderly with femoral neck fractures.
Methods/Design
Study design
A prospective, single-center, open-label, randomized controlled clinical trial.
Study setting
Pudong Hospital of Fudan University, Shanghai, China.
Study procedures
Forty patients with femoral neck fractures admitted to the Pudong Hospital of Fudan University, China were randomly divided into two groups. The patients in the experimental group were treated with SuperPATH femoral head replacement, and those in the control group were treated by femoral head replacement using the conventional posterolateral approach. All patients will be followed up for 1 week and 6 months postoperatively (Figure 1).SuperPATH hip replacement will be performed under direct vision to reduce radiation damage to the patients.The surgical incision made on the femur is used for both SuperPATH and femoral intramedullary nail implantation,and this method is easier for the clinicians to perform.Noticeably, the SuperPATH approach can be changed at any time into the standard posterolateral approach if there are any operative dif ficulties during surgery. Preservation of the joint capsule and supinator muscles by SuperPATH hip replacement can prevent the restriction of activities and enhance rehabilitation in patients. In the study, clinical data, including Harris hip scores, length of incision,operative time, intraoperative blood loss, postoperative drainage, hospital stay, will be compared between hip replacement by SuperPATH and the posterolateral approach in elderly with femoral head fractures. Clinical data have been collected since January 2015 and the follow-up visit data will be collected until August 2017.
Inclusion criteria
Patients were required to meet all of the following conditions to be included in this trial:
· Femoral head fractures as diagnosed by X-ray and CT· Garden III, IV13(Appendix 2)
· Aged > 75 years
· Both genders
Exclusion criteria
Patients presenting with any one or more of the following conditions were excluded from this trial:
· Fractures with spinal cord injury
· Fractures with nerve injury
· Refusal to sign the informed consent
Baseline data
Baseline data, including demographic data, clinical data,and general disease history will be collected from the participants (Table 1).

Figure 1: Flow chart of the study protocol.
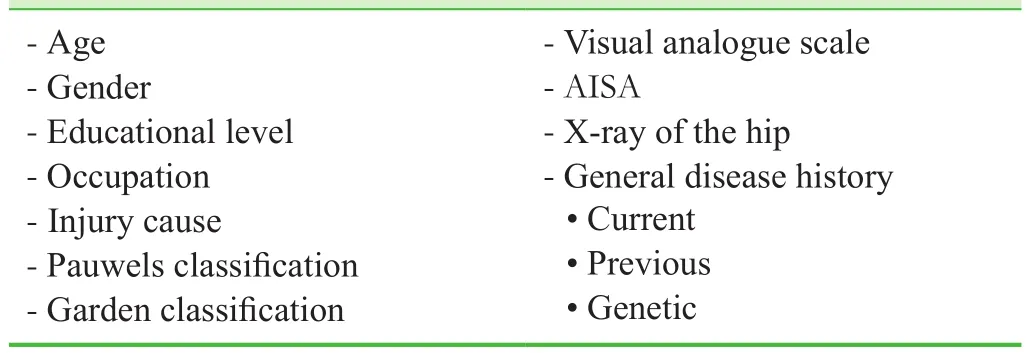
Table 1: Baseline data of all participants
Recruitment
Potential patients hospitalized in the Pudong Hospital of Fudan University were informed about the trial through a recruitment advertisement on the hospital bulletin board.Those interested in participating were screened by physicians, and eligible patients were given free examinations and drug therapy related to hospitalization, as well as treatment and follow-up guidance from our medical staff. All participants and their relatives were informed of the study protocol and provided written consent prior to enrollment in the trial.
Randomization and blinding
A random number table was generated using SPSS 13.0 software (SPSS, Chicago, IL, USA). The starting point and order of sampling was arbitrarily determined on the random number table, and the number of each sample was selected from the random number table. The 40 participants were equally randomized into experimental and control groups (n= 20 per group). This is an open-label study. All participants,surgeons, and assessors were informed of patient assignment and therapeutic schedules.
Interventions
(1) Control group. Participants were positioned in standard lateral decubitus with the operative leg upward, and underwent hip replacement via the posterolateral approach. An arc-shaped incision of 10–15 cm started about 5 cm below the posterosuperior iliac spine and extended laterally along the gluteus maximus and distally to the greater trochanter, and then was turned 3 cm distally to the femoral shaft. The skin,subcutaneous tissue, and fascia lata were cut. The gluteus maximus posterior to the greater trochanter was separated from the gluteus medius by blunt dissection to expose the extortor muscles, including the musculus piriformis, gemellus superior, musculus obturator internus, and gemellus inferior,which were cut off at the trochanteric fossa. Then, the hip joint capsule was exposed and the posterior capsule was cut.The femoral neck was cut 1.5 cm above the lesser trochanter and removed. Following reaming of the femoral medullary cavity using reamers of different diameters, a femoral head prosthesis template and standard femoral head prosthesis were placed. The template could be taken out if the flexion,abduction, external rotation, internal rotation, and tightness of the femoral head were satisfactory. Afterwards, a metal femoral prosthesis (Stryker Corporation, Kalamazoo, MI,USA; a biomechanical hip prosthesis, with titanium stem with proximal hydroxyapatite coating), ceramic head, and cobalt-chrome-nickel alloy ball, was installed followed by hip joint reduction and negative pressure drainage. Finally,the incision was sutured in successive layers after repair of the extortor muscles.14
(2) Experimental group. Participants were positioned in standard lateral decubitus, flexing the operative leg 45° and internally rotating it 10° to 15°. The foot of the operative leg was elevated on a pad. An incision was initiated 1 cm distal to the tip of the greater trochanter and extended 6–8 cm proximal with an angle of 15°, in line with the femoral axis. The gluteus maximus was bluntly split, to expose the posterior border of the gluteus medius. A retractor was placed under the gluteus medius. The operative leg was then abducted and extorted to release tension on the extortor. The piriformis was retracted and the anterior border of the gluteus minimus was pushed to expose the hip capsule.The capsulotomy was initiated at the saddle of the femoral neck, and extended proximally to the superior border of the glenoid labrum. The femoral neck was cut in a wedge-shaped manner and then removed with the help of an assistant. The operative leg was flexed and abducted to expose the saddle of the femoral neck. A round calcar femorale tapper was used to make an approach for inserting the reamer from the saddle of the femoral neck to the superior border of the femoral head.The inner wall of the greater trochanter was scraped with a curette. The medullary cavity was reamed using reamers of different diameters. Under C-arm fluoroscopy, the most suitable reamer was located about 1.5 cm above the lesser trochanter, and the remaining femoral neck was removed with a pendulum saw in line with the tip of the reamer.15Then, PR prosthesis (Wright Medical Group, Memphis,TX, USA) was placed. Head and neck prostheses were selected based on perspective results, and placed first into the stem followed by the femoral head and neck reduction.The incision was thoroughly rinsed and the capsule was repaired with a continuous suture. The incision was then closed in layers. A routine negative pressure drainage tube was inserted.
(3) Postoperative management and rehabilitation. All the participants were given anti-infection treatment once postoperatively, a change of dressing, and removal of the drainage tube 24 hours postoperatively. Training for muscle contraction of the lower limbs was initiated at postoperative day 1 under a physician’s guidance. Patients can walk out of bed using a walking frame or stick as soon as they can.16
Outcome measures
Primary outcome measure
Harris hip scores at baseline and 1 week and 6 months postoperatively will be collected. This is used to assess hip function recovery in patients. The hip function is assessed by Harris scores ranging from 0–100: excellent ≥ 90, good 80–90, fair 70–79, and bad < 70. The higher scores indicate better hip function.
Secondary outcome measures
· Length of surgical incision: a smaller surgical incision causes smaller surgical trauma to patients.
· Intraoperative blood loss: less blood loss indicates the surgical practice is more normative and safe.
· Operative time: a short operative time indicates this operation process is more successful.
· 24-hour postoperative drainage: a small amount of postoperative drainage suggests less incision exudate, and a higher quality operation.
· Hospital stay: a shorter hospitalization time indicates a rapid postoperative recovery in the patients.
Other outcome measure
Incidence of adverse events at 1 week and 6 months postoperatively is used to assess the incidence of postoperative complications in patients.
The schedule of outcome measurement assessment is shown in Table 2.
Adverse events
Postoperative adverse events including incision pain and infection, back muscle pain, spinal cord/nerve injury, length inequality of the lower limbs, prosthesis falling-off, and prosthetic loosening will be recorded during the follow-up period. If severe adverse events occur, details including the data of occurrence, type of adverse events, and therapeutic measures will be reported to the project manager and the institutional review board within 24 hours.
Data collection, management, analysis, and open access
Data collection
Clinical data, including demographic data, disease diagnosis, accompanying diseases, and allergic history (drug allergy), will be collected and summarized using standardized case report forms. These data will be processed and recorded electronically.
Researchers will be responsible for data processing, confirming, and locking. Locked data will prevent alterations and it will be preserved by the Pudong Hospital of Fudan University. In addition to the study researchers, only the persons who have permission will have the right to query the database.
Data analysis
All data will be statistically analyzed by professional statisticians who will be responsible for completing an outcome analysis report that will be submitted to the principle investigator who will be responsible for completing a research report. An independent data monitoring committee is responsible for data monitoring and management throughout the entire trial to ensure scienti fic accuracy, stringency,authenticity, and integrity.
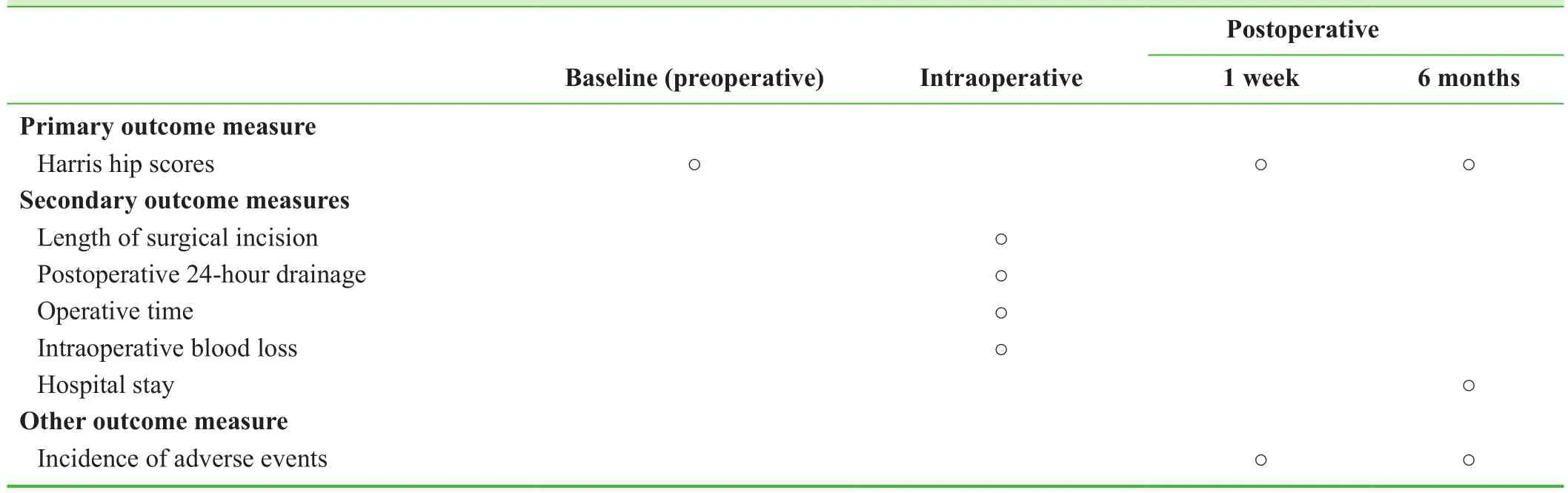
Table 2: Timing of outcome assessment
Open data
Anonymized data of the trial will be released at http://www.figshare.com.
Sample size
Based on our previous experience, we assumed that the 1-week postoperative Harris hip scores would be increased by 90% in the experimental group and by 50% in the control group. Considering α = 0.05 (two-sided), β = 0.1, and power= 90%, the necessary sample size was calculated to be n = 25 per group using PASS 11.0 software (NCSS, Kayville, UT,USA). With a predicted dropout rate of 20%, the required sample size was n = 30 per group. After application of the inclusion and exclusion criteria, our final group size was n = 20 per group.
Statistical analysis
All data will be statistically analyzed by statisticians using SPSS 13.0 software (SPSS, Chicago, IL, USA) in accordance with the intention-to-treat principle. Normally distributed measurement data will be expressed as means,standard deviations, minimums, and maximums, while non-normally distributed data will be expressed as lower quartiles, medians, and upper quartiles. Count data will be expressed as a percentage.
The Mann-Whitney U-test will be used for intergroup comparisons of Harris hip scores, length of surgical incision, intraoperative blood loss, operative time, 24-hour postoperative drainage, and hospital stay. The Pearson χ2test will be used to compare the incidence of adverse events between the two groups. The statistical signi ficance level will be set as α = 0.05.
②抑菌试验:灭菌吸管吸取制备的菌悬液1 ml加入100 ml已融化并保温在水浴中(48~50℃)的细菌平板培养基内,使菌含量达到1×106cfu/ml。融化后固体平板培养基冷却45℃左右,加入1 ml制备好的菌液,然后倒入无菌培养皿中,静置冷却,等其凝固后,用无菌镊子将灭菌牛津杯垂直放在含菌平板培养基表面,轻轻按压(每个平板放4个牛津杯)。用移液器吸取100 μl冬凌草醇提物溶液,加入到牛津杯孔内,同时用甲醇做空白对照。然后,将培养皿放入培养箱中,细菌37℃培养15h后测量抑菌圈直径。
Trial Status
As of December 2016, we had completed case collection and postoperative 1-week follow-up analysis, and the 6-month follow-up data (including the incidence of adverse events) will be collected until August 2017. The speci fic preliminary results are as follows:
(1) Participants: 40 cases were included consisting of 12 males and 28 females, aged 75–89 years with a mean age of 80.5 years. All the participants were diagnosed with femoral neck fractures by X-ray and CT. According to the Garden classi fication, there were 32 cases of type III and 8 cases of type IV. Trauma causes included falls in 37 cases, and traf fic accidents in 3 cases.
(2) Except for a longer operative time, SuperPATH minimally-invasive surgery was superior to the posterolateral approach with respect to the length of surgical incision, intraoperative blood loss, postoperative drainage, and 1-week postoperative Harris hip scores (Table 3).
(3) Incidence of adverse events: no complications, such as incision infection and length inequality of the lower limbs,occurred in the two groups within 1 week postoperatively.
(4) Conclusion: SuperPATH had a better short-term effect than the posterolateral approach regarding the hip replace-ment treatment of elderly femoral head fractures.
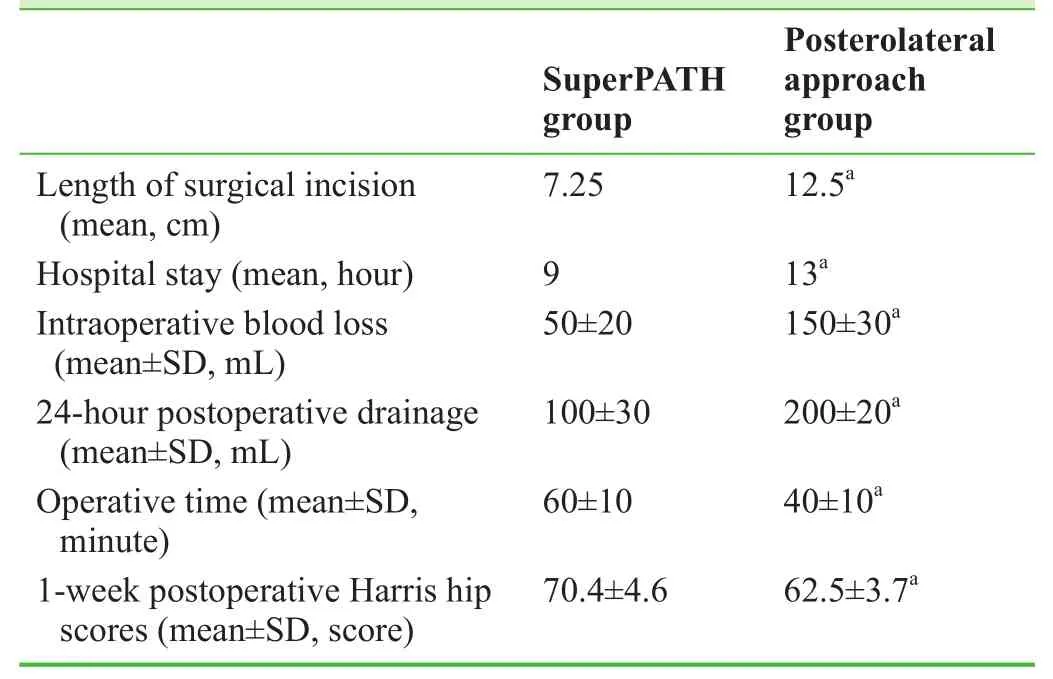
Table 3: Outcome comparison between the two groups
Discussion
Preliminary results showed that SuperPATH minimallyinvasive surgery caused less blood loss and smaller trauma compared with conventional approaches. This is of great signi ficance for elderly patients with femoral neck fractures. SuperPATH can signi ficantly reduce the incidence of complications in such patients, allow rapid rehabilitation,and reduce the use of special traction beds and equipment.It is an easier and safer method for surgeons and patients,which is worthy of clinical application.
Results from the 1-week follow-up visit showed signi ficantly improved length of surgical incision, intraoperative blood loss, postoperative drainage, and hospital stay in patients treated with SuperPATH compared with those undergoing hip replacement via conventional approaches,although the operative time was longer in the SuperPATH group. Moreover, the improvement in skilled operation and use of tools allowed the surgery basically to be completed within 60 minutes. Therefore, the posterolateral approach for hip replacement has no signi ficant disadvantages. The mean surgical incision length for SuperPATH was only 7.25 cm, half that of the conventional approach. The amount of intraoperative bleeding and postoperative drainage was also signi ficantly reduced. Furthermore, with the accumulation of experience, the drainage tube will no longer be placed in future surgery, and patients with good physical condition will be allowed to walk out of bed the same day after surgery, to achieve the maximal rapid rehabilitation. This method will greatly reduce the incidence of complications,such as bed rest, reduce hospital stay, and indirectly reduce the cost of treatment. In this study, 1-week postoperative Harris hip scores in the SuperPATH group were signi ficantly better than in the posterolateral approach group, which may be related to the implementation of earlier rehabilitation exercise after surgery. The 6-month follow-up data collection is ongoing.
This study had some limitations. There were no international assessment outcomes for neurological function and pain. Follow-up time was short (no more than 1 year).In addition, overall factors will affect the accuracy of the study results.17-19
We hope this study will con firm that SuperPATH minimally-invasive surgery for the treatment of femoral neck fracture in the elderly is safer, more reliable, with better short-to-midterm effects (1 week, 6 months postoperatively)compared with the posterolateral approach.
Appendix 1 The SuperPATH approach for hip replacement
The superPATH approach was developed by James Chow from St. Luke's Medical Center, Phoenix, Arizona, USA.It is a hybrid of the Superior Capsulotomy (SuperCap) approach (developed by Dr. Stephen Murphy, New England Baptist Hospital, Boston, Massachusetts, USA) and the percutaneously-assisted total hip technique (developed by Dr. Brad Penenberg, Cedars-Sinai Medical Center, LA,USA). The SuperPATH approach has been widely used in clinical practice, and this approach is consistent with the traditional posterolateral approach regarding the use of anatomic landmarks, retaining all the advantages of the latter.
Appendix 2 Garden classification for femoral head fractures
Grade I is an incomplete fracture; Grade II is a complete fracture without bone displacement; Grade III is a complete fracture with partial displacement of the fracture fragments that the femoral head is extended, externally rotated slightly and shifted upward; and Grade IV is a complete fracture with total displacement of the fracture fragments that the femoral head presents with overt external rotation and upper shift.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
LHW conceived and designed the study protocol, wrote the paper,read and approved the final version of the paper for publication.BQY and FCC completed the trial.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
1. Liu M, Yang J, Yu X, et al. The role of perioperative oral nutritional supplementation in elderly patients after hip surgery.Clin Interv Aging. 2015;10:849-858.
2. Taraldsen K, Thingstad P, Sletvold O, et al. The long-term effect of being treated in a geriatric ward compared to an orthopaedic ward on six measures of free-living physical behavior 4 and 12 months after a hip fracture-a randomised controlled trial. BMC Geriatr. 2015;15:160.
3. Tsertsvadze A, Grove A, Freeman K, et al. Total hip replacement for the treatment of end stage arthritis of the hip: a systematic review and meta-analysis. PLoS One. 2014;9:e99804.
4. Kawaji H, Uematsu T, Hoshikawa N, et al. Mid-term clinical results of versys hip system (zimmer) uncemented total hip replacement arthroplasty. J Nippon Med Sch. 2016;83:184-187.
5. Yi J, Han KY, Nam YJ, Kim KW. Result of modular necks in primary total hip arthroplasty with a average follow-up of four years. Hip Pelvis. 2016;28:142-147.
6. Shah SB, Manson TT, Nascone JW, Sciadini MF, O'Toole RV.Radiographic determinants of early failure after posterior wall acetabular fracture fixation. Orthopedics. 2016;39:e1104-1111.
7. Zhang ZF, Min JK, Zhong JM, Wang D. Distal fixation prosthesis for unstable intertrochanteric fractures in elderly patients: a mid-term follow-up study. Zhongguo Gu Shang. 2016;29:491-495.
8. Schäf fler A, Freude T, Stuby F, et al. Surgical treatment of acetabulum fractures with a new acetabulum butter fly plate. Z Orthop Unfall. 2016;154:488-492.
9. Zhao J, Liu SP, Lin B. Comparison analysis of ef ficacy and effects on the life qualiy of minimally invasive and traditional total hip arthroplasty surgery. Linchuang he Shiyan Yixue Zazhi. 2015; 14:750-753.
10. Bodrogi AW, Sciortino R, Fitch DA, Gofton W. Use of the supercapsular percutaneously assisted total hip approach for femoral neck fractures: surgical technique and case series. J Orthop Surg Res. 2016;11:113.
11. Huang GY, Xia J, Wei YB. Short-term ef ficacy of hip arthroplasty through the SuperPATH approach for femoral neck fractures in very elderly patients. Guoji Gukexue Zazhi.2016;37:331-336.
12. He QX, Qiao JF, Liu YQ. Minimally invasive total hip arthroplasty and conventional total hip replacement. Guangdong Yixueyuan Xuebao. 2016;34:189-292.
13. Frandsen PA, Andersen E, Madsen F, Skjødt T. Garden's classi fication of femoral neck fractures. An assessment of interobserver variation. J Bone Joint Surg Br. 1988;70:588-590.
14. Cao JG, Wang L, Liu J. The use of clamped drainage to reduce blood loss in total hip arthroplasty. J Orthop Surg Res.2015;10:130.
15. Hu FY, Lai RH, Liang MR, An YT, Hu TS. Clinical application of minimally invasive total hip arthroplasty with SuperPATH approach. Weichuang Yixue. 2016;11:416-418.
16. Tao YZ. Study for the peri-operation nursing and rehabilitation nursing for patients with Total hip arthroplasty. Hushi Jinxiu Zazhi. 2015;30:1280-1282.
17. Wu T, Zhang GQ. Minimally invasive treatment of proximal humerus fractures with locking compression plate improves shoulder function in older patients: study protocol for a prospective randomized controlled trial. Clin Transl Orthop.2016;1:51-57.
18. Yin PB, Long AH, Shen J, Tang PF. Treatment of intertrochanteric femoral fracture with proximal femo¬ral medial sustainable intramedullary nails: study protocol for a randomized controlled trial. Clin Transl Orthop. 2016;1:44-50.
19. Li Z. Minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws for repair of distal radius fracture: study protocol for a randomized controlled trial. Clin Transl Orthop. 2016;1:58-63.
 Clinical Trials in Orthopedic Disorder2017年2期
Clinical Trials in Orthopedic Disorder2017年2期
- Clinical Trials in Orthopedic Disorder的其它文章
- Efficacy of endoscopic transantral versus transorbital surgical approaches in the repair of orbital blowout fractures: study protocol for a randomized controlled trial
- Platelet-rich plasma combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures: study protocol for a prospective, randomized, controlled clinical trial
- Effects of lumbar plexus-sciatic nerve block combined with sevoflurane on cognitive function in elderly patients after hip arthroplasty: study protocol for a prospective, single-center,open-label, randomized, controlled clinical trial
- Effects of two different tranexamic acid administration methods on perioperative blood loss in total hip arthroplasty: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Should angiography be done in suspected tuberculosis of spine in an endemic country? – Hemangioma masquerading as tuberculosis of spine
