Platelet-rich plasma combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures: study protocol for a prospective, randomized, controlled clinical trial
Zi-chun Zhao*, Zhao-wei Li, Hong-xiu Yan, Bao-ming Tang, Chun-liang Li, Qi-fu Zhang, Rong Ren, Pei Li,Sheng-long Jia
Department of Trauma Orthopedics, Affiliated Hospital of Qinghai University, Xining, Qinghai Province, China
Introduction
History and current related studies
Fracture healing is a continuous process, and disturbance of any phase by unfavorable factors can block the healing process.1-3A clinical study found that the non-healing rate of long bone fractures was approximately 5%.4A certain site and type of fracture that has not healed within a particular time period (usually 3–6 months) is described as delayed union by the US Food and Drug Administration.In addition, a fracture that has not healed after 9 months and shows no tendency for further healing in the next 3 months is referred to as nonunion.5,6Based on the fracture end activity, nonunion is further classi fied into hypertrophic nonunion and atrophic nonunion.7,8Hypertrophic nonunion is mostly caused by unstable fixation of the fracture ends,and can be cured by strengthening the fracture site stability using conventional surgery. Atrophic nonunion is dif ficult to cure, because the lack of adequate blood supply and bone formation at the fracture ends leads to inability of periosteal callus formation.7,8At present, atrophic nonunion is commonly treated by internal and external fixation combined with autologous bone graft, but this method has a long treatment cycle, and there remain cases where the nonunion cannot be cured.9
Platelet-rich plasma (PRP) is blood plasma that has been enriched with platelets through centrifugation of autologous blood.10Activated platelets secrete platelet-derived growth factor, transforming growth factor beta, vascular endothelial growth factor, and epidermal growth factor. These growth factors promote cell proliferation, differentiation, matrix synthesis, and vascular regeneration, and accelerate tissue healing and bone repair.11PRP contains a large number of leukocytes, which locally phagocytize bacteria, scavenge necrotic tissue, inhibit in flammatory reaction, and resist infection.12In addition, PRP fibrin can locally build the three-dimensional structure required for tissue repair. Since Assoian et al.13first isolated PRP and used it for clinical purposes in 1984, PRP has received increasing attention in areas such as oral and maxillofacial surgery, orthopedics, plastic surgery, and neurosurgery.
Main objective
This randomized controlled trial aims to objectively analyze the effectiveness of PRP combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures.
Distinguishing features from related studies
In recent years, there have been a number of Chinese studies on the use of PRP in the treatment of nonunion (Table 1). However, there have been no randomized controlled studies on the therapeutic effect of PRP combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures.
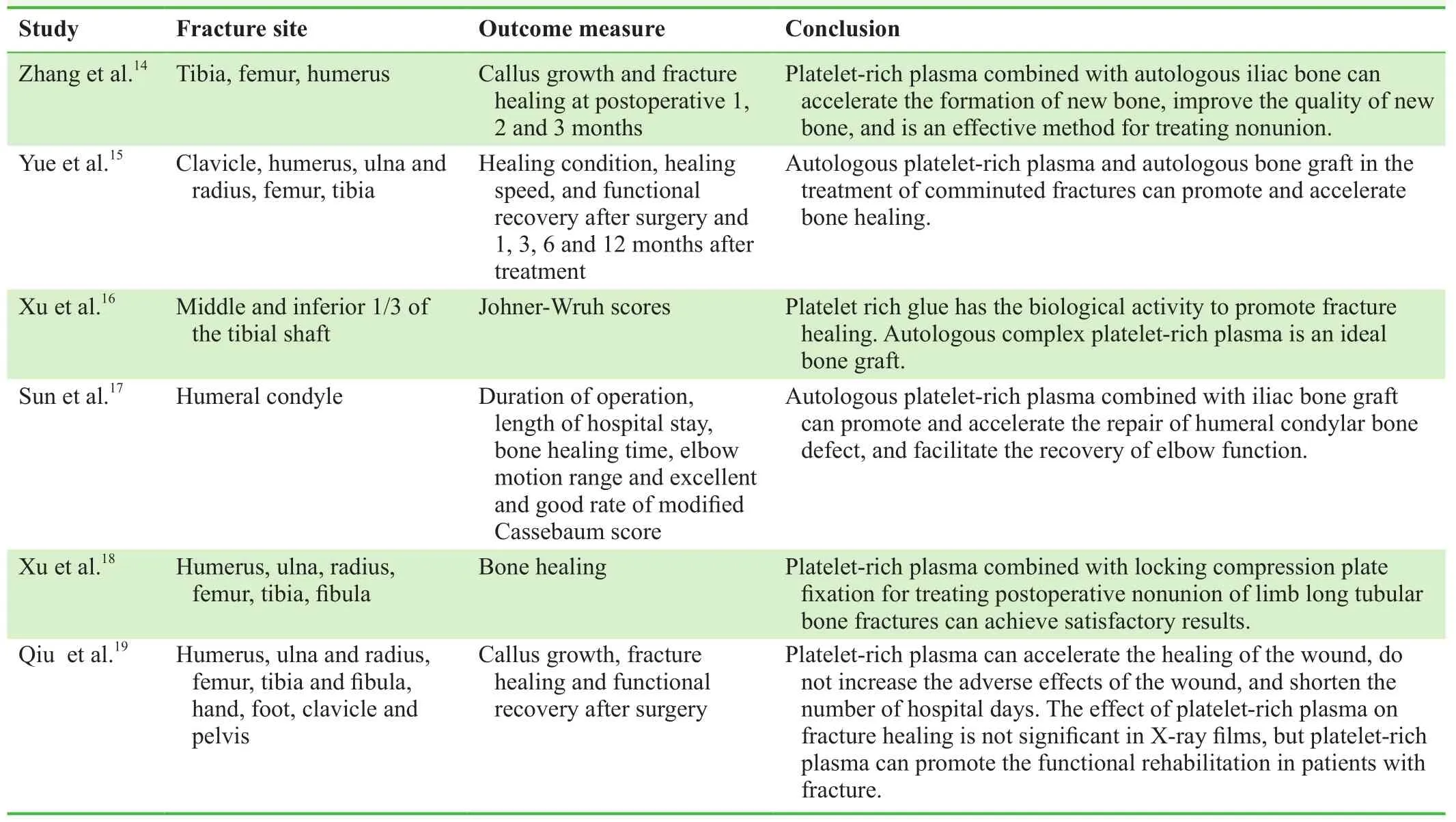
Table 1: Clinical studies on platelet-rich plasma in the treatment of nonunion
Methods/Design
Study design
This trial was designed in August 2014, and case recruitment was completed in September 2016. This is a prospective,open-label, randomized, controlled clinical trial at the Affiliated Hospital of Qinghai University, China.
After screening according to inclusion and exclusion criteria, 92 patients with atrophic nonunion of femoral shaft fractures were equally and randomly divided into a control group and an experimental group. The patients in the control group received conventional surgery, while the patients in the experimental group were injected with autologous PRP in addition to receiving conventional surgery.
The primary outcome was the fracture healing rate at 9 months postoperatively. The secondary outcomes were visual analogue scale scores in resting state and passive motion, healing time, treatment costs, and adverse reactions at 3, 6, 9, and 12 months postoperatively.
A flow chart of the study protocol is shown in Figure 1.
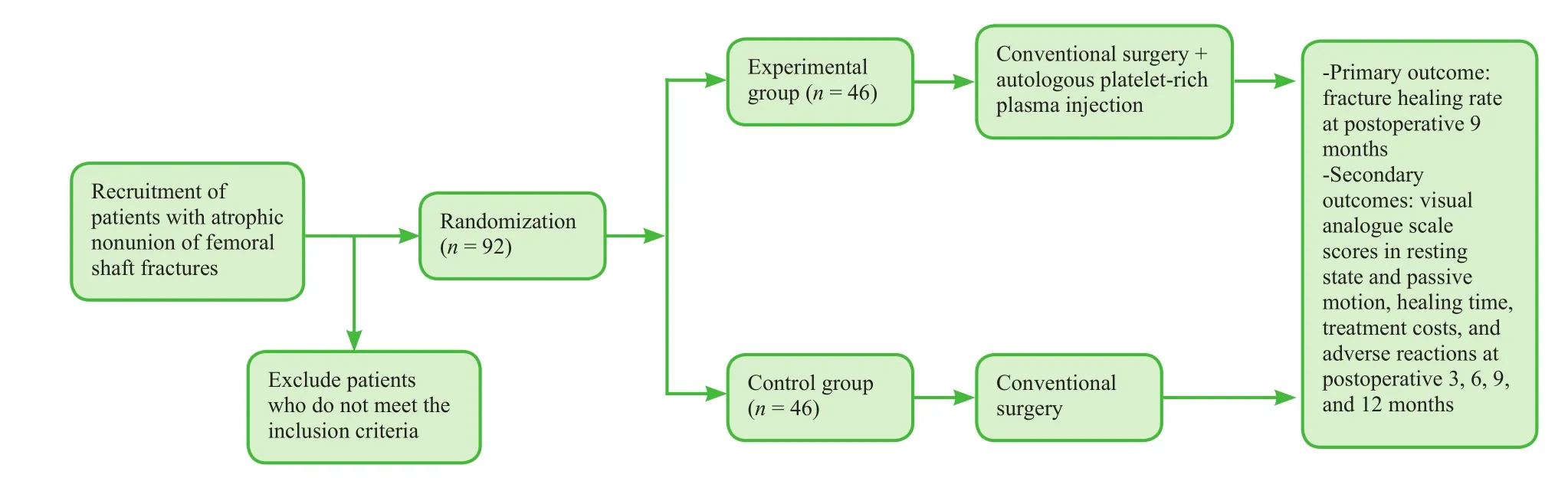
Figure 1: Trial flow chart.
Study participants
We enrolled patients with atrophic nonunion of femoral shaft fractures who were treated at the Af filiated Hospital of Qinghai University, China.
Inclusion criteria
Patients meeting with all of the following criteria were considered for study inclusion:
· Femoral shaft fractures
· Fracture time of more than 9 months5,6
· X-rays revealing a gap and sclerosis at the fracture ends,medullary closure, and osteoporosis, with absence of trabecular bone formation in the callus, for more than 3 months5,6
· Magnetic resonance images revealing a widened gap and atrophic fracture ends, with a small amount of or even no callus formation7
· Histological images revealing a gap at the fracture ends filled with fibrous tissue without osteogenic activity7
· Age of 18–70 years
Exclusion criteria
Patients with one or more of the following conditions were excluded from the study:
· Underlying disease affecting wound healing, such as diabetes, hematological system diseases, immune diseases,and connective tissue diseases
· Pregnancy or lactation
· Heart, lung, liver, and kidney dysfunction
· Participation in other clinical trials
Withdrawal criteria
Patients with one or more of the following conditions were withdrawn from the study:
· Development of a complication affecting the treatment ef ficacy and safety or a disease affecting the treatment outcome
· Combined use of other therapies or drugs to speed up the treatment effect
· Inability to complete the follow-up
Sample size
The effectiveness of surgery alone in the treatment of atrophic nonunion was reported to exceed 75%.20In our experience, the effectiveness of PRP combined with conventional surgery for atrophic nonunion was approximately 90%. Considering a power of 1 – β = 0.9 with a signi ficance level of α = 0.05 (two-sided), a sample size of n = 133 per group was required according to calculations performed with PASS 11.0 software (NSCC LLC,Kaysville, UT, USA). Assuming a patient loss rate of 20%,we required 160 patients per group. Owing to the limited time, 92 patients were recruited, and each group had a total of 46 cases.
Recruitment
Recruitment information was posted on the hospital bulletin boards. Patients were able to contact the project leader indirectly through their attending physician, or directly by telephone, email, and WeChat. After providing informed consent, participants who met the inclusion and exclusion criteria were enrolled.
Baseline analysis
Baseline data were collected at the time of enrollment. The detailed items are listed in Table 2.
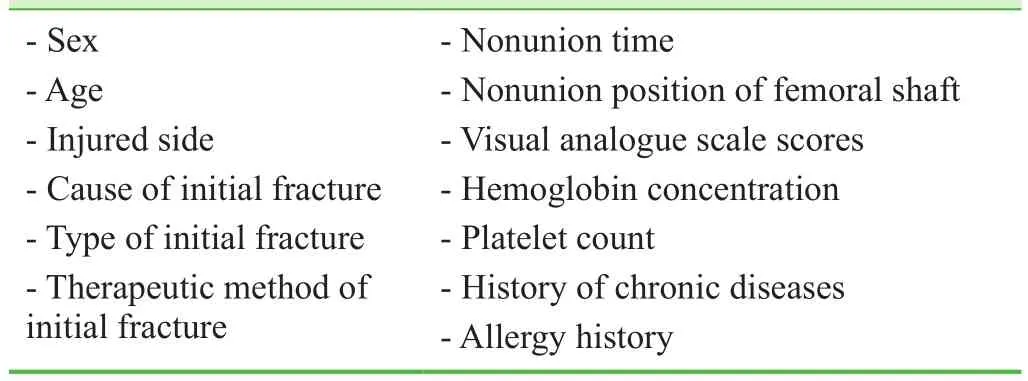
Table 2: Baseline data of the included patients
Randomization and blinding
According to the patient admission order, patients were equally randomized into a control group and an experimental group (n = 46 per group) by statisticians using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA). The patients, physicians, and assessors were not blinded to the group information.
Interventions
Control group
After the fracture site was anesthetized, the skin was incised.The original fixator was removed. The nonunion site was exposed, and the scar tissue at the fracture ends was cleaned.The hardened bone was removed, and the medullary cavity was passed through. The periosteum was removed as little as possible during the operation. The fracture ends were reset and re fixed using a plate, intramedullary nail, and screw. The fracture ends were pressurized, or an autologous, allogeneic,or arti ficial bone graft was used around the fracture ends.21-27
Experimental group
Together with the conventional surgery described above,PRP was injected into the affected site.
Preparation of PRP
PRP was prepared using the Landesberg method.28Brie fly,approximately 30 mL of blood was collected from the elbow vein and treated with 3 mL of sodium citrate for anticoagulation. After shaking, the blood was centrifuged twice. After the first centrifugation at 200 × g for 10 minutes,the supernatant to 3 mm below the interface was obtained and moved to a new centrifuge tube. After balancing, the second centrifugation was conducted by the same method.The supernatant was moved to a sterile centrifuge tube,and an appropriate amount of the supernatant was used for a sterility test. The remaining supernatant (2.5 mL) was resuspended, and the obtained platelet fraction was de fined as PRP. PRP (20 μL) was examined for the number of platelets.Activators (mixture of thrombin at final concentration of 100 U/mL and tranexamic acid at 25 mg/mL) were added before use.
Local injection of PRP
The fracture site was locally anesthetized. The puncture needle was precisely inserted into the nonunion site. After removal of the scar tissue at the nonunion site and with the needle maintained in place, 5 mL of PRP plus activators was injected into the injury site using a medicine mixer with double syringes. After local compression, the wound was bandaged. The affected limb was fixed.
Postoperative rehabilitation
In both groups, a continuous passive motion device(Beijing Zhongxi Yuanda Technology Co. Ltd., Beijing,China) was used from postoperative day 2 for 30 minutes/time twice per day. At 2 weeks postoperatively, the patients were allowed to get out of bed with crutches,but were not allowed to bear heavy weight. X-ray films revealing growth of the callus determined the partial or full weight-bearing time.21-27
Outcome measures
Primary outcome measure
Fracture healing rate at 9 months postoperatively: Disunion was identi fied if the fracture had not healed at 9 months postoperatively.6Fracture healing included clinical healing and bone healing.
Clinical healing criteria: 1) Absence of tenderness at the local site and no longitudinal percussion pain; 2) no abnormal activity at the local site; 3) X-ray films showing a blurred fracture line and continuous callus through the fracture line; 4) in cases with removal of external fixation,continuous walking for 3 minutes, not less than 30 steps; 5)fracture without any deformation for 2 weeks.29
Bone healing criteria: 1) Meeting clinical healing criteria;2) X-ray films revealing trabecular bone passing through the fracture line.29
Secondary outcome measures
· Visual analogue scale scores: A visual analogue scale is a method for assessing pain intensity. Using a ruler with 10 scales, the ends are set at 0 and 10, respectively,where 0 represents no pain and 10 represents the most unbearable severe pain. The side with the scales was at the back for the patient. The patient was allowed to mark the location of their pain on the ruler. The evaluator then selected the score according to the mark on the ruler.30The visual analogue scale scores in resting state and passive motion were recorded.
· Healing time: Time for fracture healing.
· Treatment costs: Costs from admission to fracture healing.
· Adverse reactions: Postoperative fever, infection, leukocyte abnormality, unequal leg length, and paresthesia.
The schedule for the outcome measurement assessments is shown in Table 3.
Data management
Clinical researchers filled in the clinical trial observation form to ensure that the data were accurate, complete, and collected in a timely manner. For the trial, all data would be input into a computer. After the data collection, the main clinical investigators and inspectors would monitor and check the integrity and accuracy of the data. Data processing statisticians would further verify and check the completeness and accuracy of the data after data entry. The anonymized trial data will be published at www.figshare.com.
Statistical analysis
Al data were analyzed using SPSS 17.0 software (SPSS,Chicago, IL, USA). Measurement data were expressed as the mean ± SD. Count data were expressed as percentages.A normality test and variance homogeneity test were conducted. Normally distributed data with homogeneity were compared by one-way analysis of variance. Non-normally distributed data were compared by Wilcoxon’s two-sample rank-sum test.
The incidence of adverse reactions in the two groups was compared by the chi-square test.
A value of P < 0.05 was considered statistically signi ficant. The results followed the intention-to-treat principle.
Confidentiality
The clinical trial observation forms and informed consent forms were password-protected. No persons other than authorized researchers were able to access these forms.
Ethical requirements
The study protocol was approved by the Ethics Committee of the Af filiated Hospital of Qinghai University of China (approval number: QHG0223A). All protocols were performed in accordance with the Ethical Principles for Medical Research Involving Human Subjects in the Declaration of Helsinki. The writing and editing of the article were performed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) (Additional file 1). The trial was registered in ClinicalTrials.gov (identi fier: NCT03129971). Written informed consent was provided by each patient and their family members after they indicated that they had fully understood the treatment plan.
Trial Status
The trial began in August 2014. Ninety-two patients were enrolled and followed. The partial results are as follows:Ninety-two patients will be followed for 8–26 months.
The visual analogue scale scores did not differ signi ficantly between the experimental group and the control group on postoperative days 1–3 (P > 0.05; Table 4).
The healing rate was higher in the experimental group compared with the control group (94% vs. 78%, P < 0.05;Table 5).
The healing time was signi ficantly shorter in the experimental group compared with the control group (91.6 ± 6.9 vs. 115.2 ± 8.4, P < 0.05; Table 6).
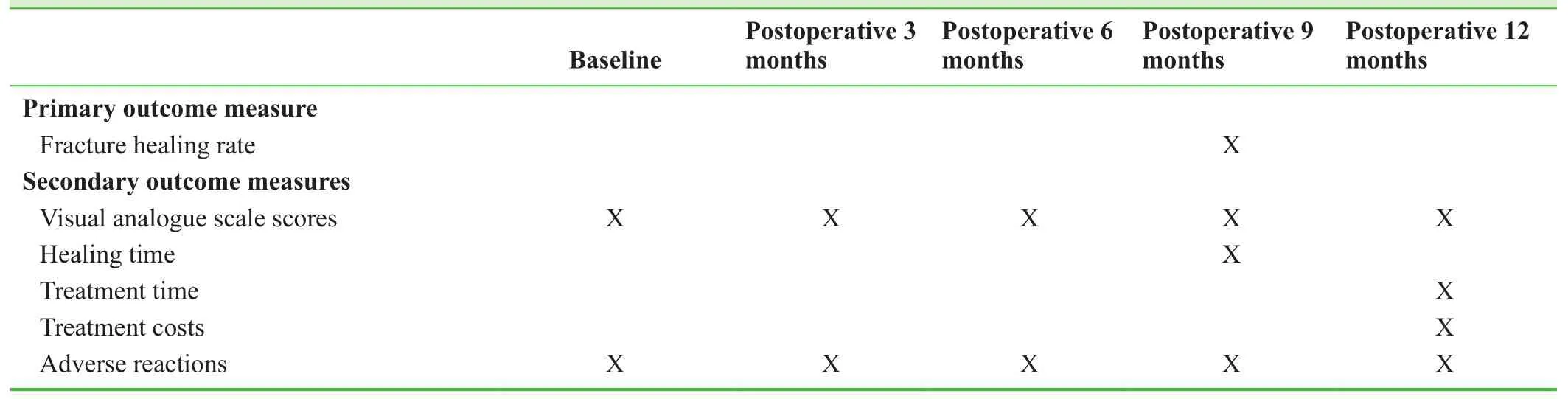
Table 3: Timing of outcome assessments
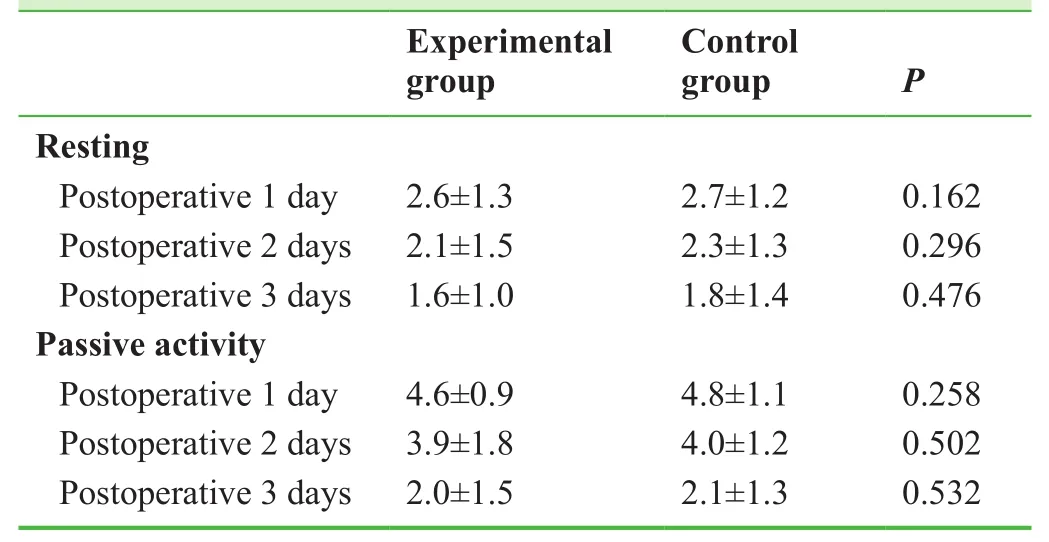
Table 4: Effects of platelet-rich plasma on visual analogue scale scores in patients with atrophic nonunion of femoral shaft fractures
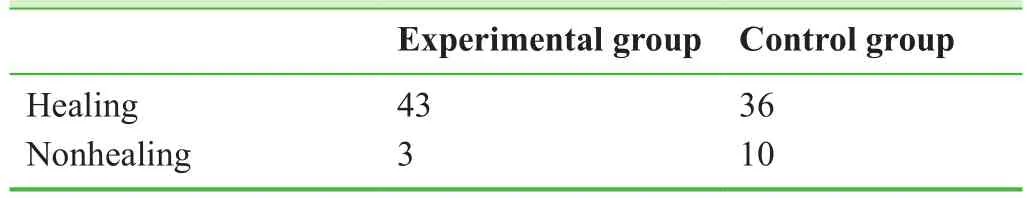
Table 5: Healing of atrophic nonunion of femoral shaft fractures after treatment with platelet-rich plasma
Postoperative complications: Infection occurred in one case in the experimental group and two cases in the control group. Rejection was not found in either group (Table 7).
Discussion
Significance of the study
The key points for the treatment of nonunion are to maintain the stability of the fracture ends, restore the blood supply, fill the bone defect, and promote osteogenesis.31We considered the use of PRP combined with conventional surgery. PRP can promote cell proliferation, cell differentiation, and matrix synthesis, and has effects on vascular regeneration and anti-infection.11,12PRP contributes to tissue healing and graft fusion, thus elevating the healing rate, shortening the treatment time, and mitigating the pain and costs.
Advantages and limitations of the study
The PRP used in the study was autologous, had no immunological rejection, was simply prepared, caused less damage to the body, released a large number of growth factors to promote fracture healing, and was limited to the fracture ends, thereby achieving the best synergistic effects.11The fibrin in PRP can provide support for tissue repair.11PRP contains a high concentration of leukocytes, which have local bacteriostatic and anti-in flammatory effects and can prevent infection.12
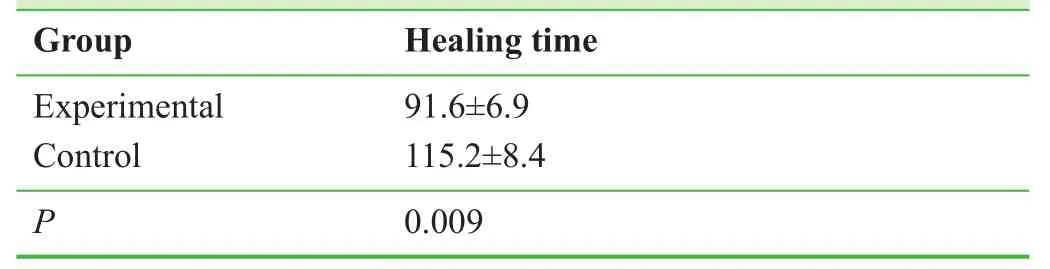
Table 6: Healing time (days) of atrophic nonunion of femoral shaft fractures after treatment with platelet-rich plasma
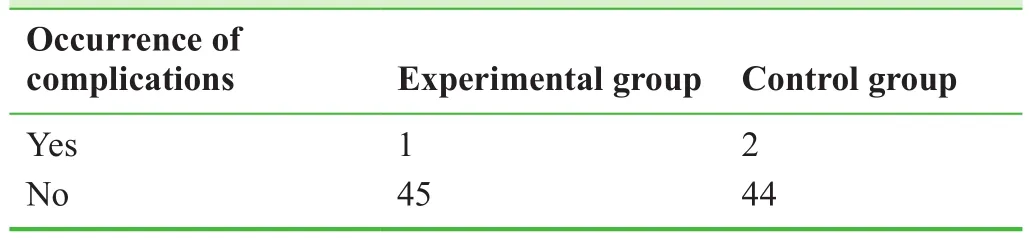
Table 7: Complications in patients with atrophic nonunion of femoral shaft fractures after treatment with plateletrich plasma
The Af filiated Hospital of Qinghai University of China is a third-class first-grade hospital, and has a good scienti fic research foundation. As a Qinghai First Aid Center, the Af filiated Hospital of Qinghai University has adequate traumatic cases and a good clinical basis for carrying out the trial. Our team has performed a study on PRP effectiveness in chronic osteomyelitis.32We have rich experience in the application of PRP and are skilled in the treatment of nonunion, both being conducive to smooth implementation of the study.
Evidence for contribution to future studies
As fracture healing is a multifactorial process, a single treatment cannot achieve satisfactory results. This study uses a combined method for the treatment of fracture healing, and provides an experimental basis for the clinical use of PRP in the treatment of atrophic nonunion.
Additional file
Additional file 1: SPIRIT checklist (PDF 48.0 kb).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
Patient selection, surgery, PRP preparation and injection, and manuscript writing: ZCZ and ZWL. Equipment preparation, patient management during hospitalization and follow-up: HXY, BMT,CLL and QFZ. Data collection and analysis: RR, PL and SLJ.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
1. Zhao ZC, Li ZW, Tang BM, Guo QF. Digital three-dimensional imaging models for repair of complex long bone fractures:study protocol for a randomized controlled trial with 6-month follow-up. Clin Transl Orthop. 2016;1:177-181.
2. Xu JJ. Safety and effectiveness of proximal femoral nail antirotation for the treatment of intertrochanteric femoral fracture:study protocol for a prospective case series. Clin Transl Orthop. 2016;1:90-99.
3. Yin PB, Long AH, Shen J, Tang PF. Treatment of intertrochanteric femoral fracture with proximal femoral medial sustainable intramedullary nails: study protocol for a randomized controlled trial. Clin Transl Orthop. 2016;1:44-50.
4. Tzioupis C, Giannoudis PV. Prevalence of long-bone non-unions.Injury. 2007;38 Suppl 2:S3-S9.
5. Milgram JW. Nonunion and pseudarthrosis of fracture healing.A histopathologic study of 95 human specimens. Clin Orthop Relat Res. 1991:203-213.
6. Frölke JP, Patka P. De finition and classi fication of fracture nonunions. Injury. 2007;38:S19-S22.
7. Weber BG. Treatment of juvenile fractures: general introduction(author's transl). Langenbecks Arch Chir. 1976;342:283-286.
8. Nyary T, Scammell BE. Principles of bone and joint injuries and their healing. Surgery. 2012;33:7-14.
9. Rodriguez-Merchan EC, Forriol F. Nonunion: general principles and experimental data. Clin Orthop Relat Res. 2004:4-12.
10. Rof fiA, Filardo G, Kon E, Marcacci M. Does PRP enhance bone integration with grafts, graft substitutes, or implants? A systematic review. BMC Musculoskel Disord. 2013;14:330-330.
11. Fernandes G, Yang S. Application of platelet-rich plasma with stem cells in bone and periodontal tissue engineering. Bone Res. 2016;4:16036.
12. Cohn CS, Lockhart E. Autologous platelet-rich plasma: evidence for clinical use. Curr Opin Hematol. 2015;22:527-532.
13. Assoian RK, Grotendorst GR, Miller DM, Sporn MB. Cellular transformation by coordinated action of three peptide growth factors from human platelets. Nature. 1984;309:804-806.
14. Zhang FT, Liu RW, Li H, Yu SF, Liu F, Sun XJ. Clinical observation of platelet- rich plasma combined with autogenous iliac in bone nonunion. Zhonghua Guanjie Waike Zazhi: Dianzi Ban.2016;10:598-603.
15. Yue Y, Paerhati·Rexiti, Wang Q, et al. Autologous platelet-rich plasma and autologous bone graft for comminuted fractures:randomized controlled follow-up. Zhongguo Zuzhi Gongcheng Yanjiu. 2014;18:3603-3608.
16. Xu HT, Zuo ZB, Zhuang J, et al. Application of autologous platelet rich glue combined with particulate of cancellous bone in the treatment of aseptic tibial nonunion. Zhongguo Jiaoxing Waike Zazhi. 2010;18:92-94.
17. Sun T, Wang JH, Luan JJ. Repair of bony defective nonunion of humeral condyle using autologous platelet rich-plasma combined with iliac autograft. Zhonghua Chuangshang Guke Zazhi. 2016;18:498-502.
18. Xu DZ, Wang YL, Kang HW. Platelet rich plasma combined with internal fixation by locking compression plate in the treatment of bone nonunion after surgery of long tubular bone fractures. Chuangshang Waike Zazhi. 2015;17:560,565.
19. Qiu JJ. Clinical Study of Improve Bone and Soft Repair with Platelet-Rich Plasma. Shanghai: Shanghai Jiao Tong University; 2009.
20. Jain A, Kumar S, Aggarwal AN, Jajodia N. Augmentation of bone healing in delayed and atrophic nonunion of fractures of long bones by partially decalci fied bone allograft (decal bone).Indian J Orthop. 2015;49:637-642.
21. Ebraheim NA, Buchanan GS, Liu X, et al. Treatment of distal femur nonunion following initial fixation with a lateral locking Plate. Orthop Surg. 2016;8:323-330.
22. Monroy A, Urruela A, Singh P, Tornetta P 3rd, Egol KA. Distal femur nonunion patients can expect good outcomes. J Knee Surg.2014;27:83-87.
23. Canadian Orthopaedic Trauma Society. Nonunion following intramedullary nailing of the femur with and without reaming.Results of a multicenter randomized clinical trial. J Bone Joint Surg Am. 2003;85-A:2093-2096.
24. Chen CE, Weng LH, Ko JY, Wang CJ. Management of nonunion associated with broken intramedullary nail of the femur. Orthopedics. 2008;31:78.
25. Rodriguez H, Ziran BH. Temporary antibiotic cement-covered gamma nail spacer for an infected nonunion of the proximal femur. Clin Orthop Relat Res. 2007;454:270-274.
26. Steinberg EL, Keynan O, Sternheim A, Drexler M, Luger E.Treatment of diaphyseal nonunion of the femur and tibia using an expandable nailing system. Injury. 2009;40:309-314.
27. Weng LH, Wang JW. Nonunion of the femur treated with conventional osteosynthesis combined with autogenous and strut allogeneic bone grafts. Chang Gung Med J. 2004;27:268-274.
28. Landesberg R, Roy M, Glickman RS. Quanti fication of growth factor levels using a simpli fied method of platelet-rich plasma gel preparation. J Oral Maxillofac Surg. 2000;58:297-300.
29. Wu MC, Wu ZD, Wu ZH. Surgery. Beijing: People's Medical Publishing House Co., Ltd.; 2013.
30. Langley GB, Sheppeard H. The visual analogue scale: its use in pain measurement. Rheumatol Int. 1985;5:145-148.
31. Schofer MD, Block JE, Aigner J, Schmelz A. Improved healing response in delayed unions of the tibia with low-intensity pulsed ultrasound: results of a randomized sham-controlled trial. BMC Musculoskel Disord. 2010;11:229-229.
32. Tang BM, Yang AR, Li ZW, Zhao ZC, Li CL. The clinical research of the chronic osteomyelitis’ nonunion wound treated by platelet-rich plasma. Qinghai Yiyao Zazhi. 2016;46:2-6.
 Clinical Trials in Orthopedic Disorder2017年2期
Clinical Trials in Orthopedic Disorder2017年2期
- Clinical Trials in Orthopedic Disorder的其它文章
- Efficacy of endoscopic transantral versus transorbital surgical approaches in the repair of orbital blowout fractures: study protocol for a randomized controlled trial
- Effects of lumbar plexus-sciatic nerve block combined with sevoflurane on cognitive function in elderly patients after hip arthroplasty: study protocol for a prospective, single-center,open-label, randomized, controlled clinical trial
- Effects of two different tranexamic acid administration methods on perioperative blood loss in total hip arthroplasty: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Supercapsular percutaneously-assisted total hip approach for the elderly with femoral neck fractures: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Should angiography be done in suspected tuberculosis of spine in an endemic country? – Hemangioma masquerading as tuberculosis of spine
