Should angiography be done in suspected tuberculosis of spine in an endemic country? – Hemangioma masquerading as tuberculosis of spine
Vishal Kumar, Avinash Kumar*, Sarvdeep S. Dhatt, Raj Bahadur
Post Graduate Institute of Medical Education and Research, Chandigarh, India
Introduction
Vertebral hemangiomas constitute 2–4% of benign spinal tumors. It usually involves the vertebral body while posterior elements are involved in only 10–15% of cases.1,2They are present in about 14% of the population at autopsy.3Laredo et al.4has divided vertebral haemangiomas into three categories according to the mode of presentations.First is the asymptomatic group in which it is detected incidentally. Second is the group of patients presenting with features of myelopathy, radiculopathy or cauda equina syndrome due to compression of the spinal cord, nerve root, and cauda equina, respectively. Third is the group of patients presenting with axial pain due to vertebral haemangioma with or without associated vertebral body fracture. Several characteristic radiological features like“jail-house” or “corduroy” appearance in X-ray, “polka-dot”appearance on axial computed tomography (CT) scan,have been described for vertebral body hemangiomas.5Magnetic resonance imaging (MRI) is the standard for diagnosing vertebral hemangiomas presenting with compressive symptoms and usually shows hyperintensity on both T1- and T2-weighted sequences.6However, there are case reports suggesting these lesions to mimick other more commonly diagnosed lesions of the spine both clinically and radiologically, apart from hemangiomas.7,8We are reporting a case of vertebral body haemangioma in dorsal spine mimicking tuberculosis. The importance of this case report lies in the fact that in endemic country,patients with typical clinical features of tuberculosis of spine, the diagnosis of tuberculosis cannot be neglected in the absence of biopsy specially when there is also severe neurological de ficit to the patient; and then a dilemma of the diagnosis may be encountered.
Case Report
A 50-year-old female patient presented to the outpatient department with complaints of inability to walk, decreased sensation in both lower limbs and retention of urine for past 3 months. She also had complaints of loss of appetite and weight recently. She received anti-tuberculous chemotherapy during the last 2 months, but without any relief. On examination she had deep tenderness over upper dorsal spine, muscle strength grade 0 assessed using the Medical Research Council (MRC) scale9in all lower limb muscle groups, decreased sensation below D6 vertebral level dermatome, involvement of bladder and bowel, bilateral positive Babinski re flex and presence of exaggerated deep tendon re flexes and clonus in bilateral lower limbs. This study was approved by the local ethics committee. An informed written consent from the patient for all the necessary investigations, interventions and the surgeries was obtained after proper explanation.Plain radiographs showed decreased density of fourth and fifth dorsal vertebrae with decreased disc space and associated soft-tissue mass apparently (Figure 1). MRI showed altered signal intensity in D4 and D5 vertebrae with end plate destruction and involvement of intervening disc. There was associated large bilateral soft-tissue mass suggestive of abscess (Figure 2). A clinico-radiological diagnosis of tuberculosis was made on the basis of compressive myelopathy and suspected radiographic features though without biopsy because of endemicity of the disease and similar clinicoradiological features. The patient was transferred to operating room for open biopsy,decompression, and fixation through anterior (transthoracic periscapular) approach. Patient was positioned in the right lateral position on the operating table and the fourth rib was cut and profuse bleeding was encountered, and therefore only biopsy specimens from the vertebral body was taken and the planned procedure was abandoned.

Figure 1: Anteroposterior radiograph of the dorsal spine showing end plate destruction of D4 and D5 vertebrae (red arrow) with an apparent soft tissue swelling around.
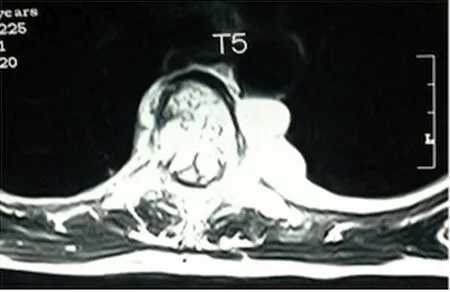
Figure 2: Axial section of magnetic resonance imaging of D5 (T5)showing enhanced signal intensity in the body, in the spinal canal and around the vertebra suggestive of an abscess.
A mixed capillary and venous haemangioma involving D4 and D5 vertebrae was revealed by a histopathological report. Computed tomography angiography showed a number of large vessels supplying the tumor (Figure 3).After discussion with the interventional radiologist, a plan of decompression and fixation was made after preoperative embolization. Patient was taken for digital subtraction angiography (DSA) procedure room for embolization again.After that she was re-operated and an anterior decompression (corpectomy) with pedicle screw and cage fixation was performed (Figure 4). The patient was prescribed intravenous antibiotics for 10 days and pregabalin and methylcobalamin tablets at night for 1 month. She was allowed to mobilize the next day after surgery when she could tolerate pain; first in the wheel chair. One week after surgery, the patient had MRC grade 4 power in all lower limb muscle groups and then she was allowed to walk first with support. The patient was discharged after the suture removal and was allowed to mobilize. The use of walking aid was advised as per her balance. She started walking of her own after 15 days.
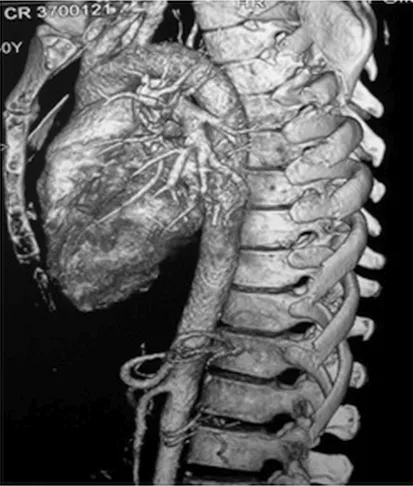
Figure 3: Computed tomography angiogram showing large feeding vessel to the affected vertebral lesion.
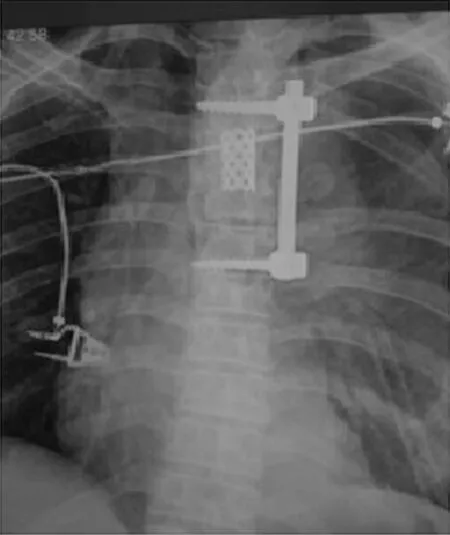
Figure 4: Immediate postoperative anteroposterior radiograph of dorsal spine after corpectomy decompression and fixation with pedicle screws and a cage.
At 6 months of follow-up, the patient came to the clinic walking and was symptom free. The neurological status at that time was MRC grade 5. The last follow-up was at 14 months and the patient was pain free (Denis pain scale10score 1) without any neuropathic pain or signs of upper motor neuron disease.
Discussion
In India, the most common cause of extradural compressive myelopathy is tuberculosis.11The appearances of classical radiographic findings in case of tuberculosis may be observed 5 months after onset,12,13thus posing diagnostic dilemma in early stages of the disease on the basis of radiographs only. Being an endemic country for this disease,most cases of tuberculous paraplegia can be diagnosed con fidently on the basis of clinical and radiological features with preoperative biopsy. When the patients do not respond to the chemotherapy even after 1 month, the suspicion of multidrug resistance tuberculosis comes as a first diagnosis which can be con firmed from the specimen culture obtained intraoperatively; because the prevalence of multidrug resistance in Mycobacterium tuberculosis is estimated at more than 15% and is believed to be increasing manifold especially in a endemic country.12The chances of isolating the organism in Fine Needle Aspiration Cytology specimens can be as less as 10% due to its paucibacillary nature.13Vertebral body hemangiomas on the other hand are usually asymptomatic and rarely cause paraplegia. Their usual location is in lower dorsal or upper lumbar spine. Radiological features described to indicate an aggressive haemangioma potentially causing features of neural compression include location in D3 to D9 region, involvement of entire vertebral body, involvement of the neural arch (the pedicles particularly), irregular trabecular appearance, expanded and poorly de fined cortex of the vertebral body, and soft-tissue swelling.14In retrospective analysis, some of these features were also present in our patient. But in the context of associated typical constitutional symptoms, a diagnosis of tuberculosis was made. The usual protocol in our institute for a case of clinico-radiologically suspected spinal tuberculosis is to start the patient on anti-tuberculous chemotherapy and if no clinical response is there after waiting for a reasonable period of time, surgical intervention is done in the form of debridement with or without fixation. Open biopsy is taken at the time of surgery. Treatment options in a case of symptomatic vertebral haemangioma include radiotherapy, embolization, vertebroplasty and surgical decompression with pre-operative embolization being used as an adjunct increasingly.15In the present case, considering the high vascularity, the greater extent of involvement and the associated neurological de ficit, embolization followed by anterior decompression was a reasonable option, as advocated by other researchers.16,17For the purpose of embolization, it is important to get digital substraction angiography done, to delineate the feeding vessels of the lesion, which need to be embolized.
Conclusion
Tuberculosis, though the most common entity producing extradural compressive myelopathy in this part of the world should not be a casual diagnosis and proper history taking,clinical examination and evaluation of radiological features are mandatory in all cases suspected of having the disease.The diagnostic digital substraction angiography in such a diagnostic dilemmatic case may be a good preoperative planning tool for helping us to make correct diagnosis and even if it turns out to be a case of tuberculosis, the test will also help in knowing the vascularity around the operating region.Vertebral body haemangioma, though a rare cause of cord compression, should be kept in the differential diagnoses in such cases to avoid unforeseeable complications during further course of treatment.
Declaration of patient consent
The authors certify that they have obtained the appropriate patient consent form. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal her identity,but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
Concept, design, de finition of intellectual content, data acquisition, manuscript editing, manuscript review: VK. Data analysis,concept, design, manuscript preparation, manuscript editing, literature search: AK. Data analysis, de finition of intellectual content,manuscript editing, manuscript review, performed the surgery:SSD. Data acquisition, concept, de finition of intellectual content,manuscript review, performed the surgery: RB.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
1 Aksu G, Saynak M, Karadeniz A. Spinal Cord compression due to vertebral hemangioma. Orthopedics. 2008;31:169.
2. Osborn AG. Tumors, cysts and tumor like lesions of the spine and spinal cord. In: Anne G, ed. Diagnostic Neuroradiology. St Louis: Mosby; 1994:876-918.
3. Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993;78:36-45.
4. Laredo JD, Assouline E, Gelbert F, Wybier M, Merland JJ,Tubiana JM. Vertebral hemangiomas: fat content as a sign of ag gressiveness. Radiology. 1990;177:467-472.
5. Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral heman giomas: Radiologic evaluation. Radiology. 1986;161:183-189.
6. Ross JS, Masaryk TJ, Modic MT. Vertebral hemangiomas: MR imaging. Radiology. 1987;165:165-167.
7. Sainani NI, Pungavkar SA, Patkar DP. Multiple hemangiomas involving the vertebral column. Acta Radiol. 2005;46:510-513.
8. Kulshrestha M, Byrne P. Multiple primary haemangiomas of bone mimicking vertebral metastases. J R Soc Med. 1997;90:632-634.
9. Frese E, Brown M, Norton BJ. Clinical reliability of manual muscle testing. Middle trapezius and gluteus medius muscles.Phys Ther. 1987;67:1072-1076.
10. Denis F, Armstrng G, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic de ficit; a comparison between operative and non-operative treatment. Clin Orthop Relat Res. 1984;189:142-149.
11. Jain AK, Rajasekaran S. Tuberculosis of spine. Indian J Orthop.2012;46:127-129.
12. Tuli SM. Challenge of therapeutically refractory and multidrug resistant tuberculosis in orthopaedic practice. Indian J Orthop.2002;36:211-213.
13. Jain AK. Tuberculosis of the spine:A fresh look at an old disease. J Bone Joint Surg Br. 2010;92-B:905-913.
14. Hsu W, Kosztowski TA, Zaidi HA. Multidisciplinary management of primary tumors of the vertebral column. Curr Treat Options Oncol. 2009;10:107-125.
15. Bandiera S, Gasbarrini A, De lure F. Symptomatic vertebral hemangiomas: the treatment of 23 cases and review of the lit erature. Chir Organi Mov. 2002;87:1-15.
16. Acosta FL Jr, Dowd CF, Chin C, Tihan T, Ames CP, Weinstein PR. Current treatment strategies and outcomes in the manage ment of symptomatic vertebral hemangiomas. Neurosurgery.2006;58:287-295.
17. Nair AP, Kumar R, Srivastav AK, Sahu RN, Kumar B. Outcome of dorsolumbar vertebral hemangiomas presenting with neuraxial compression. Indian J Orthop. 2012;46:536-541.
 Clinical Trials in Orthopedic Disorder2017年2期
Clinical Trials in Orthopedic Disorder2017年2期
- Clinical Trials in Orthopedic Disorder的其它文章
- Efficacy of endoscopic transantral versus transorbital surgical approaches in the repair of orbital blowout fractures: study protocol for a randomized controlled trial
- Platelet-rich plasma combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures: study protocol for a prospective, randomized, controlled clinical trial
- Effects of lumbar plexus-sciatic nerve block combined with sevoflurane on cognitive function in elderly patients after hip arthroplasty: study protocol for a prospective, single-center,open-label, randomized, controlled clinical trial
- Effects of two different tranexamic acid administration methods on perioperative blood loss in total hip arthroplasty: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Supercapsular percutaneously-assisted total hip approach for the elderly with femoral neck fractures: study protocol for a prospective, open-label, randomized, controlled clinical trial
