Effects of lumbar plexus-sciatic nerve block combined with sevoflurane on cognitive function in elderly patients after hip arthroplasty: study protocol for a prospective, single-center,open-label, randomized, controlled clinical trial
Yan-hong Guo, Liang-de A*, Zhen Jia
Department of Anesthesiology, Affiliated Hospital, Qinghai University, Xining, Qinghai Province, China
Introduction
History and current related studies
Elderly patients frequently experience postoperative cognitive dysfunction (POCD) after total hip arthroplasty,resulting in disorders of brain function, including memory,concentration, perception and behavioral disorders.1-5Postoperative cognitive dysfunction is often transient, and can be effectively controlled if measures are taken promptly. If POCD is not addressed in a timely fashion it can become permanent, which may greatly impair the patient’s quality of life.6At present, the pathogenesis of POCD in elderly patients undergoing hip arthroplasty, and the optimum treatment strategies, are not known.
Combined lumbar plexus and sciatic nerve block achieves complete unilateral limb anesthesia, and are facilitated by using a nerve stimulator to identify correct needle position. The block has little in fluence on hemodynamic status, but can reportedly suppress the stress response to surgery, reduce postoperative pain intensity and reduce the risk of POCD.7Basic fibroblast growth factor (bFGF) has been shown to in fluence cognitive function,8-12and decreased bFGF concentration can directly affect the function of nerve cells and impair cognitive ability.8-12Sevo flurane combined with dexmedetomidine can decrease the incidence of POCD in elderly patients after thoracic surgery13; however, whether sevo flurane can reduce the incidence of POCD after hip arthroplasty has not been reported.
Main objective
We hypothesized that lumbar plexus-sciatic nerve block combined with sevo flurane would reduce the incidence of cognitive dysfunction in elderly patients after hip arthroplasty. We designed a study to test this hypothesis.
Methods/Design
Study design
A prospective, single-center, open-label, randomized, controlled clinical trial.
Study setting
Af filiated Hospital of Qinghai University, Xining, Qinghai Province, China.
Study procedures
Seventy elderly patients undergoing unilateral total hip arthroplasty at the Af filiated Hospital of Qinghai University were randomized into two groups. All patients underwent endotracheal intubation, mechanical ventilation and general anesthesia. The experimental group first underwent a lumbar plexus-sciatic nerve block, after which anesthesia was maintained with sevo flurane (Appendix 1). In the control group, general anesthesia was maintained with intravenous propofol. Patients were subjected to a preoperative assessment, and were followed-up 1 and 3 days after surgery(Figure 1).
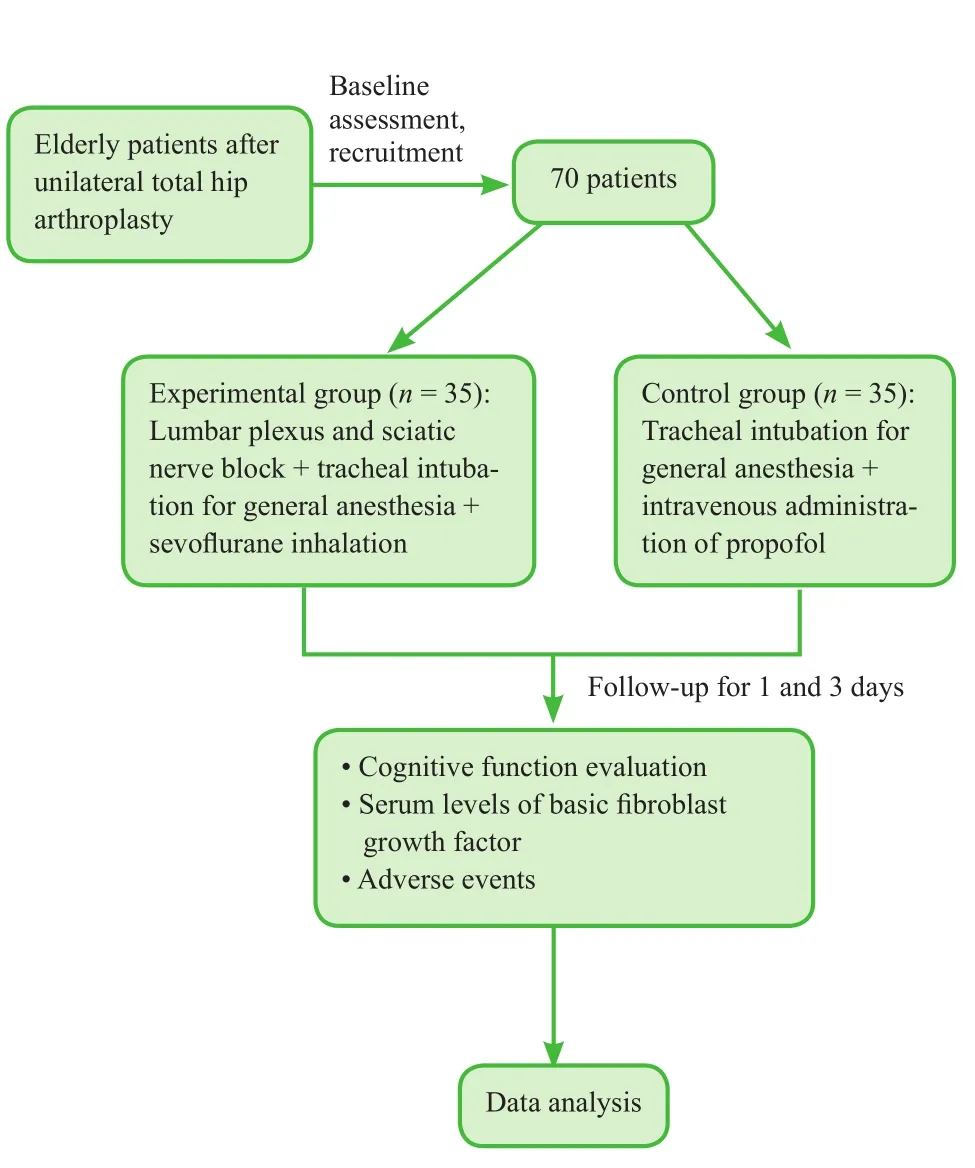
Figure 1: Flow chart of the trial protocol.
The Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) are commonly used to assess cognitive function. The scores of both are reliable and reproducible, and have been widely validated.14We elected to use MMSE and MoCA to evaluate POCD.
Subjects were recruited from July 2012 to December 2014.
Inclusion criteria
Patients who met all the following criteria were considered for study inclusion:
· Age: 60–70 years
· American Society of Anesthesiologists (ASA) physical status classi fication: Class II or III
· Scheduled for unilateral hip arthroplasty
· Educational level: junior high school or above; no cognitive dysfunction before surgery
· First surgical treatment for osteoarthritis of the hip
· Provision of written, informed consent by the patient and their family
Exclusion criteria
Patients ful filling any of the following criteria were excluded from the trial:
· Existing central or peripheral nervous system disease or psychosis
· Allergy to anesthesia
· Poor compliance with study protocols
· Cardiovascular disease, or severe primary liver or renal disease
· Other diseases impairing cognitive function
Baseline analysis
Patients’ baseline demographic and clinical characteristics are shown in Table 1.
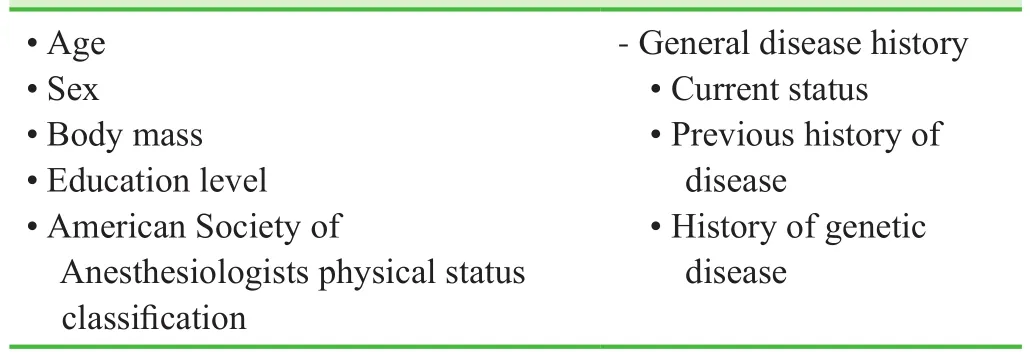
Table 1: Baseline data and general disease history of enrolled patients
Sample size calculation
We judged that MMSE score would have fallen by 2.5 and 4.5 in the experimental and control groups, respectively,by the 3rdpostoperative day. The standard deviation of the MMSE score was 3.0. Taking β = 0.1 and power = 90%with a signi ficance level of α = 0.05, the final effective sample size of n = 49 per group was calculated using PASS 11.0 software (NCSS, Kaysville, UT, USA). Assuming a drop-out rate of 20%, we would therefore require 59 patients per group. We therefore aimed to include 35 patients in the experimental group and 35 patients in the control group, according to the inclusion and exclusion criteria.
Recruitment
Information lea flets were sent to outpatients or hospitalized patients undergoing treatment for osteoarthritis of the hip at the Af filiated Hospital of Qinghai University of China. The lea flet gave details of the study objectives.Patients were given the project leader’s contact details.After providing informed consent, potential participants successfully screened against the inclusion and exclusion criteria were enrolled.
Randomization and blinding
Patients were assigned a number and randomized into two groups using a random number table. This was an open-label trial. Patients, physicians and assessors were not blinded to randomization status or the therapeutic regimen.
Intervention
Preoperative preparation
All patients were fasted before surgery. Heart rate, peripheral oxygen saturation and electrocardiogram were monitored after entering the operating room. Invasive arterial blood pressure was monitored via an arterial catheter placed in the contralateral radial artery under local anesthetic.
Intraoperative anesthesia
Control group: General anesthesia was induced with intravenous midazolam 0.02 mg/kg, sufentanil 0.3 μg/kg and rocuronium bromide 0.6 mg/kg. An intravenous propofol infusion was used for maintenance of anesthesia.
Experimental group: The lumbar plexus and sciatic nerve block was performed using a nerve stimulator needle (B. Braun Medical Inc., Melsungen, Germany). The initial stimulus settings were: frequency 1 Hz, intensity 1 mA and pulse duration 0.1 ms. Lumbar plexus block:the patient was positioned in the lateral position with the hips and knees flexed and the affected side superior. The spinous processes were identi fied in the midline, and a line parallel to the midline was drawn through the posterior superior iliac spine. A perpendicular line was drawn between the parallel lines at the level of the L4spinous process.The lateral third of the perpendicular line was used as the entry point. The needle was inserted and advanced until regular contraction of quadriceps femoris was observed.Current intensity was gradually reduced to 0.25–0.35 mA, and, if twitching was sustained, approximately 25 mL 0.4% ropivacaine was slowly injected in the absence of blood or cerebrospinal fluid during aspiration. Sciatic nerve block: The nerve stimulator and needle were used in the same way to identify gastrocnemius contraction,and approximately 25 mL 0.4% ropivacaine was injected. Sensory and motor hypofunction in the expected distribution was con firmed 20 minutes later. Induction of anesthesia was then undertaken in the same way as the control group, but 2% sevo flurane (oxygen flow rate 2 L/min; Maruishi, Japan) was used for maintenance.Postoperatively, patient-controlled intravenous analgesia was given in both groups.
Hip arthroplasty
The hip arthroplasty was conducted by the same group of surgeons. A large-diameter metal-on-metal total hip prosthesis was used. Through a posterolateral approach, the hip joint was completely exposed and the femoral head excised approximately 1 cm above the calcar femorale.After fully exposing the acetabulum, excessive osteo-phytes were removed. After moderately deepening the acetabulum, an acetabular prosthesis was inserted in 45°valgus and 20° anteversion. Appropriately-sized Corail or Summit femoral stems were used (Depuy, Warsaw,IN, USA). A femoral head prosthesis, whose diameter is 5 mm smaller than the diameter of the acetabular cup,was paired with an acetabular cup of outer diameter <52 mm. A femoral head prosthesis, whose diameter is 6 mm smaller than the diameter of the acetabular cup, was paired with an acetabular cup of outer diameter 52 mm. A femoral head prosthesis, whose diameter is 7 mm smaller than the diameter of the acetabular cup, was paired with an acetabular cup of outer diameter > 52 mm. Bone debris was removed from the acetabular prosthesis, the femoral head was placed in the acetabulum and the range of motion of the hip was checked. A surgical drain was placed and the incision closed layer by layer by suturing.
Measurement of serum bFGF concentration
Preoperatively, and 1 day and 3 days postoperatively, a sample of approximately 3 mL fasting venous blood was collected from all patients, stored at room temperature for 30 minutes, then centrifuged. Serum was collected and stored at −20°C. An enzyme linked immunosorbent assay was used to measure serum bFGF concentration with a bFGF kit (Bei Nuo Life Science, Shanghai, China) according to the manufacturer’s instructions.
Outcome measures
Primary outcome measure
The primary outcome was MMSE, measured preoperatively,and 1 day and 3 days postoperatively. The MMSE items include memory, attention and calculation ability, orientation, recall ability and language skill. The score ranges from 0–30. An MMSE score < 25 is considered to represent cognitive d ysfunction. All MMSE tests were performed by the same experienced attending physician in psychologically stable patients.
Secondary outcome measures
We also measured MoCA preoperatively, and 1 day and 3 days postoperatively. The MoCA items include execution and visual space function, language concentration, attention, naming, delayed recall, abstract thinking and orientation. The score ranges from 0–30. A MoCA score < 26 is considered to represent cognitive dysfunction. All MoCA tests were performed by the same experienced attending physician in psychologically stable patients.
Serum bFGF concentration: bFGF is a biochemical marker of nervous system injury. A substantially decreased bFGF concentration after anesthesia is associated with POCD.
Intraoperative blood loss: Lower blood loss indicates a high quality of surgery.
Operation time: A shorter operation time indicates that the operation is progressing well.
Other outcome measures
We also recorded adverse events intraoperatively, and 1 day and 3 days postoperatively. We calculated the incidence of adverse events as the proportion of patients who experienced an adverse event from the total number of patients,and expressed it as a percentage.
The schedule of outcome measurement assessments is shown in Table 2.
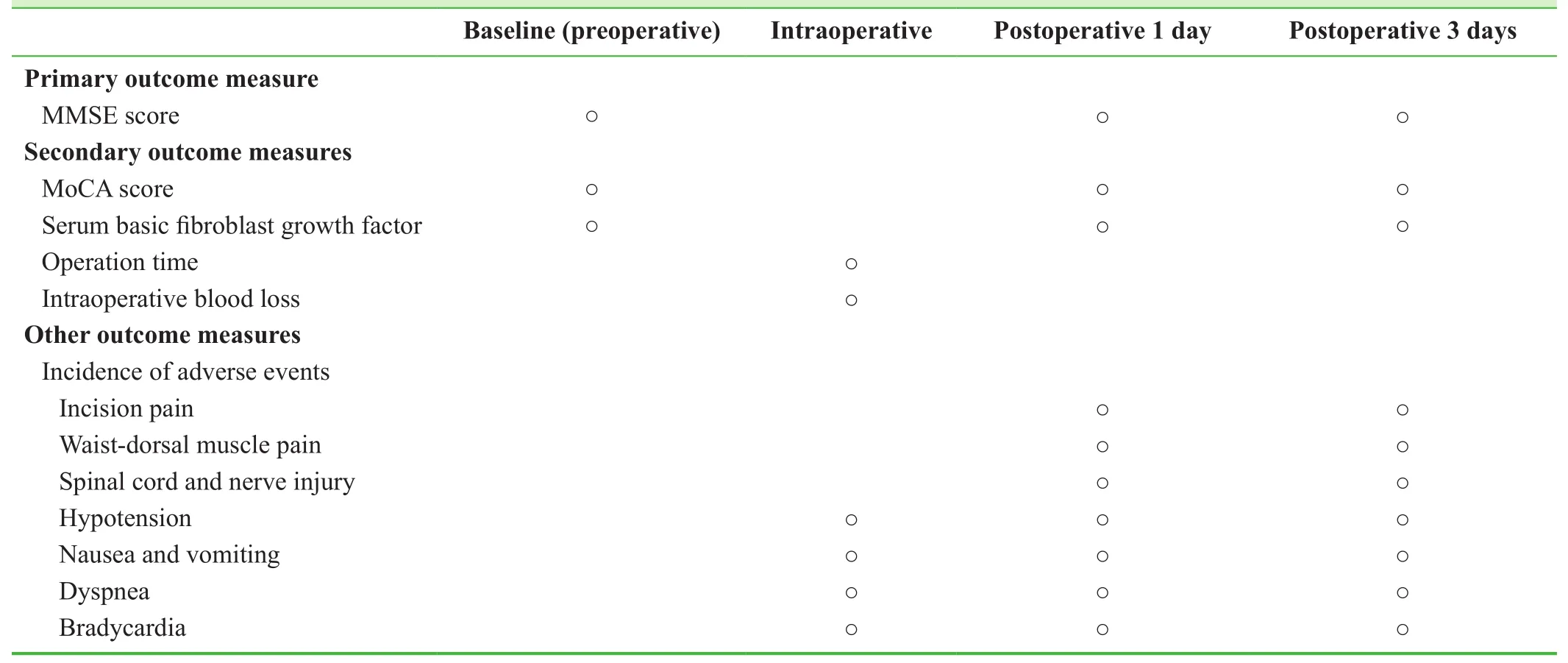
Table 2: Timing of outcome assessment
Adverse events
We recorded adverse events, including postoperative pain,spinal cord or nerve injury, hypotension, nausea and vomiting, dyspnea and bradycardia.
For severe adverse events, investigators reported the details-including the date of occurrence and treatment measures-to the principal investigator and the institutional review board within 24 hours.
Data collection, management, analysis and open access
Data collection: Case report forms were collected, processed using Epidata software (Epidata Association, Odense, Denmark), collated and then recorded electronically by data managers using a double-data entry strategy.
Data management: The locked electronic database was accessible only by the project manager. This arrangement will not be altered. The Af filiated Hospital of Qinghai University, China will preserve all trial data forever.
Data analysis: A professional statistician was employed to analyze the data, and compiled an outcome analysis report that was submitted to the lead researchers. An independent data monitoring committee supervised and managed the trial data, ensuring a scienti fic and stringent trial that yielded accurate and complete data.
Data open access: Anonymized trial data were published at www. figshare.com.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 software(IBM, Armonk, NY, USA) and followed the intention-totreat principle.
Measurement data were normally distributed, and are expressed as the mean ± standard deviation. Frequency data are expressed as the constituent ratio or rate.
Comparisons of the serum bFGF concentration, MMSE score and MoCA score between groups were made using a two-sample t-test. Within-group changes in each of the parameters at the three time points were assessed using repeated measures analysis of variance. The incidence of adverse events in both groups was compared using Pearson’s χ2test.
The correlation between serum bFGF concentration and cognitive function was analyzed using Pearson correlation analysis.
The signi ficance level was α = 0.05.
Trial Status
Recruitment and the clinical trial have been completed at the time of submission; data analysis is ongoing. Provisional findings are as follows.
Comparison of baseline data, operation time and intraoperative blood loss
Sex, age, body mass index, educational level, ASA physical status classi fication, operation time, blood loss and complications were not signi ficantly different between the two groups (P > 0.05 for all analyses; Table 3).
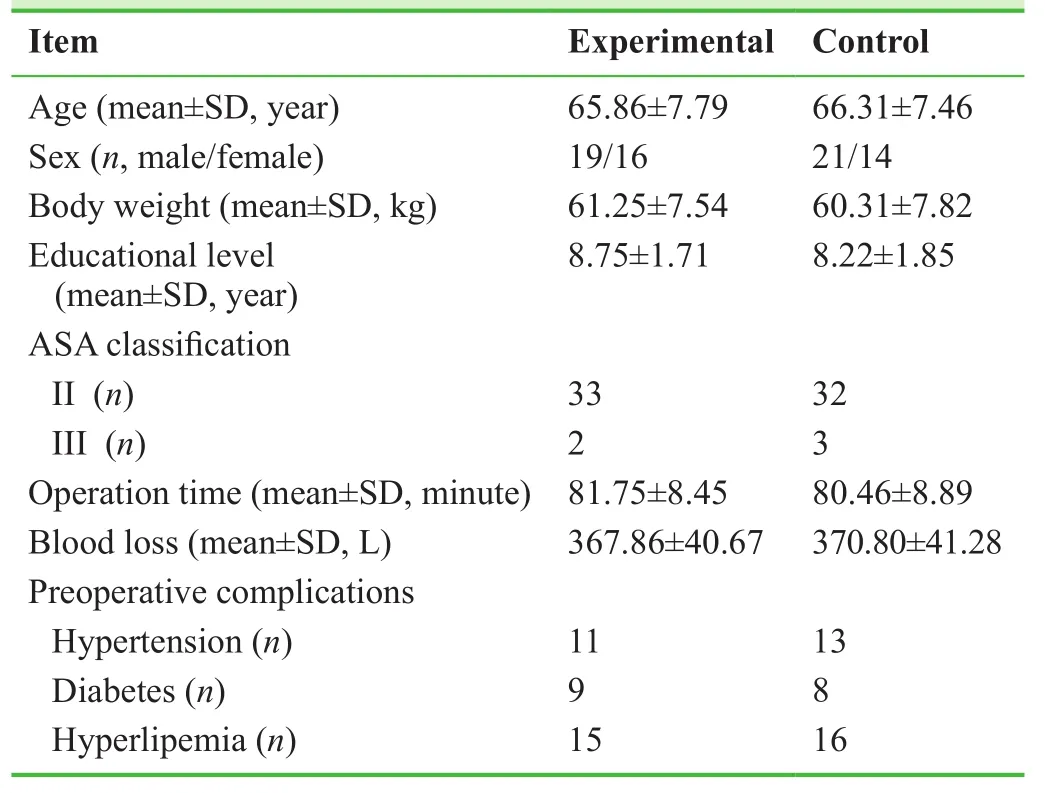
Table 3: Comparison of baseline data, duration of surgery and intraoperative blood loss in the study groups
Comparison of MMSE score and MoCA score
MMSE and MoCA scores were signi ficantly lower at 1 day and 3 days postoperatively in both groups (P < 0.05 and P < 0.01, respectively); MMSE and MoCA scores were signi ficantly higher in the experimental group than in the control group 1 day and 3 days postoperatively (P < 0.01 for both analyses; Table 4).
Changes in serum bFGF concentration
Serum bFGF concentration was signi ficantly lower 1 day and 3 days postoperatively in both groups (P < 0.05 and P < 0.01, respectively). Serum bFGF concentration was signi ficantly higher in the experimental group than in the control group 1 day and 3 days postoperatively (P < 0.01 for both analyses; Table 5).
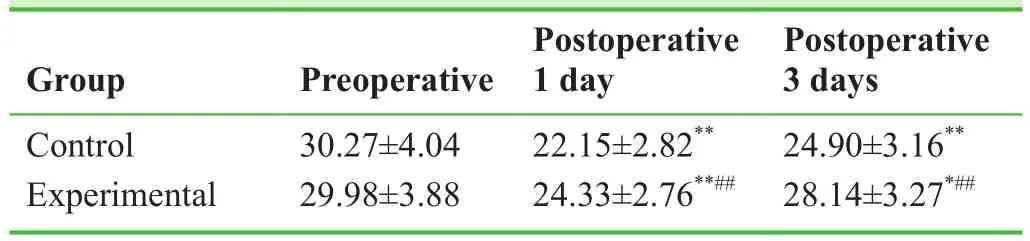
Table 5: Comparison of serum basic fibroblast growth factor concentration (pg/mL) in the study groups
Correlation between serum bFGF concentration and cognitive function
The changes in serum bFGF concentration were positively correlated with MMSE and MoCA scores, with correlation coef ficients (r) of 0.52 and 0.49, respectively (P < 0.01 for both analyses).
Comparison of the incidence of adverse events between the groups
On the first postoperative day, two patients suffered from nausea and vomiting, and two patients experienced respiratory depression in the experimental group; the incidence of adverse events was 11.4%. In the control group, five patients had nausea and vomiting, and eight had respiratory depression; the incidence of adverse events was 37.1%.Hypotension or bradycardia was not observed in either group. The incidence of adverse events was signi ficantly lower in the experimental group than in the control group(P < 0.01; Table 6).
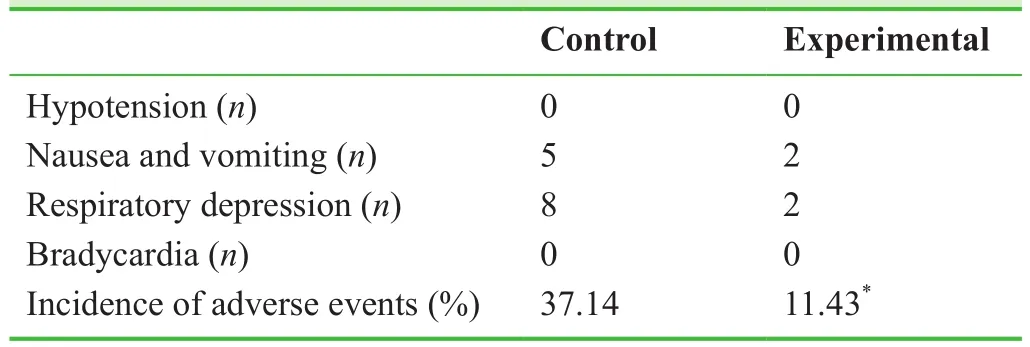
Table 6: Comparison of the incidence of adverse events in both groups at postoperative 1 day
Discussion
Significance of this study
Compared with other analgesic and anesthetic drugs, the incidence of POCD is reportedly lower after sevo flurane anesthesia, and patients recover from anesthesia more rapidly.15We elected to examine the in fluence of lumbar plexus and sciatic nerve block and sevo flurane anesthesia.We found that this combination reduced the incidence of POCD and adverse events compared with intravenous anesthesia with propofol.
Limitations of this study
The small sample size and lack of long-term follow-up results will likely affect the accuracy and reliability of the results.16-18
Evidence for contribution to future studies
This study will expand the evidence base that sevo flurane,combined with lumbar plexus-sciatic nerve block protects cognitive function in elderly patients after total hip arthroplasty, and reduces the incidence of POCD.
Appendix 1 Sevoflurane description
(1) Sevo flurane is a clear, colorless liquid containing no additives. Sevo flurane is not corrosive to stainless steel,brass, aluminum, nickel-plated brass, chrome-plated brass or copper beryllium. Sevo flurane is non-pungent. It is miscible with ethanol, ether, chloroform and benzene, and it is slightly soluble in water.
(2) Sevo flurane is stable when stored at room temperature according to the manufacturer’s instructions. No discernible degradation of sevo flurane occurs in the presence of strong acids or heat. When in contact with alkaline CO2absorbents(e.g. Baralyme®and to a lesser extent soda lime) within the anesthesia machine, sevo flurane can undergo degradation under certain conditions. Degradation of sevo flurane is minimal, and degradants are either undetectable or present in non-toxic amounts when used as directed with fresh absorbents.
(3) Sevo flurane degradation and subsequent degradant formation are enhanced by increasing absorbent temperature, increased sevo flurane concentration, decreased fresh gas flow and desiccated CO2absorbents (especially with potassium hydroxide containing absorbents, e.g. Baralyme®).
(4) Sevo flurane is an inhalational anesthetic agent for use in the induction and maintenance of general anesthesia. The minimum alveolar concentration of sevo flurane in oxygen for a 40-year-old adult is 2.1%. The minimum alveolar concentration of sevo flurane decreases with age.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
Study concept and design, drafting of the manuscript: YHG. Data processing: LDA. Critical revision of the manuscript, approval of the final version: ZJ.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
1. Goettel N, Burkhart CS, Rossi A, et al. Associations between impaired cerebral blood flow autoregulation, cerebral oxygenation, and biomarkers of brain injury and postoperative cognitive dysfunction in elderly patients after major noncardiac surgery.Anesth Analg. 2017. doi: 10.1213/ANE.0000000000001803.
2. Hilmani S, Houass Y, El Azhari A. Paraventricular meningioma revealed by mental disorder. Surg Neurol Int. 2016;7:S1004-1007.
3. Yu P, Wang H, Mu L, Ding X, Ding W. Effect of general anesthesia on serum β-amyloid protein and regional cerebral oxygen saturation of elderly patients after subtotal gastrectomy.Exp Ther Med. 2016;12:3561-3566.
4. Grocott HP. Postoperative cognitive dysfunction and low regional cerebral oxygen saturation: is this relationship fragile or fractured altogether? Anesth Analg. 2017;124:697-698.
5. Wu XM, Xu WC, Yu YJ, Han L, Zhang J, Yang LJ. Postoperative serum thioredoxin concentrations correlate with delirium and cognitive dysfunction after hip fracture surgery in elderly patients. Clin Chim Acta. 2017;466:93-97.
6. Benson RA, Ozdemir BA, Matthews D, Loftus IM. A systematic review of postoperative cognitive decline following open and endovascular aortic aneurysm surgery. Ann R Coll Surg Engl.2017. doi: 10.1308/rcsann.2016.0338.
7. Gong CS, Zhao RG, Yu ZG, Chen YQ. The impacts of lumbar plexus block combined with sciatic nerve block on postoperative cognitive function and plasma S100β in eldly patients undergoing hip surgeries. Linchuang Mazuixue Zazhi.2014;30:1172-1174.
8. Wang Q, Song YH, Tang Z, Wang ZP, Xu Q, Bao N. Effects of ganglioside GM1 and neural growth factor on neural stem cell proliferation and differentiation. Genet Mol Res. 2016. doi:10.4238/gmr.15038376.
9. Rusanescu G, Mao J. Immature spinal cord neurons are dynamic regulators of adult nociceptive sensitivity. J Cell Mol Med.2015;19:2352-2364.
10. Zhang W, Zhu X, Liu Y, et al. Nur77 was essential for neurite outgrowth and involved in schwann cell differentiation after sciatic nerve injury. J Mol Neurosci. 2015;57:38-47.
11. Ren M, Deng X, Guo Y, Zheng F, Feng Z. Effect of basic fibroblast growth factor on endogenous neural stem cell in rat cerebral cortex with global cerebral ischemia-reperfusion. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2014;31:846-849.
12. Nascimento CM, Pereira JR, de Andrade LP, et al. Physical exercise in MCI elderly promotes reduction of pro-in flammatory cytokines and improvements on cognition and BDNF peripheral levels. Curr Alzheimer Res. 2014;11:799-805.
13. Zhu J. Effects of sevo flurane combined dexmedetomidine for early cognitive function in elderly patients after thoracic surgery. Zhongguo Laonianxue Zazhi. 2015;35:2120-2122.
14. Hollis AM, Duncanson H, Kapust LR, Xi PM, O'Connor MG.Validity of the mini-mental state examination and the montreal cognitive assessment in the prediction of driving test outcome.J Am Geriatr Soc. 2015;63:988-992.
15. Dube SK, Pandia MP, Chaturvedi A, et al. Comparison of intraoperative brain condition, hemodynamics and postoperative recovery between des flurane and sevo flurane in patients undergoing supratentorial craniotomy. Saudi J Anaesth. 2015;9:167-173.
16. Yin PB, Long AH, Shen J, et al. Treatment of intertrochanteric femoral fracture with proximal femoral medial sustainable intramedullary nails: study protocol for a randomized controlled trial. Clin Transl Orthop. 2016;1:44-50.
17. Wu T, Zhang GQ. Minimally invasive treatment of proximal humerus fractures with locking compression plate improves shoulder function in older patients: study protocol for a prospective randomized controlled trial. Clin Transl Orthop.2016;1:51-57.
18. Li Z. Minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws for repair of distal radius fracture: study protocol for a randomized controlled trial. Clin Transl Orthop. 2016;1:58-63.
 Clinical Trials in Orthopedic Disorder2017年2期
Clinical Trials in Orthopedic Disorder2017年2期
- Clinical Trials in Orthopedic Disorder的其它文章
- Efficacy of endoscopic transantral versus transorbital surgical approaches in the repair of orbital blowout fractures: study protocol for a randomized controlled trial
- Platelet-rich plasma combined with conventional surgery in the treatment of atrophic nonunion of femoral shaft fractures: study protocol for a prospective, randomized, controlled clinical trial
- Effects of two different tranexamic acid administration methods on perioperative blood loss in total hip arthroplasty: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Supercapsular percutaneously-assisted total hip approach for the elderly with femoral neck fractures: study protocol for a prospective, open-label, randomized, controlled clinical trial
- Should angiography be done in suspected tuberculosis of spine in an endemic country? – Hemangioma masquerading as tuberculosis of spine
