Application of transjugular intrahepatic portosystemic stent shunt combined with chemotherapy in treatment of hepatocellular carcinoma with portal vein tumor thrombosis
, ,
(Department of Gastroenterology, the Second Affiliated Hospital ofNanchang University, Nanchang 330006, China)
Application of transjugular intrahepatic portosystemic stent shunt combined with chemotherapy in treatment of hepatocellular carcinoma with portal vein tumor thrombosis
XIEZhengyuan,XIONGKai,GUOWuhua*
(DepartmentofGastroenterology,theSecondAffiliatedHospitalofNanchangUniversity,Nanchang330006,China)
Objective To explore the application value of transjugular intrahepatic portosystemic shunt (TIPS) combined with chemotherapy in treatment of hepatocellular carcinoma with portal vein tumor thrombus (PVTT). Methods According to therapeutic methods, totally 39 patients with hepatocellular carcinoma with PVTT, who were not appropriate surgical treatment or unwilling to surgical treatment were divided into two groups. There were 17 cases in treatment group and 22 cases in control group. For the patients of treatment group, the portal vein tumor thrombus were opened by TIPS. And the chemotherapy were performed with FOLFOX4 scheme. While for the patients of control group, only conservative treatments were performed. The incidence rate of complications, quality of life (QOL) scores and survival times between the two groups were compared. Results In treatment group, TIPS was performed successfully in 14 of 17 cases with the success rate of 82.35% (14/17). The incidence rates of combind upper gastrointestinal hemorrhage, intractable ascites of treatment group were lower than those of control group (bothP<0.05). The QOL scores of treatment group was higher than that of control group (P<0.05). The average survival times of patients were (114.50±47.18) days in treatment group and (88.10±36.81) days in control group. The difference of average survival times was statistically significant between the two groups (P<0.05). There was no statistical difference of the incidence rates of hepatic encephalopathy between the two groups (P=0.074). Conclusion TIPS combined with chemotherapy is a feasible and effective method for the treatment of hepatocellular carcinoma with PVTT.
Carcinoma, hepatocellular; Portal vein; Portasystemic shunt, transjugular intrahepatic; chemicals, therapeutic
门静脉癌栓(portal vein tumor thrombus, PVTT)的发生往往提示原发性肝癌已属晚期,此类患者大多失去外科手术机会,此时即使积极采取外科手术治疗,临床疗效也难以保证,患者总体生存期并无明显延长,且手术创伤大,可能使患者在有限的生存期内生活质量更为下降[1]。而单纯化疗也难以取得满意效果。近年来,我院采用经颈静脉肝内门体分流术(transjugular intrahepatic portosystemic shunt, TIPS)畅通门静脉及降低门静脉压后联合化疗对肝癌伴PVTT患者进行治疗,取得一定疗效,现报道如下。
1 资料与方法
1.1一般资料 2013年6月—2015年12月我院收治的原发性肝癌伴PVTT患者39例,男35例,女4例,年龄35~68岁,平均(52.6±11.4岁)。所有患者均符合2011版原发性肝癌诊疗规范[2]标准,并经CTA证实伴有确切的PVTT;均无外科手术治疗适应证和(或)无外科手术意愿。依据临床治疗方案分为两组,其中TIPS联合化疗组17例,接受TIPS治疗,术后接受化疗及常规内科药物治疗;对照组22例,仅接受内科药物护肝、输蛋白、利尿等对症处理。本研究经医院医学伦理委员会批准,接受治疗者均对治疗方案知情同意,并签署知情同意书。两组患者临床资料见表1。
1.2仪器与方法
1.2.1TIPS治疗 采用Philips FD20 Allura Xper FD20血管造影机作为影像引导设备。TIPS手术步骤包括:①行右颈内静脉穿刺后,引入导丝,将RUPS100置入肝中静脉或肝右静脉;②另行右股动脉穿刺,将导管置于肠系膜上动脉,行肠系膜上动脉造影,观察门静脉位置及与肝中静脉或肝右静脉空间方位;③调整RUPS100穿刺角度,穿刺门静脉,缓慢注入对比剂以显示门静脉走行,引入导丝,经门静脉主干超选择至肠系膜上静脉;④以球囊导管扩张穿刺道及门静脉狭窄段后,植入支架覆盖癌栓全程。门体分流支架采用金属覆膜支架(Wallgraft支架,Boston科学公司,美国),内径8、10 mm;门静脉内支架采用金属裸支架(Luminexx支架,Bard医疗公司,美国),内径8、10、12 mm。维持门静脉通畅,造影见血流进入肝静脉或下腔静脉后结束治疗(图1)。
1.2.2化疗方案 TIPS治疗后第2天开始化疗。采用FOLFOX4方案:奥沙利铂(oxaliplatin, OXA) 85 mg/m2,静脉滴注,第1天用;亚叶酸钙(leucovorin calcium, LV) 200 mg/m2,静脉滴注2 h,第1、2天用;5-氟尿嘧啶(5-fluorouracil, 5-FU),以400 mg/m2静脉注射,继以600 mg/m2持续静脉滴注22 h,第1、2天用;每2周为1个治疗周期。
1.3评价指标 观察并记录两组患者治疗后并发症情况,包括上消化道出血、顽固性腹腔积液、肝性脑病。采用肿瘤患者生活质量评分(quality of life, QOL)标准对两组生活质量进行评价。记录两组患者生存时间。

2 结果
TIPS联合化疗组17例患者中,对14例成功实施TIPS,成功率82.35%(14/17);3例失败,原因包括术中穿刺无法刺中门静脉主干或一级分支2例,术中呕血,血压下降无法耐受手术1例。3例失败患者均因上消化道出血难以控制死亡。
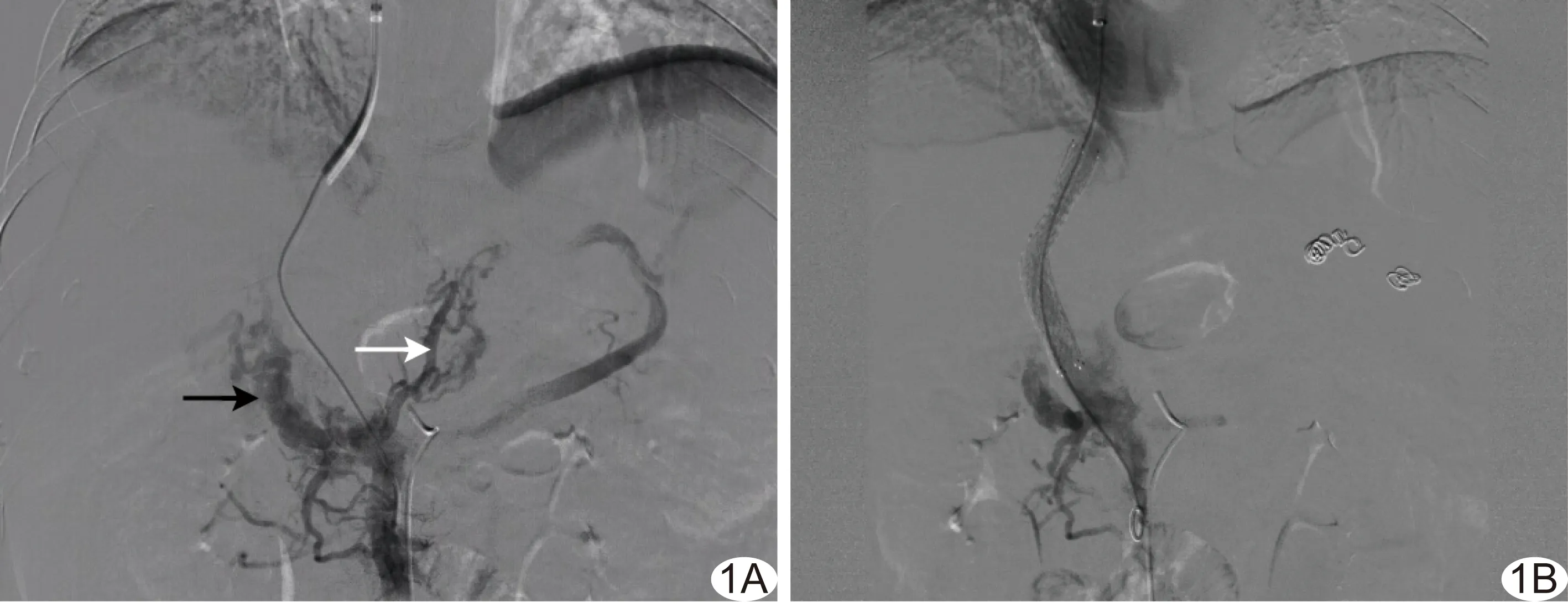
图1 患者男,48岁,PVTT伴门静脉海绵样变 A.TIPS术中穿刺成功后行肠系膜上静脉造影示门静脉栓塞后正常结构消失,代之为门静脉海绵样变(黑箭),并见曲张的胃冠状静脉(白箭); B.置入分流支架后,门静脉海绵样变减轻,胃冠状静脉消失
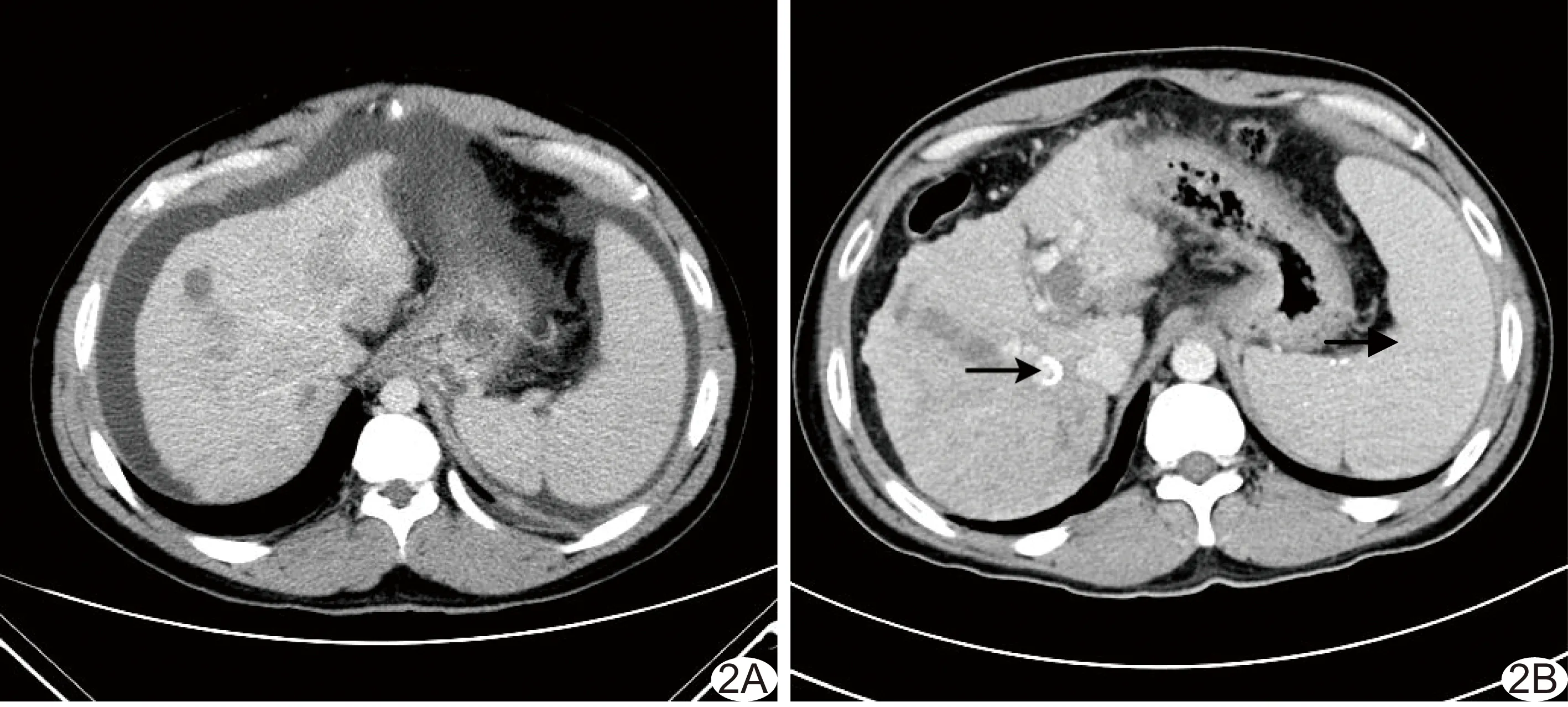
图2 患者男,37岁,肝癌伴PVTT A.TIPS联合化疗前CT 示上消化道出血、大量腹腔积液; B.术后70天CT示分流支架(箭)通畅,腹腔积液消失
TIPS联合化疗组患者并发上消化道出血、顽固性腹腔积液的发生率低于对照组(P均<0.05,图2),两组肝性脑病发生率差异无统计学意义(P=0.074),见表2。TIPS联合化疗组肿瘤患者QOL评分高于对照组,差异有统计学意义(P<0.05,表2)。TIPS联合化疗组平均生存期为(114.50±47.18)天,对照组为(88.10±36.81)天,差异均有统计学意义(P<0.05,表2)。两组生存曲线见图3。
3 讨论
肝癌伴PVTT患者生存期有限,生活质量较差,临床治疗相当棘手[3]。尽可能地减少创伤,延长生存期,改善生活质量是临床目前对此类患者的治疗目标[4]。通过微创介入的方法来治疗肝癌伴PVTT具有较高的临床应用价值[5]。
肝癌伴PVTT患者主要的病理生理改变是引起并逐渐加重门静脉高压,从而导致上消化道出血和顽固性腹腔积液[6];另一方面,门静脉堵塞,减少了肝脏营养血流灌注,肝脏功能损伤加剧,加速死亡[7]。因此,畅通门静脉是逆转此类患者病理生理改变积极、有效的治疗方法[8]。传统外科手术方式仅适用于肝功能Child-Pugh A级患者[9],且创伤大,术后多数患者也无法马上耐受化疗,极易于短期内再次形成PVTT[10]。肝功能Child-Pugh B级和C级是传统外科手术的禁忌证[11]。因此,微创介入方法治疗肝癌伴PVTT的理念应运而生[12]。国内徐克等[13]于1995年成功将TIPS技术应用于肝癌合并门静脉高压患者的治疗,取得一定的疗效,发现TIPS可有效缓解门静脉高压,尽管其所选病例门静脉均通畅,但为TIPS技术应用于肝癌伴PVTT的治疗提供了参考。近年来,冯超等[14]采用覆膜支架进行TIPS治疗,发现其对门静脉主干癌栓患者具有较好的近期疗效,且此法相对安全、可行。通过TIPS技术放置的门静脉支架既可达到分流降门静脉压的目的,也在一定程度上恢复了向肝血流,使得肝脏血流灌注增加,肝功能得以维持[15]。TIPS为患者术后立即进行化疗创造了条件。本研究中,17例患者愿意接受介入治疗,对其中14例治疗成功,成功率达82.35%(14/17)。
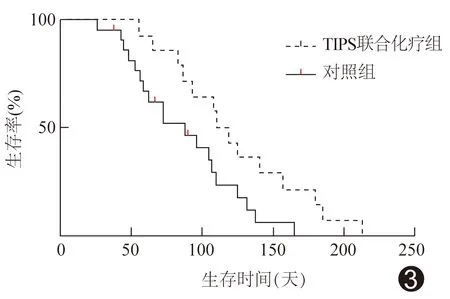
图3 两组患者生存曲线
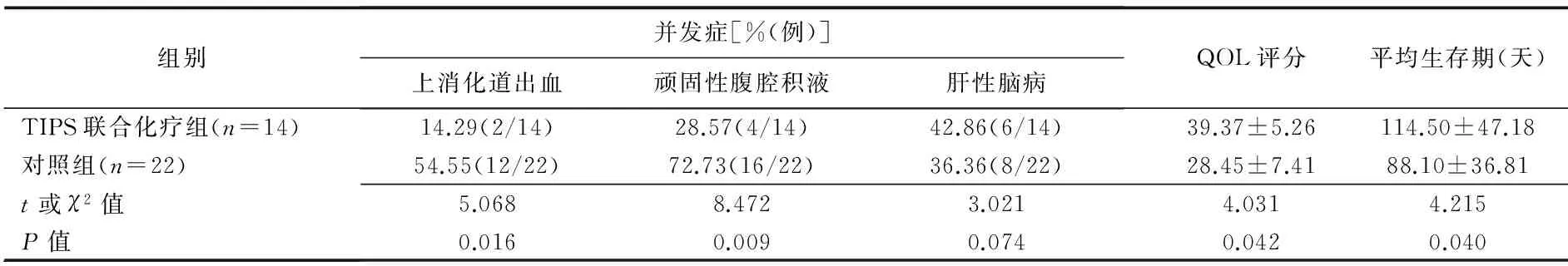
组别并发症[%(例)]上消化道出血顽固性腹腔积液肝性脑病QOL评分平均生存期(天)TIPS联合化疗组(n=14)14.29(2/14)28.57(4/14)42.86(6/14)39.37±5.26114.50±47.18对照组(n=22)54.55(12/22)72.73(16/22)36.36(8/22)28.45±7.4188.10±36.81t或χ2值P值5.0688.4723.0214.0314.2150.0160.0090.0740.0420.040
注:TIPS联合化疗组17例中3例未完成治疗,共14例完成治疗
既往肝癌的化疗无标准方案。杨柳青等[16]研究认为,FOLFOX4方案可为亚洲肝癌患者带来临床获益。进一步研究[17]发现,针对国人肝癌患者进行FOLFOX4化疗方案与阿霉素化疗相比,可显著提高治疗有效率、疾病控制率和延长生存期。目前该方案已逐渐成为国内晚期肝癌的主要化疗方案。但化疗也具有其局限性,肝功能不全为相对禁忌证,此时化疗可能进一步加重肝功能损害[18]。本组患者肝功能多为Child-Pugh B级和C级(33/36,91.67%),在门静脉堵塞未解除的情况下直接化疗必然加重肝功能损害。当门静脉重新开通后,肝脏血流灌注增加,肝功能得以维持,此时结合化疗可控制癌栓短期内再次形成[19]。本研究发现,经TIPS联合化疗后,患者上消化道出血和顽固性腹腔积液发生率明显低于单纯内科保守治疗(P均<0.05)。此外,本研究发现TIPS联合化疗组肿瘤患者QOL评分明显高于对照组(P=0.042),分析原因可能为患者经TIPS联合化疗后腹胀减轻、食欲好转后,精神心理压力下降,因此生活质量得到明显改善。有研究[20]报道,肝癌合并PVTT患者因门静脉堵塞,肝脏缺血明显,肝功能恶化较快,发生肝性脑病的概率较单纯肝硬化、肝癌患者更高(P<0.05)。一般认为肝性脑病是TIPS术后的主要并发症,是影响TIPS手术患者生存期的主要因素[21]。但本研究发现,TIPS联合化疗组与对照组患者肝性脑病发生率差异无统计学意义(P=0.074),可能与肝癌合并PVTT患者门静脉堵塞,易出现侧支循环开放,介入手术开通门静脉后尽管出现血液绕开肝脏分流,但同时从侧支循环分流的血液减少明显,因此发生肝性脑病的概率并无明显增加[22]。本研究结果显示,TIPS联合化疗组患者并发症更少,生活质量更高,因此其平均生存期较仅接受内科保守治疗的对照组更长,两组生存期差异有统计学意义(P=0.04,图3)。
本研究的局限性:①样本量有限;②未能对支架大小的选择、化疗方案和周期的选择、是否可联合靶点类抗肿瘤药物治疗及影响肝癌预后的多因素作用等问题进行进一步分析。
综上所述,通过TIPS技术联合化疗对肝功能较差的肝癌伴PVTT患者进行积极治疗,相对于单纯内科保守治疗可能获得更为满意的疗效,有助于改善患者的生活质量并延长生存期,值得临床推广。
[1] Kojima H, Hatano E, Taura K, et al. Hepatic pesection for hepatocellular carcinoma with tumor thrombus in the major portal vein. Dig Surg, 2015,32(6):413-420.
[2] 中华人民共和国卫生部.原发性肝癌诊疗规范(2011年版).临床肿瘤学杂志,2011,16(10):929-946.
[3] Tang ZY, Zhou BH, Wang W et al. Curative analysis of several therapeutic methods for primary hepatocellular carcinoma with portal vein tumor thrombus. Hepatogastroenterology, 2015,62(139):703-709.
[4] Han K, Kim JH, Ko GY, et al. Treatment of hepatocellular carcinoma with portal venous tumor thrombosis: A comprehensive review. World J Gastroenterol, 2016,22(1):407-416.
[5] Qiu B, Zhao MF, Yue ZD, et al. Combined transjugular intrahepatic portosystemic shunt and other interventions for hepatocellular carcinoma with portal hypertension. World J Gastr oenterol, 2015,21(43):12439-12447.
[6] Kawai T, Yashima Y, Sugimoto T, et al. Emergency endoscopic variceal ligation following variceal rupture in patients with advanced hepatocellular carcinoma and portal vein tumor thrombosis: A retrospective study. World J Surg Oncol, 2016,14(1):52.
[7] Manzano-Robleda Mdel C, Barranco-Fragoso B, Uribe M, et al.Portal vein thrombosis: What is new? Ann Hepatol, 2015,14(1):20-27.
[8] Thornburg B, Desai K, Hickey R, et al. Portal vein recanalization and transjugular intrahepatic portosystemic shunt creation for chronic portal vein thrombosis: Technical Considerations. Tech Vasc Interv Radiol, 2016,19(1):52-60.
[9] 李磊,李忠超,卢红,等.肝细胞癌合并门静脉癌栓的治疗现状及进展.中华外科杂志,2015,53(6):468-471.
[10] Zhang YF, Wei W, Guo ZX, et al. Hepatic resection versus transcatheter arterial chemoembolization for the treatment of hepatocellular carcinoma with hepatic vein tumor thrombus. Jpn J Clin Oncol, 2015,45(9):837-843.
[11] Pesi B, Ferrero A, Grazi GL, et al. Liver resection with thrombectomy as a treatment of hepatocellular carcinoma with major vascular invasion: Results from a retrospective multicentric study. Am J Surg, 2015,210(1):35-44.
[12] Zhao JB, Feng C, Zhu QH, et al. Transjugular intrahepatic portosystemic shunt with covered stents for hepatocellular carcinoma with portal vein tumor thrombosis. World J Gastroenterol, 2014,20(6):1602-1607.
[13] 徐克,周玉斌. 肝肿瘤并门脉高压上消化道出血TIPSS治疗.实用医学杂,2001,17(4):288-290.
[14] 冯超,赵剑波,陈勇,等.覆膜支架经颈静脉肝内门体分流术治疗门静脉主干癌栓.中国介入影像与治疗学,2014,11(12):775-778.
[15] Ahmed R, Santhanam P, Rayyan Y. MELD-Na as a prognostic indicator of 30- and 90-day mortality in patients with end-stage liver disease after creation of transjugular intrahepatic portosystemic shunt. Eur J Gastroenterol Hepatol, 2015,27(10):1226-1227.
[16] 杨柳青,秦叔逵,赵宁莉,等.FOLFOX4方案治疗中晚期原发性肝癌的临床研究,临床肿瘤学杂志,2013,18(2):108-113.
[17] Qin S, Cheng Y, Liang J, et al. Efficacy and safety of the FOLFOX4 regimen versus doxorubicin in Chinese patients with advanced hepatocellular carcinoma: A subgroup analysis of the EACH study. Oncologist, 2014,19(11):1169-1178.
[18] Tural D, Akar E, Öztürk MA, et al. Severe liver dysfunction and safe use of 5-fluorouracil leucovorin and oxaliplatin in one patient with metastatic colorectal carcinoma. J Cancer Res Ther, 2014,10(3):745-748.
[19] Lin CC, Hung CF, Chen WT, et al. Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein thrombosis: Impact of early response to 4 weeks of treatment. Liver Cancer, 2015,4(4):228-240.
[20] Cabibbo G, Maida M, Genco C, et al. Natural history of untreatable hepatocellular carcinoma: A retrospective cohort study. World J Hepatol, 2012, 4(9):256-261.
[21] Yao J, Zuo L, An G, et al. Risk factors for hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in patients with hepatocellular carcinoma and portal hypertension. J Gastrointestin Liver Dis, 2015,24(3):301-307.
[22] Casadaban LC, Parvinian A, Minocha J, et al. Clearing the confusion over hepatic encephalopathy after TIPS creation: Incidence, prognostic factors, and clinical outcomes. Dig Dis Sci, 2015,60(4):1059-1066.
江西省卫生计生委科技计划项目(20151076)。
谢正元(1976—),男,江西宁都人,博士,副主任医师。研究方向:消化系统疾病放射介入诊治。E-mail: xzyxzy1230@sohu.com
郭武华,南昌大学第二附属医院消化内科,330006。E-mail: xzyxzy1230@163.com
2016-05-19
2016-09-01
经颈静脉肝内门体分流术联合化疗在原发性肝癌伴门静脉癌栓治疗中的应用
谢正元,熊 恺,郭武华*
(南昌大学第二附属医院消化内科,江西 南昌 330006)
目的 探讨经颈静脉肝内门体分流术(TIPS)联合化疗在原发性肝癌伴门静脉癌栓(PVTT)治疗中的应用价值。方法 将39例不宜或不愿接受外科手术治疗的肝癌伴PVTT患者按治疗方法分为两组。TIPS联合化疗组17例,于TIPS治疗后接受FOLFOX4化疗方案;对照组22例,单纯接受内科保守药物治疗。比较两组患者并发症发生率、生活质量评分(QOL)及生存期。结果 TIPS联合化疗组中,14例TIPS治疗成功,成功率82.35%(14/17)。TIPS联合化疗组并发上消化道出血、顽固性腹腔积液的发生率低于对照组,QOL评分高于对照组,平均生存期[(114.50±47.18)天]长于对照组[(88.10±36.81)天],差异均有统计学意义(P均<0.05)。两组肝性脑病发生率差异无统计学意义(P=0.074)。结论 TIPS联合化疗是治疗原发性肝癌伴PVTT的一种较为可行、有效的方法。
癌,肝细胞;门静脉;门体分流术,经颈静脉肝内;化学药物,治疗性
R735.7; R815
A
1672-8475(2016)10-0600-05
10.13929/j.1672-8475.2016.10.005
- 中国介入影像与治疗学的其它文章
- Comparative analysis of ultrasonographic and pathologic findings of uterine lipoleiomyoma
- Ultrasound-guided histology biopsy in diagnosis of benign and malignant thyroid nodules: Meta analysis
- MRI findings of cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy
- Application of Orem self-care theory on nursing for patients with hepatocellular carcinoma after transcatheter arterial chemoembolization
- Preparation and characteristic comparison of two phase-transition multifunctional nanoparticles
- Clinical analysis of fetal malformation