脑保护下颈动脉支架成形术治疗颈动脉中重度钙化狭窄的疗效分析
张 路 唐 骁 符伟国 史振宇 吕 鹏 戴媛媛 王玉琦 郭大乔△
(1复旦大学附属中山医院血管外科-复旦大学血管外科研究所;2复旦大学附属中山医院放射科 上海 200032)
脑保护下颈动脉支架成形术治疗颈动脉中重度钙化狭窄的疗效分析
张路1唐骁1符伟国1史振宇1吕鹏2戴媛媛2王玉琦1郭大乔1△
(1复旦大学附属中山医院血管外科-复旦大学血管外科研究所;2复旦大学附属中山医院放射科上海200032)
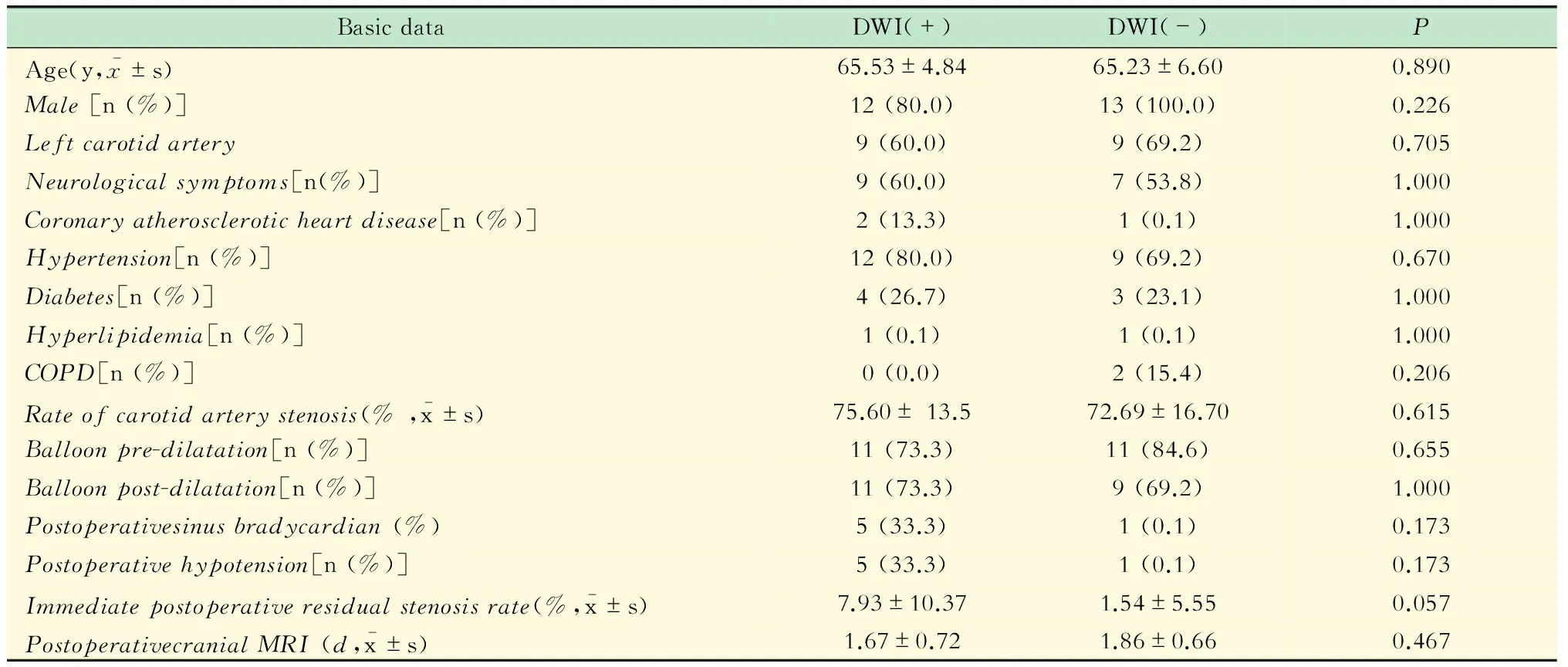
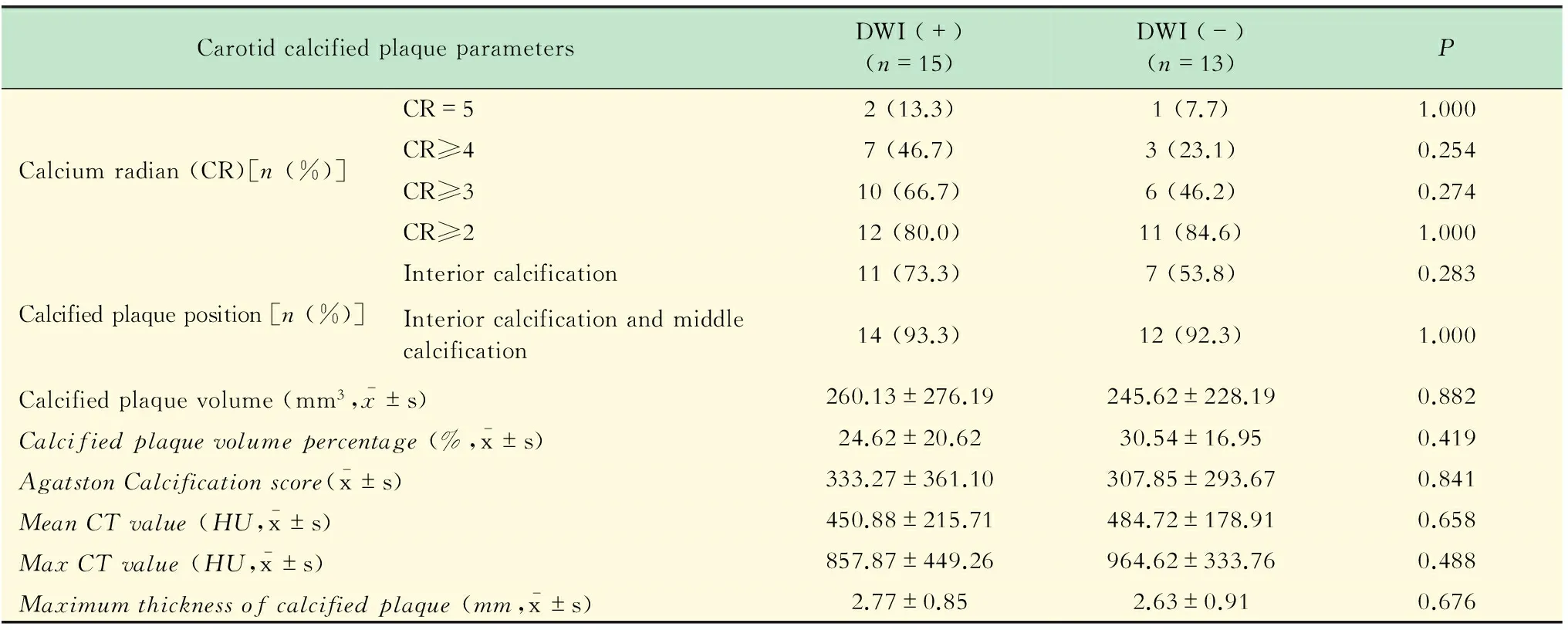
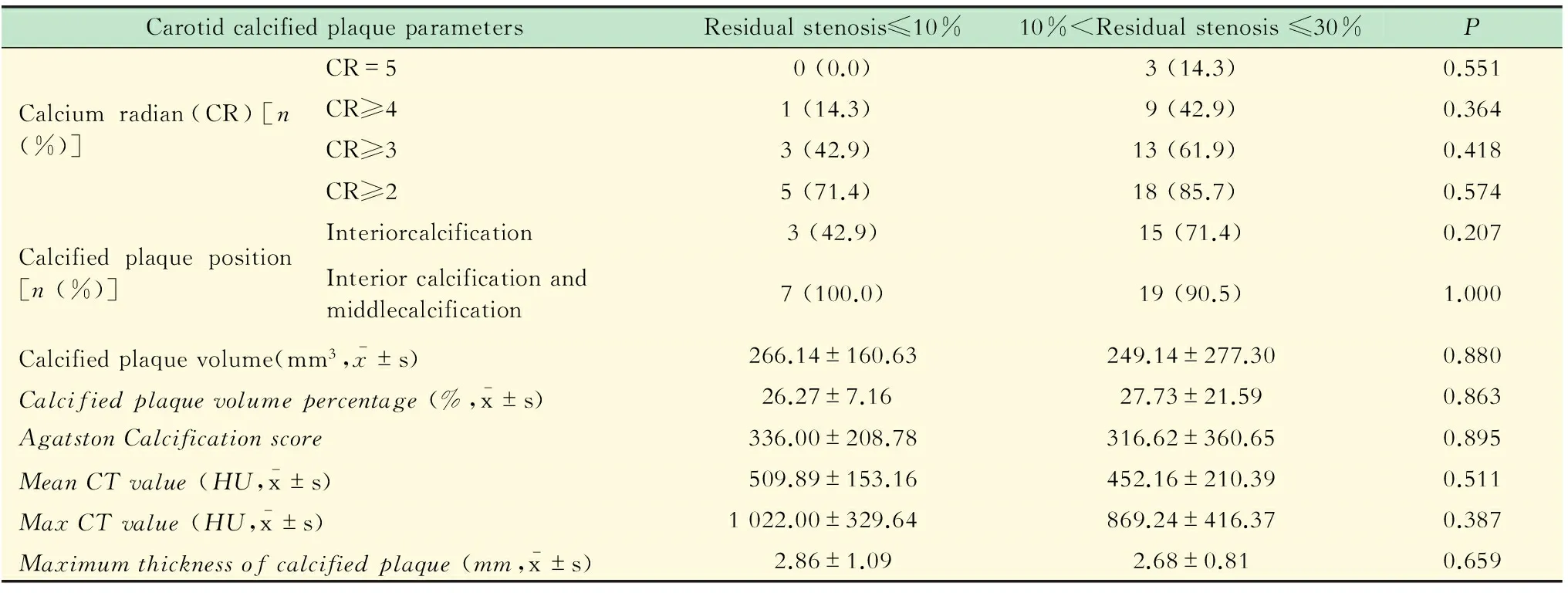
目的评价脑保护下颈动脉支架成形术(carotid angioplasty and stenting,CAS)治疗颈动脉中重度钙化狭窄的安全性及有效性。方法28例颈动脉中重度钙化狭窄患者接受了脑保护下颈动脉支架植入术,均接受了术前颈动脉CT血管造影检查及术前术后头颅MRI检查,评价术后新发弥散加权(diffusion weighted imaging,DWI)病灶、术后支架即刻残余狭窄率与钙化斑块的关系。结果28例次CAS的即刻成功率为100%。围手术期无死亡或心肌梗死等严重并发症。术后3天内复查头颅MRI:新发DWI病灶15例(53.6%),均无神经系统症状。根据术后有无新发DWI病灶,将患者分为阳性组和阴性组,比较两组钙化斑块的位置、体积大小、钙化弧度(calcium radian,CR)及Agatston钙化评分、钙化CT值、钙化斑块体积百分比和颈动脉斑块最大厚度,差异均无统计学意义(P>0.05)。术后12个月内,1例患者发生手术侧脑卒中,其余27例恢复良好,无短暂性脑缺血发作或脑卒中发生。术后1年复查颈动脉超声,并随访颈部X线,支架内再狭窄发生率为0,支架断裂发生率为0。结论在实施远端脑保护装置的情况下,CAS对颈动脉中重度钙化狭窄是一种安全有效的治疗方法。钙化斑块的位置、体积大小、CR、Agatston钙化评分、钙化斑块CT值、钙化斑块体积百分比和颈动脉斑块最大厚度对术后新发DWI病灶的发生率无明显影响。
颈动脉狭窄;支架;钙化;新发DWI病灶;残余狭窄率
在中国,脑卒中已成为死亡的首位原因[1]。颈动脉狭窄是脑卒中重要的危险因素,20%~25%脑卒中与颈动脉狭窄密切相关[2]。作为颈动脉狭窄的治疗方式之一,颈动脉支架成形术(carotid angioplasty and stenting,CAS)取得了良好的效果。CAS具有微创的优点,但是目前颈动脉狭窄病变的钙化严重程度对于CAS疗效的影响,尚无确切结论。如何选择合适患者,对于CAS及颈动脉内膜剥脱术这类预防性手术具有重要的意义。复旦大学附属中山医院血管外科自2014年6月至 2015年1月共实施127例次CAS治疗颅外颈动脉狭窄,本研究回顾性分析了其中28例次颈内动脉中重度钙化狭窄病例,就围手术期及中期疗效分析如下。
资 料 和 方 法
病例资料CAS适应证为颈动脉直径狭窄率超过50%的有症状患者,或者颈动脉直径狭窄率超过60%的无症状患者[2]。入组条件为:非环状钙化、严重心肺功能不全、对侧颈动脉严重狭窄或闭塞、颈部放疗后、超过第2颈椎的高位病变或锁骨以下的低位病变等。排除条件为:颈动脉环状钙化、髂动脉闭塞等颈动脉支架入路困难、严重肾功能不全、对比剂过敏史及患者选择颈动脉内膜剥脱术等。颈动脉直径狭窄率、颈动脉残余狭窄及颈动脉再狭窄率的计算按照北美症状性颈动脉狭窄内膜切除研究(the North American Symptomatic Carotid Endarterectomy Trial,NASCET)的标准[3]。
颈动脉钙化斑块分布见图1:无钙化;外层钙化(靠近外膜及外膜以外);中层钙化(既不靠近管腔面,也不靠近外膜);内层钙化(靠近血管管腔面)。颈动脉钙化弧度大小(calcium radian,CR)见图2:无钙化;CR≤30°钙化;30°钙化 方法术前所有入组患者行颈动脉CT血管造影和头颅MRI,术后3天内完成MRI。术前1周口服肠溶阿斯匹林100 mg/d和氯吡格雷75 mg/d,所有患者均行全身麻醉,经股动脉入路。颈动脉狭窄病变的预扩张和后扩张,尽量在脑保护伞释放到位后进行;如果颈动脉呈重度狭窄,脑保护伞无法顺利通过,则应用小直径球囊(2.5 mm~3mm)快速预扩,以便脑保护伞顺利通过病变。所有患者均在路径图模式下释放脑保护伞和颈动脉支架。如果残余狭窄>30%,则行后扩。术后即刻对颈动脉及全脑血管造影,确认远端有无栓塞及支架残余狭窄情况。术毕连续监测血压心率至少24 h观察神经系统症状和体征,出院后继续口服肠溶阿司匹林100 mg/d (终身)及氯吡格雷75 mg/d (至少半年)。 2014年6月至2015年1月,我们共实施了127例颈动脉手术,其中颈动脉中重度钙化患者28例。有症状患者15例,无症状患者13例。所有患者术中都应用远端脑保护装置NAV6(美国Abbott公司),共放置自膨式颈动脉支架Acculink(美国Abbott公司)28个,即刻成功率为100%(残余狭窄<30%)。围手术期无死亡或心肌梗死等严重并发症发生。术后3天内复查头颅MRI,结果显示新发DWI病灶15例(53.6%),均无神经系统症状。1例患者于术后1个月出现手术侧脑卒中,患侧肢体肌力明显降低(Ⅱ级),于康复治疗后,肢体肌力恢复至Ⅳ级,顺利出院,其余患者无症状性脑卒中发作。根据术后新发DWI病灶将患者分为新发DWI病灶阳性组[DWI(+)]和新发DWI病灶阴性组[DWI(-)]。两组间在年龄、性别、伴随基础疾病、有无神经系统症状、术前颈动脉狭窄率及有无预扩、后扩,心率、血压有无下降、术前颈动脉狭窄率、术后即刻残余狭窄率、术后复查头颅MRI时间差异均无统计学意义(P>0.05,表1)。 术后DWI(+)组和DWI(-)组在CR、颈动脉斑块的位置、钙化斑块体积大小、钙化斑块体积百分比、钙化斑块CT值及钙化斑块的最大厚度差异均无统计学意义(P>0.05,表2)。术后支架即刻残余狭窄率在颈动脉斑块的位置、钙化斑块体积大小、钙化斑块体积百分比、CR、钙化斑块CT值及钙化斑块的最大厚度差异均无统计学意义(P>0.05,表3)。28例患者术后1年随访颈动脉超声,支架内再狭窄率为0。术后1年随访颈部正侧位X线,支架断裂发生率为0。 表1 新发DWI病灶阳性组和新发DWI病灶阴性组临床基本资料 表2 新发DWI病灶与术前颈动脉CTA测量钙化斑块参数的关系 表3 术后即刻残余狭窄与钙化斑块之间的关系 目前颅外颈动脉狭窄的手术指征,主要包括动脉狭窄程度和神经系统症状,即症状性颈动脉狭窄超过50%,无症状性颈动脉狭窄超过60%[2]。虽然数字减影血管造影仍是颈动脉狭窄诊断的金标准,但目前临床筛选颅外颈动脉狭窄高危病变的检测方法存在不足。从狭窄测量标准来讲,血管造影测量采用北美症状性颈动脉内膜切除术试验(NACET)或者欧洲颈动脉手术试验(European Carotid Surgery Trial,ECST)标准。但是狭窄程度并不能完全区分高危和低危病变。研究显示轻度狭窄也可导致TIA或卒中等神经系统事件,当颈动脉狭窄度0~29%时,TIA或卒中发生率为2.1%/年,当颈动脉狭窄度为30%~75%时,TIA或卒中发生率为5.7%/年[5]。从颈动脉斑块成分和性质评估来讲,血管造影难以鉴别稳定性斑块和不稳定性斑块。颈动脉斑块性质是影响手术效果的因素之一,易损斑块往往在CAS中容易发生破裂脱落,引起新发DWI病灶,随着远端脑保护装置的应用,CAS后新发DWI病灶的发生率逐渐下降[6-7]。Gensicke 等[8]报道,CAS后新发DWI病灶可能增加未来脑血管事件再次发生的发生率。 以往研究显示,严重钙化狭窄是CAS的危险因素。由于颈动脉支架对颈动脉窦的压迫,在CAS后可能导致血压降低、心率下降,进而造成术后脑灌注不足引发缺血灶的发生[9]。在颈部X线可显示颈动脉斑块与CAS后的支架断裂、扭曲密切相关[10],且Ⅲ级以上钙化斑块引起支架断裂的概率是其他斑块的4.5倍[11]。严重钙化的颈动脉斑块导致颈动脉支架的展开效果不佳,导致支架内再狭窄的发生率较高[12]。严重钙化的颈动脉狭窄,影响自膨式支架的扩张,进一步导致支架内再狭窄,为了减少支架残余狭窄率就需要后扩张应用更大的球囊压力来克服斑块的挤压。Obeid 等[13]发现颈动脉支架后扩张联合预扩张比单纯预扩张使围手术期脑卒中和死亡率增加了2.4倍。但是并非所有颈动脉钙化病变都是CAS手术的禁忌证,如何选择合适患者,如何详细评估颈动脉钙化病变,需要进一步详细的研究。 Katano等[12]研究发现,颈动脉支架残余狭窄率与钙化斑块的钙化评分有关,认为术前颈动脉钙化斑块评分是术后支架残余狭窄的唯一预测因子。Tsutsumi等[14-15]发现颈动脉残余狭窄率与钙化斑块的体积无关,但是他们发现斑块CR超过278°时,支架断裂的发生率为94.4%(17/18)。本临床研究中,支架残余狭窄率与钙化斑块的体积、位置、钙化斑块CT值、CR及Agatston钙化积分均无关系,术后1年无支架断裂发生。钙化斑块稳定的因素,可能包括生物力学和炎症两方面,Huang等[16]利用血流动力学有限元分析发现,钙化成分并不像脂质成分那样增加纤维帽的生物力学压力。Shaalan 等[17]发现纤维帽的炎性反应与斑块的比例呈反比,这也解释了斑块钙化成分越多,斑块越稳定的原因。本临床研究证实,术后新发DWI病灶与CR、颈动脉斑块的位置、钙化斑块体积大小、钙化斑块体积百分比、钙化斑块CT值及钙化斑块的最大厚度均无关系,从而也证明了钙化成分的稳定性。文献报道[13]后扩张使围手术期脑卒中率及死亡率增加,因此本组临床研究采用充分预扩张并尽量避免支架内后扩的原则,结果显示预扩张或者后扩张对新发DWI病灶并无影响,分析原因,考虑本临床研究入组患者虽为中重度颈动脉钙化狭窄,但均为非环状钙化,术中不需要特别大的球囊扩张压力来克服钙化斑块的挤压,减少了斑块碎屑脱落的风险。本临床研究主要不足是病例数较少,尚待更大样本量和更长的随访时间来验证结果。 本组病例术后出现新发DWI病灶的患者都未表现神经系统症状和体征,均通过CAS术后3天内实施的头颅MRI-DWI序列检查发现,分析为术中微栓子脱落所致。术中微栓子脱落可能发生在CAS的任何阶段,尤其是导丝通过ICA病变及支架释放时,脱落微栓子最多[18]。尽管术后新发脑DWI病灶没有任何症状且可以部分吸收[4],但有研究表明,隐匿性DWI病灶与阿尔兹海默症[19]、认知功能障碍[20-22]、抑郁[23-26]等有关。有研究证实这种隐匿性的脑缺血病灶使未来卒中的风险增加2~4倍[27-28]。国际颈动脉支架研究-磁共振研究中CAS术后新发脑DWI病灶的发生率为50%[4],Bijuklic 等[29]研究发现其发生率甚至高达87.1%。因此,本临床研究中CAS后新发DWI病灶的发生率为53.6%(15/28),与文献报道基本一致。 总之,对于非环状钙化的颈动脉狭窄,无论颈动脉斑块的位置、CR、钙化斑块体积大小、钙化斑块体积的百分比、钙化斑块CT值、Agatston钙化积分及钙化斑块的最大厚度,对CAS术后新发DWI病灶和支架残余狭窄均无影响。因此,对于中重度钙化颈动脉狭窄,远端脑保护装置下的CAS是安全有效的治疗方法。 [1]LIU L,WANG D,WONG KS,et al.Stroke and stroke care in China:huge burden,significant workload,and a national priority[J].Stroke J Cereb Circ,2011,42(12):3651-3654. [2]BROTT TG,HALPERIN JL,ABBARA S,et al.2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease:executive summary[J].Stroke J Cereb Circ,2011,42(8):e420-463. [3]North American Symptomatic Carotid Endarterectomy Trial.Methods,patient characteristics,and progress[J].Stroke J Cereb Circ,1991,22(6):711-720. [4]BONATI LH,JONGEN LM,HALLER S,et al.New ischaemic brain lesions on MRI after stenting or endarterectomy for symptomatic carotid stenosis:a substudy of the International Carotid Stenting Study (ICSS) [J].Lancet Neurol,2010,9(4):353-362. [5]CHAMBERS BR,NORRIS JW.Outcome in patients with asymptomatic neck bruits[J].New England J Med,1986,315(14):860-865. [6]BREWSTER LP,BEAULIEU R,CORRIERE MA,et al.Carotid revascularization outcomes comparing distal filters,flow reversal,and endarterectomy[J].J Vascular Surg,2011,54(4):1000-1005. [7]SORIMACHI T,NISHINO K,MORITA K,et al.Flow impairment during filter-protected carotid artery stent placement:frame-by-frame evaluation of digital subtraction angiography images[J].World Neurosurg,2011,76(3-4):282-287. [8]GENSICKE H,VAN DER WORP HB,NEDERKOORN PJ,et al.Ischemic brain lesions after carotid artery stenting increase future cerebrovascular risk[J].J Am Coll Cardiol,2015,65(6):521-529. [9]ALTINBAS A,ALGRA A,BONATI LH,et al.Periprocedural hemodynamic depression is associated with a higher number of new ischemic brain lesions after stenting in the International Carotid Stenting Study-MRI Substudy[J].Stroke J Cereb Circ,2014,45(1):146-151. [10]CHANG CK,HUDED CP,NOLAN BW,et al.Prevalence and clinical significance of stent fracture and deformation following carotid artery stenting[J].J Vascular Surg,2011,54(3):685-690. [11]COPPI G,MORATTO R,VERONESI J,et al.Carotid artery stent fracture identification and clinical relevance[J].J Vascular Surg,2010,51(6):1397-1405. [12]KATANO H,MASE M,NISHIKAWA Y,et al.Surgical treatment for carotid stenoses with highly calcified plaques[J].J Stroke Cerebrovasc Dis,2014,23(1):148-154. [13]OBEID T,ARNAOUTAKIS DJ,ARHUIDESE I,et al.Poststent ballooning is associated with increased periprocedural stroke and death rate in carotid artery stenting[J].J Vascular Surg,2015,62(3):616-623. [14]TSUTSUMI M,AIKAWA H,ONIZUKA M,et al.Carotid artery stenting for calcified lesions[J].AJNR Am Neuroradiol,2008,29(8):1590-1593. [15]TSUTSUMI M,KODAMA T,AIKAWA H,et al.Fragmentation of calcified plaque after carotid artery stenting in heavily calcified circumferential stenosis[J].Neuroradiology,2010,52(9):831-836. [16]HUANG H,VIRMANI R,YOUNIS H,et al.The impact of calcification on the biomechanical stability of atherosclerotic plaques[J].Circulation,2001,103(8):1051-1056. [17]SHAALAN WE,CHENG H,GEWERTZ B,et al.Degree of carotid plaque calcification in relation to symptomatic outcome and plaque inflammation[J].J Vascular Surg,2004,40(2):262-269. [18]VOS JA,de BORST GJ,OVERTOOM TT,et al.Carotid angioplasty and stenting:treatment of postcarotid endarterectomy restenosis is at least as safe as primary stenosis treatment[J].J Vascular Surg,2009,50(4):755-761. [19]BRETELER MM.Vascular risk factors for Alzheimer's disease:an epidemiologic perspective[J].Neurobiol Aging,2000,21(2):153-160. [20]PRICE TR,MANOLIO TA,KRONMAL RA,et al.Silent brain infarction on magnetic resonance imaging and neurological abnormalities in community-dwelling older adults[J].Stroke J Cereb Circ,1997,28(6):1158-1164. [21]LONGSTRETH WT JR,BERNICK C,MANOLIO TA,et al.Lacunar infarcts defined by magnetic resonance imaging of 3660 elderly people:the Cardiovascular Health Study[J].Archives Oneurol,1998,55(9):1217-1225. [22]VERMEER SE,PRINS ND,DEN HEIJER T,et al.Silent brain infarcts and the risk of dementia and cognitive decline[J].New England J Med,2003,348(13):1215-1222. [23]SATO R,BRYAN RN,FRIED LP.Neuroanatomic and functional correlates of depressed mood:the Cardiovascular Health Study[J].Am J Epidemiol,1999,150(9):919-929. [24]STEFFENS DC,HELMS MJ,KRISHNAN KR,et al.Cerebrovascular disease and depression symptoms in the cardiovascular health study[J].Stroke J Cereb Circ,1999,30(10):2159-2166. [25]STEFFENS DC,KRISHNAN KR,CRUMP C,et al.Cerebrovascular disease and evolution of depressive symptoms in the cardiovascular health study[J].Stroke J Cereb Circ,2002,33(6):1636-1644. [26]BARNES DE,ALEXOPOULOS GS,LOPEZ OL,et al.Depressive symptoms,vascular disease,and mild cognitive impairment:findings from the cardiovascular health study[J].Archives Gen Psychiatry,2006,63(3):273-279. [27]BERNICK C,KULLER L,DULBERG C,et al.Silent MRI infarcts and the risk of future stroke:the cardiovascular health study[J].Neurology,2001,57(7):1222-1229. [28]VERMEER SE,HOLLANDER M,VAN DIJK EJ,et al.Silent brain infarcts and white matter lesions increase stroke risk in the general population:the Rotterdam Scan Study[J].Stroke;J Cereb Circ,2003,34(5):1126-1129. [29]BIJUKLIC K,WANDLER A,HAZIZI F,et al.The PROFI study (Prevention of Cerebral Embolization by Proximal Balloon Occlusion Compared to Filter Protection During Carotid Artery Stenting):a prospective randomized trial[J].J Am Coll Cardiol,2012,59(15):1383-1389. E-mail:guo.daqiao@zs-hospital.sh.cn Curative effect analysis of carotid artery stenting in the treatment of carotid angioplasty and stenting with moderate or severe calcification using the distal embolization protected device ZHANG Lu1, TANG Xiao1, FU Wei-guo1, SHI Zhen-yu1, LYU Peng2, DAI Yuan-yuan2, WANG Yu-qi1, GUO Da-qiao1△ (1Department of Vascular Surgery,Zhongshan Hospital,Fudan University-Institute of Vascular Surgery, Fudan University,Shanghai 20032,China;2Department of Radiology,Zhongshan Hospital, Fudan University,Shanghai 200032,China) ObjectiveTo evaluate the safety and efficacy of carotid angioplasty and stenting (CAS) in the treatment of carotid artery stenosis with moderate or severe calcification using the distal embolization protected device.MethodsTwenty-eight carotid artery stenosis patients with moderate or severe calcified plaque accepted CAS using the distal embolization protected device.Patients underwent carotid artery CT angiography before CAS,and magnetic resonance imaging of the brain pre-and post-operatively.We evaluated the relationship between calcified plaque and the rate of immediate postoperative residual stenosis as well as the postoperative new diffusion-weighted lesions.ResultsThe immediate technical success rate was 100% in 28 patients.No death or myocardial infarction occurred during the perioperative period.Fifteen cases (53.6%) of new diffusion-weighted lesions (DWI) occurred according to postoperative cranial MRI.The new diffusion-weighted lesions positive group and negative group were compared.While there was no significant difference in the calcified plaque position,volume,calcium radian(CR) and Agatston calcification score,CT calcification value,calcified plaque volume percentage and thickness between the two groups.Within 12 months after CAS,one patient suffered ischemic stroke on the side of CAS and the remaining 27 patients after CAS recovered well without transient ischemic attacks (TIA) or ischemic stroke.After 1 year,the incidence rate of carotid artery restenosis and stent fracture was zero.ConclusionsWith the distal embolization protected device,carotid artery stenting is a safe and effective treatment for carotid artery stenosis with moderate or severe calcified plaque.The location,volume,CT calcium value,the volume percentage and thickness of calcified plaque have no influence on the occurrence rate of the postoperative new diffusion-weighted lesions and restenosis. carotid artery stenosis;stenting;calcification;new diffusion-weighted lesions;residual stenosis R654.4 Adoi: 10.3969/j.issn.1672-8467.2016.05.006 2016-01-27;编辑:沈玲) * This work was supported by the Foundation of Science and Technology Commission of Shanghai Municipality (074119503) and the National Natural Science Foundation of China (81570433). 上海市科委基金(074119503);国家自然科学基金(81570433)
结 果
讨 论