SWI与ASL联合应用对轻中度急性脑梗死诊断及预后评估的价值
周建国,符大勇,李勇刚
SWI与ASL联合应用对轻中度急性脑梗死诊断及预后评估的价值
周建国1,2,符大勇1,李勇刚2*
目的 探讨3.0 T MR磁敏感加权成像(SWI)与动脉自旋标记成像(ASL)对于急性缺血性脑卒中缺血半暗带(IP)、侧支代偿储备、出血转化(HT)、责任血管及近期预后评估的临床应用价值。材料与方法 35例急性缺血性脑卒中患者行常规MR序列、SWI和3D-PCASL检查,通过软件进行后处理,得出SWI最小密度投影图和3D-ASL伪彩图。观察35例患者梗死核心区周围引流静脉形态学改变,分为引流静脉明显显示组和正常显示组,分别对两组入院当日及15 d NIHSS评分进行分析。将未经溶栓治疗的33例患者,依据3D-ASL伪彩图提示梗死核心区周围是否出现匍匐走行条状高灌注信号,分为侧支代偿组和对照组,并对其入院当日与15 d后NIHSS评分进行分析。依据3D-ASL提示的梗死核心区灌注状态不同,分为高灌注组和低灌注组,结合SWI提示HT的发生率,统计分析梗死核心区不同灌注状态与HT发生之间的关联。结果 梗死区周围引流静脉明显显示组预后好转、稳定及进展比例分别为13/27、6/27和8/27;正常显示组预后好转、稳定及进展比例分别为6/8、2/8和0/8,两组近期预后进展差异有统计学意义(P=0.0432)。侧支代偿组与对照组入院当日NIHSS评分差异无统计学意义(t=0.886,P=0.392),侧支代偿组近期预后好转、稳定及进展比例为13/17、3/17和1/17;而对照组近期预后好转、稳定及进展比例为5/16、4/16和7/16,两组15 d后NIHSS评分差异有统计学意义(t=2.296,P=0.039)。梗死核心高灌注组HT发生比例为6/6,低灌注组HT发生比例为5/29,两组差异有显著统计学意义(P=0.000)。结论 SWI与ASL联合MR常规序列检查,能够更好评估IP范围、侧支循环代偿建立状态、责任血管及HT等相关信息,对于了解急性脑卒中患者缺血梗死现状及近期预后评估提供客观依据。
缺血性脑卒中;动脉自旋标记;磁敏感加权成像;侧支循环
缺血性脑卒中是由于供血动脉发生严重狭窄或闭塞,且侧支循环不够完善,导致其供血区脑血流量减少或阻断,继而引发脑组织缺血缺氧、软化坏死[1]。随着我国老龄人口的日益增多,脑卒中的发病率也逐年递增,现已成为严重的社会公共卫生问题。早期进行客观、准确的影像诊断对于临床治疗方案的选择及预后评估具有重要的临床应用价值。
1 材料与方法
1.1一般资料
收集连云港市中医院2014年12月至2015年12月期间经临床确诊的35例轻中度急性期缺血性脑卒中患者,女13例,男22例;年龄42~80 岁,平均年龄64.5岁,首发症状主要表现为:头晕头痛、偏瘫、偏身麻木及言语不清等。入组标准:(1)符合第四届全国脑血管病会议修订的急性脑梗死诊断标准;(2)临床发病至接受MR检查间隔时间为72 h内;(3)病灶均为单侧发生。排除标准:(1)患者年龄>80岁;(2)昏迷或入院 NIHSS评分>15分;(3)脑干或基底节区腔梗。由神经内科医师采用美国国立卫生研究院卒中量表(National Institute of Health Stroke Scale,NIHSS)于MRI检查当日、15 d后分别对患者进行评分。
1.2检查方法
采用GE Discovery 750 3.0 T MR扫描仪、8通道相控头颈线圈。扫描常规序列包括:T1WI、T2WI 、FLAIR、DWI;SWI扫描参数:TR 37.4 ms,TE 22.9 ms,FOV 24 cm×24 cm,矩阵416×320,层厚2 mm,无间隔,采集次数1次,NEX为0.70次,反转角20°;3D-ASL扫描参数:TR 5369 ms,TE 10.5 ms,FOV24 cm×24 cm,分辨率512×8,激励次数3,标记后延迟时间2500 ms。
1.3数据处理和图像分析
分别将磁敏感加权成像(susceptibility weighted imaging,SWI)和动脉自旋标记(arterial spinlabeling,ASL)数据传输至GE AW4.6工作站,由2名神经放射医师分别将SWI原始数据进行最小密度投影处理(minIP),得到SWI图像,将病变区与同层面镜像区相比较,将引流静脉增多、管径增粗定义为明显显示;引流静脉稀疏、纤细定义为减少显示,两侧引流静脉形态相似定义为正常显示。将3D-ASL原始数据经Functool软件处理后得到全脑(cerebral blood flow,CBF)伪彩图,观察分析缺血梗死区域灌注异常改变,结合DWI选择多处感兴趣区(regionof interest,ROI),每处ROI行3次测量,取其平均值,得出脑血流量(cerebral blood flow,CBF)值,与同层镜面区CBF值相对比得出相对脑血流值(relative cerebral blood flow,rCBF)。参考以往的研究将rCBF值大于1.1定义为高灌注,0.9~1.1定义为正常灌注,小于0.9定义为低灌注[2],当观察结果存在分歧时,引入第三名医师进行评估,经协商后达成一致意见。
依据SWI图像提示梗死核心区周围引流静脉形态差异,将35例患者分为引流静脉明显显示组和正常显示组,分别对两组入院当日及15 d NIHSS评分进行分析。
收集未经临床溶栓治疗的33例患者,依据3D-ASL伪彩图提示梗死核心区周围是否出现条状高灌注分为侧支代偿组和对照组,并将两组入院当日及15 d NIHSS评分进行统计分析。
依据3D-ASL伪彩图提示的梗死核心灌注状态不同,将35例患者分为高灌注组和低灌注组,分析梗死核心灌注状态与出血转化(hemorrhagic transformation,HT)之间的相关性。
1.4统计学分析
采用SPSS 21.0数据分析软件进行分析,两组间比较用配对样本t检验;计数资料采用卡方检验和Fisher确切概率法,计量资料以均数+标准差表示,以P<0.05为差异有统计学意义。
2 结果
2.1梗死核心区周围引流静脉形态改变与近期预后的相关性
具体见表1,图1。
2.2侧支循环代偿状态与近期临床预后的相关性
具体见表2,图2。
2.3梗死核心区灌注状态差异与HT的相关性
具体见表3,图3。
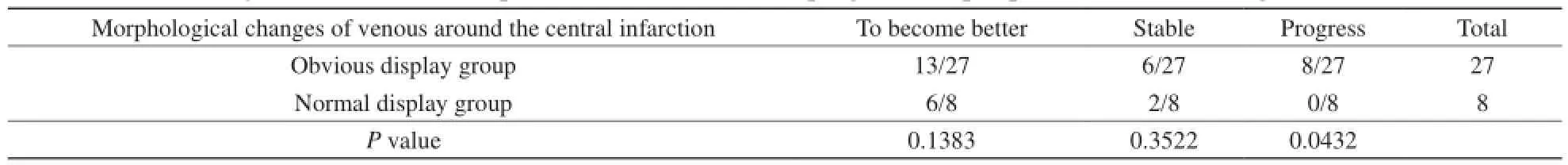
表1 梗死核心区周围引流静脉显示结果与预后关系分析Tab. 1 Analysis of the relationship between the results and prognosis of peripheral venous drainage in the core area
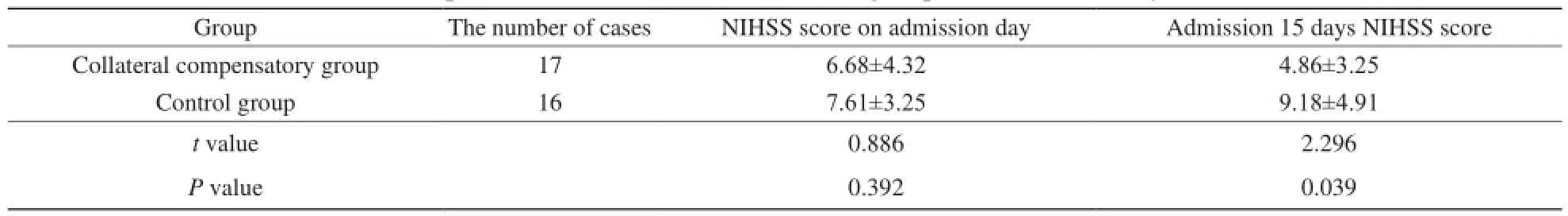
表2 2组入院当日和15 d NIHSS评分比较Tab. 2 Comparison of NIHSS between the two groups on admission day and 15 d
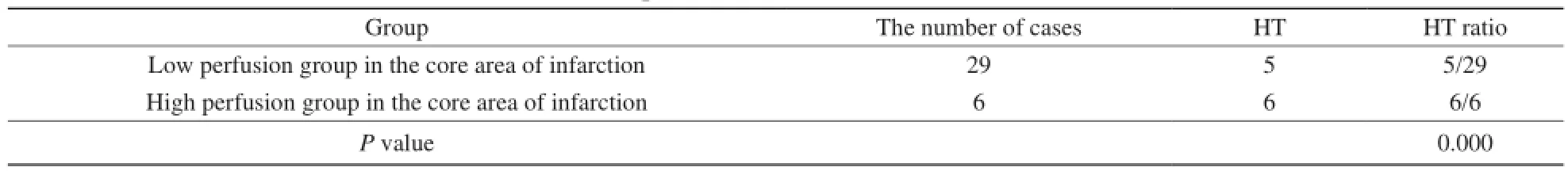
表3 梗死核心区灌注状态与HT相关性Tab. 3 Correlation between perfusion status and HT in the core area of infarction
3 讨论
3.1SWI与ASL联合应用对急性脑梗死IP范围显示的临床应用价值
SWI是一种利用不同组织间磁敏感差异和血氧水平依赖的MRI成像技术,其对血管内顺磁性物质脱氧血红蛋白具有高敏感性。梗死核心区周围血流灌注减少且血氧饱和度较低,但该区域神经细胞仍具有基本代谢功能[3],其通过增加组织氧摄取分数(oxygen extraction fraction,OEF)以代偿细胞血氧需求,随着血管内脱氧血红蛋白含量的增加,SWI图像可提示周围缺血区引流静脉明显显示,借此可通过缺血区细胞氧代谢功能识别缺血区范围。当引流静脉正常显示时,说明该区域血供较为良好,病情较为稳定。梗死核心区的神经细胞由于血流灌注的严重降低导致功能障碍或已经死亡,细胞结构发生破坏,OEF及大脑氧代谢率(cerebral metabolic rate for oxygen,CMRO2)明显降低,导致引流静脉内的脱氧血红蛋白含量减少,SWI图像往往提示引流静脉减少显示。
脑梗死核心区及缺血半暗带(ischemic penumbra,IP)容积的动态变化取决于脑血流灌注的改变。通过15O-PET来评价IP可显示局部脑血液灌注量、rCMRO2及OEF等指标,是目前确定IP范围的金标准[4]。有研究表明采用3D-ASL技术获得的CBF值与PET结果相吻合[5]。ASL作为一种无创性检查方法,利用自体动脉血中自由扩散的水分子作为内源性对比剂,其将流入动脉的血液进行磁化标记,当标记血对组织灌注后行全脑三维快速成像,标记像与未标记像相减影即得到灌注像[6]。并可通过测定CBF值定量单位时间内流经一定量脑组织的血流。ASL在临床应用中能够较为真实可靠地反映缺血梗死区域的低灌注状态[7]。通常将DWI序列提示的高信号区作为判断梗死核心区范围的标准,我们参考以往研究将IP阈值定在18~20 ml/100 g×min,即正常值的30%~40%[8],将ASL伪彩图提示的低灌注区与DWI的不匹配可作为急性期IP存在的影像学依据,IP呈低血流灌注状态,但神经细胞仍维持基本的形态和功能,是急性期溶栓治疗及良好预后的基础。
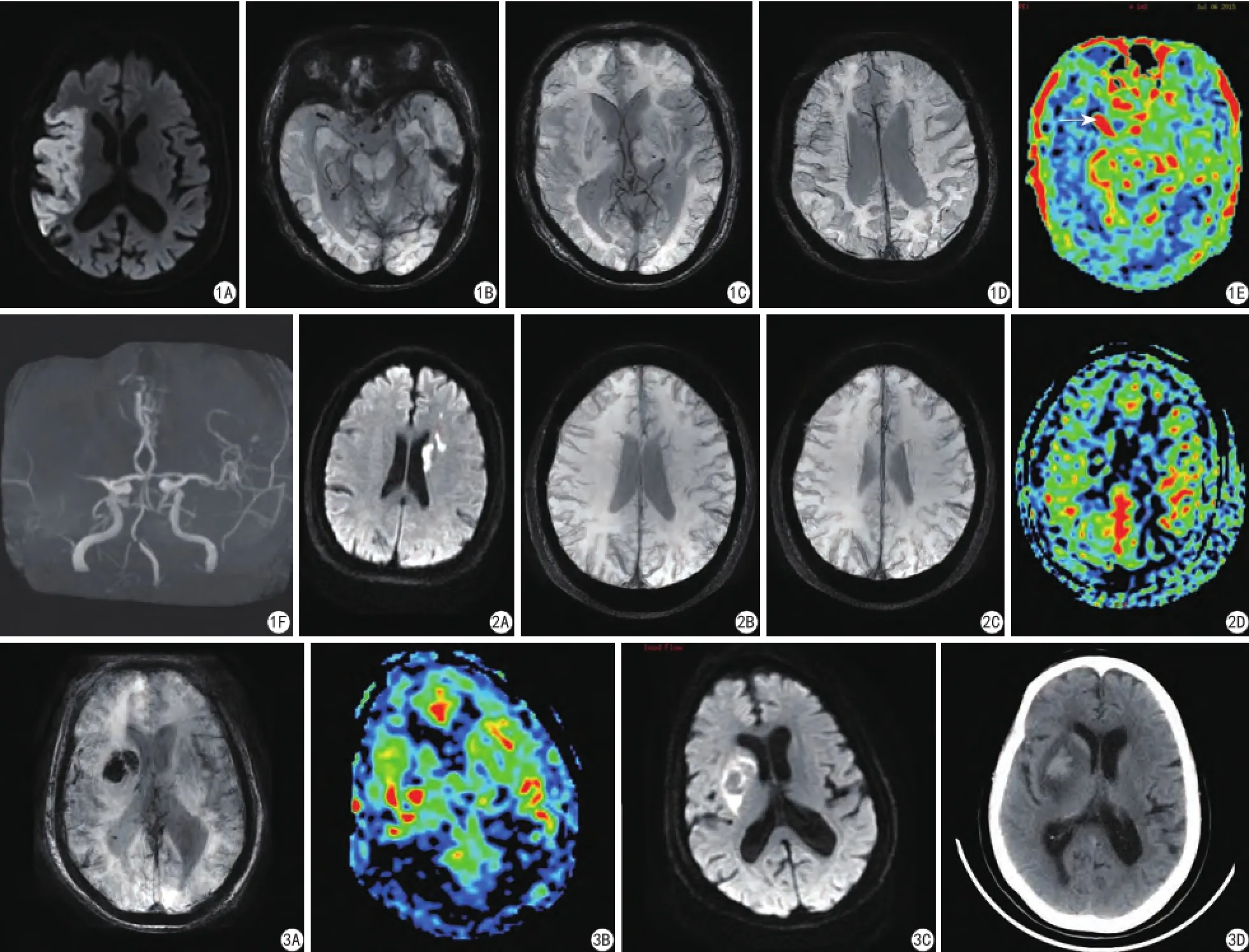
图1 男,80岁,言语不清、左侧肢体不利3 h入院。A:DWI提示右侧额颞顶叶、岛叶急性脑梗死;B:SWI提示右侧大脑中动脉走行区条状低信号(提示血栓);C:SWI提示梗死核心区引流静脉减少显示;D:SWI提示梗死核心区周围引流静脉明显显示;E:ASL提示右侧大脑中动脉走行区条状高灌注(箭提示责任血管血流淤积);F:MRA提示右侧大脑中动脉M1段狭窄 图2 男,68岁,右侧肢体活动不利7 h入院。当日NIHSS评分6分,入院15日NIHSS评分3分,病情好转。A:DWI提示左侧基底节区、脑室旁及额叶急性脑梗死;B、C:SWI提示梗死核心区周围引流静脉明显显示;D:ASL提示梗死核心区周围、匍匐走行条状高灌注 图3 女,78岁,左侧肢体活动不利2 d入院。A:SWI提示右侧基底节区低信号出血转化;B:ASL提示梗死核心区结节状高灌注;C:DWI提示右侧基底节区高信号梗死灶,中央斑片状低信号区;D:CT提示右侧基底节区出血性脑梗死Fig. 1 Male, 80 years old, slurred speech, on the left side of the body adverse 3 hours before admission. A: DWI prompt right frontotemporal and parietal lobe, insula acute cerebral infarction. B: SWI tips right middle cerebral artery area strip low signal (suggesting thrombosis). C: SWI tips in the infarct core area draining vein reduce display. D: SWI tips around the infarction core area draining veins showed obvious. E: ASL tips right middle cerebral artery area strip high perfusion (arrow, prompt responsibility vascular blood fow deposition). F: MRA tips of right middle cerebral artery M1 segment stenosis.Fig. 2 Male, 68 years old, on the right side of physical activity adverse 7 hours admission, the day NIHSS score 6 points, 15 days of admission NIHSS score 3 points, the condition improved. A: DWI tips left basal ganglia and ventricle adjacent frontal acute cerebral infarction. B, C: SWI tips in the infarct core area around the drainage vein showed obvious, prompt in the infarct core area around. D: ASL, creeping line strip high perfusion. Fig. 3 Female, 78 years old, left limbs activity 2 days of admission is unfavourable. A: SWI tips in the right basal ganglia area low signal hemorrhagic transformation. B: ASL tips in the infarct core area nodular high perfusion, prompting the right basal ganglia infarction high signal foci. C: DWI, central patchy low signal zone. D: CT tips right basal ganglia hemorrhage of cerebral infarction.
3.2SWL联合ASL对急性期脑梗死侧支代偿显示的临床应用价值
脑缺血发生后,机体可通过增加OEF,扩张小动脉以及侧支血管吻合来满足缺血组织的血氧需求。Marks等[9]研究显示侧支循环代偿良好的患者其NIHSS评分、最终梗死范围以及溶栓后再灌注情况均明显优于侧支循环不良的患者。通过侧支血管还可使治疗药物最大限度抵达缺血区,陈翠荣的研究认为对于侧支循环良好的患者,临床排除溶栓禁忌,可以适当增宽溶栓时间窗[10]。有研究亦表明ASL与DSC相比能够更敏感显示脑梗死再灌注改变[11]。ASL伪彩图提示的低灌注区周围、皮层及皮层下匍匐条状高灌注信号与侧支循环的建立相关,当血管内的水质子经过冗长的侧支血管到达缺血区后,因T1时间缩短,质子多停留在大血管至微血管水平,未能进入毛细血管网与神经细胞进行血氧交换,结果形成高灌注假象[12],其有别于再通后的高灌注,本研究表明侧支代偿组17例患者,15 d后NIHSS评分预后明显优于对照组,其中5例提示梗死核心区周围引流静脉正常显示,亦提示该区域具有良好的血液供应,患者预后较为良好。
3.3SWI联合ASL对责任血管、血栓显示的临床应用价值
由于急性脑梗死责任动脉血管内的新鲜血栓含有大量脱氧血红蛋白,因此可在SWI图像显示供血动脉内血栓的位置、长度,并可反映血栓的成分[13]。借此亦可区分血栓的不同时间分期,新鲜血栓在SWI图像往往表现为血管走行区条状、斑点状均匀低信号,可较正常血管管径略粗,因其与动脉管壁的结合不够紧密,可作为临床进行动静脉溶栓或血栓清除术的依据[14]。而在脑梗死恢复期,由于血栓内脱氧血红蛋白的减少,纤维胶原成分的增加,于SWI图像上表现为等低混杂信号。同时责任血管内较长的血栓可在阻塞主干的同时,对其分支也可不同程度的累及,这也将影响着脑侧支循环的有效建立[15],对于临床治疗方法的选择及预后的评估亦具有一定的参考意义。3D-ASL伪彩图可因责任血管的阻塞导致血液潴留,于血栓的近心端提示条状高灌注信号,有研究亦说明其与责任血管管腔的严重狭窄或闭塞所引发的血流瘀滞或缓慢相关[16]。本组病例提示3D-ASL伪彩图对于动脉主干闭塞导致的血液瘀滞显示效果较好。
3.4SWI联合ASL对脑梗死后HT显示的临床应用价值
HT是脑梗死常见的并发症,梗死核心区的血液低灌注状态导致血脑屏障的破坏、血管再通引起再灌注损伤是导致HT发生的主要机制[17]。微小出血往往不会导致病情的恶化,然而出血量的增加可能会造成脑梗死后遗症的发生,也是作为目前临床抗凝、溶栓治疗的禁忌证之一。SWI因其对正铁血红蛋白及含铁血黄素的高敏感性,在HT的早期显示能够比CT和2D-GRE T2*WI 更为敏感,较MR常规序列更为准确检出HT的发生,有研究显示SWI序列对于梗死区脑出血的检出率达100%,检出率最高[18]。同时亦可通过SWI图像观察陈旧性出血灶的分布及数量来间接反映卒中患者血管系统的脆弱性,警示临床治疗过程中发生HT的风险。3D-ASL伪彩图亦可通过提示梗死核心区的灌注信息来反映HT的发生,该组核心区高灌注6例患者,病灶区域均发生HT。Wang等[19]研究认为血管再通后的再灌注可增加脑梗死发生HT的风险,血脑屏障严重破坏导致的高灌注,患者预后往往较差,因此ASL提示梗死区高灌注可作为临床溶栓禁忌的一项重要参考指标。
3.5研究不足与展望
本研究采用病例较少,可能会使结论产生偏差,且没有进行长期随访分析。ASL伪彩图提示梗死核心区周围的灌注缺损区包括IP和良性低灌注区,两者分布范围的甄别也需进一步研究,随着MR检查设备及新技术的发展,特别是选择性ASL,流速选择ASL等技术的完善和应用亦可为临床提供更为准确的影像诊断信息,为临床制定个体化、精准化的治疗方案提供参考。
[References]
[1] Jia SL, Wang XM. The diagnosis value of susceptibility-weighted imaging in cerebral ischemic stroke. Chin J Magn Reson Imaging, 2015, 6(3): 182-186.贾素兰, 王晓明. 磁敏感加权成像对脑梗死的诊断价值. 磁共振成像, 2015, 6(3): 182-186.
[2] Xu M, Yang JL, Wu XP, et al. The diagnostic value of ASL and dwi in acute ischemic cerebrovascular disease. Mod Med Imagelogy, 2014, 23(5): 461-465.徐敏, 杨军乐, 邬小平, 等. ASL与DWI在急性缺血性脑血管病中的诊断价值. 现代医用影像学, 2014, 23(5): 461-465.
[3] Lou X, Wu B, Huang DD, et al. In normal adults after circulation of cerebral arterial spin labeling perfusion imaging can repeat research. Chin J Radiol, 2014, 48(2): 151-154.娄昕, 吴冰, 黄点点, 等. 正常成人后循环脑区动脉自旋标记灌注成像的可重复性研究. 中华放射学杂志, 2014, 48(2): 151-154.
[4] Kashef A, Zhao H, chen X. Molecular imaging as the main part of our decision making and treatment strategies in stroke. Front Biosci, 2008, 13(10): 1535-1556.
[5] Bokkers RP, Bremmer JP, van Berckel BN, et al. Arterial spin labeling perfusion MRI at multiple delay times: a correlative study with H(2) (15)O positron emission tomography in patients with symptomatic carotid artery occlusion. J Cereb Blood Flow Metab, 2010, 30(1): 222-229.
[6] Zhang LJ, Xing W, Xing F, et al. Clinical application of arterial spin labeling perfusion imaging in patients with acute cerebral infarction. Jiangsu J Med, 2014, 40(20): 2490-2492.张丽君, 邢伟, 邢飞, 等. 动脉自旋标记灌注成像在急性脑梗死中的临床应用. 江苏医药, 2014, 40(20): 2490-2492.
[7] Zhang SX, Zhang S, Yao YH, et al. Comparative study of threedimension arterial spin labelling (3D-ASL) and bolus contrast perfusion weighted imaging (DSC-PWI) in ischemic stroke patients. Radiol Pract, 2014, 29(8): 901-905.张水霞, 张顺, 姚义好, 等. 3D-ASL与DSC-PWI在缺血性脑梗死患者中的对比研究. 放射学实践, 2014,29(8): 901-905.
[8] Zhang JY, Ni GX. et al. Study of ischemic semi dark band. Chin Archives Tradit Chin Med, 2011, 29(6): 1312-1315.张家英, 倪光夏. 缺血半暗带的研究概况. 中华中医药学刊, 2011, 29(6): 1312-1315.
[9] Marks MP, Lansberg MG, Mlynash M, et al. Effect of collateral blood fow on patients undergoing endovascular therapy for acute ischemic stroke. stroke, 2014, 45(4): 1035-1039.
[10] Chen CR, Zhao ZG, Zhou Y, et al. The study of MRI-based intravenous thrombolysis with broadened therapeutic window for mild-and-moderate acute cerebral infarction. Stroke Neurological Dis, 2014, 21(6): 330-333.陈翠荣, 赵振国, 周媛, 等. 轻中度急性脑梗死MRI指导下超时间窗静脉溶栓治疗的研究. 卒中与神经疾病, 2014, 21(6): 330-333.
[11] Wang DJ, Alger JR, Qiao JX, et al. The value of arterial spin-labeled perfusion imaging in acute ischemic stroke: comparison with dynamic susceptibility contrast-enhanced MRI. Stroke, 2012, 43(4):1018-1024.
[12] Chng SM, Petersen ET, Zinmine I, et al. Territorial arterial spin labeling in the assessment of collateral circulation: comparison with digital subtraction angiography. Stroke, 2008, 39(12): 3248-3254.
[13] Lian KQ, Liu J. The value of susceptibility weighted imaging in diagnosingarterial thrombosis in acute cerebral infarction. Mod Med Imagelogy, 2015, 24(2): 128-131.廉凯茜, 刘筠. 磁敏感加权成像对急性脑梗死动脉血栓的诊断价值. 现代医用影像学, 2015, 24(2): 128-131.
[14] Fujimoto M, Salamon N, Mayor F, et al. Characterization of arterial thrombus composition by magnetic resonance imaging in a swine stroke model. Stroke, 2013, 44(3): 1463-1465.
[15] Sillanpaa N, Saarinen JT, Rusanen H, et al. Location of the clot and outcome fo perfusion defects in acute anterior circulation stroke treated with intravenous thrombolysis. Am J Neuroradiol, 2013, 34(1): 100-106.
[16] Ishimori Y, Kawamura H,Monma M. Feasibility of MR perfusionweighted imaging by use of a time-spatial labeling inversion pulse. Radiol phys Technol, 2013, 6(2): 461-466.
[17] Chen KN, Guo SY, Geng Y. et al. Advance of perfusion imaging in predicting hemorrhagic transformation after thrombolytic therapy for acute ischemic stroke. Chin J Stroke, 2015, 10(2): 165-169.陈珂楠, 郭舜源, 耿昱. 脑灌注成像预测溶栓后出血转化风险的研究进展. 中国卒中杂志, 2015, 10(2): 165-169.
[18] Zhou XF, Wang LW, Yin XD, et al. Application of susceptibility weighted imaging in acute massive cerebral infarction complicated by hemorrhage. Chin J Magn Reson Imaging, 2014, 5(5): 328-331.周星帆, 王利伟, 殷信道, 等. 磁敏感成像序列在急性大面积脑梗死并发出血中的应用. 磁共振成像, 2014, 5(5): 328-331.
[19] Wang DJ, Alger JR, Qiao JX, et al. The value of arterial spin-labeled perfusion imaging in acute ischemic stroke: comparison with dynamic susceptibility contrast-enhanced MRI. Stroke, 2012, 43(4): 1018-1024.
The value of susceptibility weighted imaging combined with arterial spin labeling in diagnosis and prognosis in mild-to-moderate acute ischemic cerebral stroke
ZHOU Jian-guo1,2, FU Da-yong1, LI Yong-gang2*
1Nanjing University of Chinese Medicine Affiliated Lianyungang Hospital and Lianyungang Hospital of Traditional Chinese Medicine, Lianyun-gang 222004, China
2Department of Medical Imaging, the First Pople's Hospital of Suzhou University, Suzhou 215006, China
*Correspondence to: Li YG, E-mail: liyonggang224@163.com
Objective: To study the clinical diagnostic value of 3.0 T magnetic resonance susceptibility weighted imaging (SWI) combined with arterial spin labeling (ASL) in ischemic penumbra (IP), collateral compensatory reserves, hemorrhage transformation (HT), responsible blood vessels and the recent prognosis of patients with acute cerebral infarction. Materials and Methods: Thirty-fve patients with acute ischemic stroke underwent conventional MR sequences, SWI and 3D-PCASL check. Then the SWI minimum intensity projection and 3D-ASL pseudo color pictures were obtained by postprocessing with the software. According to drainage morphological changes around infarction core, 35 cases were divided into the obvious display group and the normal display group. Respectively, the NIHSS score of the two groups on the day of admission and the 15th day was analysed. Thirty-three patients without thrombolytic therapy, according if creeping line strip high perfusion signal existed in the 3D-ASL pseudo color pictures that surrounding the infarction core area, were divided into the collateral compensative group and the control group, and on the day of admission and after 15 d NIHSS scores were analyzed respectively on the day of admission and the 15th day. According to the difference of perfusion state in the infarct core area 3D-ASL suggested, 35 cases were divided into high perfusion group and low perfusion group. Combined with the incidence of HT SWI, the relationship between different perfusion status in the core area of infarction and the occurrence of HT was statistically analysed. Results: The obvious display group showed the prognosis, stability and progress in proportion respectively for 13/27, 6/27 and 8/27, while the normal display group showed that respectively for 6/8, 8 and 0/8, the progress difference of short-term prognosis of two groups was statistically significant (P=0.0432). The NIHSS score difference between the collateral compensative group and the control group was not statistically signifcant (t=0.886, P=0.392). The collateral compensative group showed the recent prognosis improvement, stability and progress in proportion respectively for 13/17, 3/17 and 1/17, while the control group showed that respectively for 5/16, 4/16 and 7/16, and between the two groups after 15 d NIHSS score differences had statistical signifcance (t=2.296, P=0.039). The incidence of HT in the infarction core high perfusion group was 6/6, while the proportion of HT in the low perfusion group was 5/29, and the difference between the two groups was statistically signifcant (P=0.000). Conclusions: MRI imaging combined with ASL as well as SWI, can better evaluate cell oxygen metabolic state, blood perfusion, HT and so on, the IP range, collateral compensatory reserves and short-term prognosis, which provide the basis for clinical diagnosis and treatment.
Ischemic stroke; Aterial spin labeling; Susceptibility weighted imaging; Collateral circulation
5 July 2016, Accepted 16 Aug 2016
1. 南京中医药大学附属连云港市中医院影像科,连云港 222004
2. 苏州大学附属第一医院影像科,苏州 215006
李勇刚,E-mail:liyonggang224@163. com
2016-07-05
接受日期:2016-08-16
R445.2;R743.33
A
10.12015/issn.1674-8034.2016.09.005
周建国, 符大勇, 李勇刚. SWI与ASL联合应用对轻中度急性脑梗死的诊断及预后评估的价值. 磁共振成像, 2016, 7(9): 663-668.