囊性低级别子宫内膜间质肉瘤一例
刘英琦,张静
囊性低级别子宫内膜间质肉瘤一例
刘英琦1,张静2*
作者单位:
1.甘肃中医药大学,兰州大学第二医院西固分院放射科,兰州 730060
2. 兰州大学第二医院磁共振科,兰州 730000
1Gansu University of Chinese Medicine, Department of Radiology, Xigu Hospital of Lanzhou University Second Hospital, Lanzhou 73000, China
2Department of Nuclear Magnetic Resonance, Lan Zhou University Second Hospital, Gansu 730000, China
患者 女,51岁。以“不规则阴道流血、排液1年余,加重2个月”入院。妇科检查:阴道见大量烂肉样组织及淡血性液体,子宫增大如孕5个月,活动度可,有压痛。盆腔MRI平扫描示:子宫增大,宫腔明显扩张,伴多发纤细分隔,呈多房囊状蜂窝样改变,受累肌层不同程度疏松,趋于囊性改变,越近宫腔越明显,宫腔内实性分隔呈T1WI、T2WI等信号,囊性成分T1WI低信号、T2WI高信号,弥散加权成像(diffusion weighted imaging,DWI)高b值(b=800)实性成分呈稍高信号,双侧附件区无异常,盆腔内未见肿大淋巴结(图1A~D)。静脉注入Gd-DTPA后:实性成分明显强化,强化程度同子宫肌层,呈蜂窝样,囊性成分无强化(图1E,F)。MR初步诊断子宫增大,宫内囊性为主占位,结合带显示不清,病变明显强化,多考虑子宫内膜肿瘤。术后病理:内膜,肿瘤细胞,Vimentin(+),CD10(+),ER (3+,90%),SMA(-),Ki-67(+,5%),结合HE切片及免疫组化结果,符合低级别子宫内膜间质肉瘤,肉瘤组织侵犯子宫肌层>1/2层(图2)。
讨论 子宫内膜间质肉瘤(endometrial stromal sarcoma,ESS)是罕见的雌激素依赖性恶性肿瘤,多发生于围绝经期妇女,在子宫肉瘤中占10%,在生殖道恶性肿瘤中仅占0.2%[1]。ESS起源于内膜的间质细胞,沿扩张的淋巴管或血管生长,可来源于原位子宫内膜及相邻肌瘤或肌腺细胞(宫内病变),也可由分布于子宫以外的异位子宫内膜间质发生恶变形成(宫外病变)[2],临床表现主要为盆腔包块,腹痛,阴道不规则出血。ESS的分类首先由Norris和Taylor于1966年提出[3],2014年WHO根据最新的分子研究结果将子宫内膜间质肿瘤分为四类:(1)子宫内膜间质结节(endometrial stromal nodule,ESN);(2)低级别子宫内膜间质肉瘤(low grade endometrial stromal sarcoma,LGESS);(3)高级别子宫内膜间质肉瘤(high grade endometrial stromal sarcoma,HGESS);(4)未分化子宫肉瘤(undifferentiated uterine sarcoma,UUS)[4]。
LGESS按病变部位分为:宫腔型、肌壁型、肌壁间型、浆膜下型和混合型[5],以宫腔型和肌壁间型多见。LGESS宫腔型MR主要表现为子宫增大,宫腔内>5cm的实性肿块;肌壁间型MR主要表现壁结节或肌层内小结节形成,肿块边缘多模糊,部分边缘不规则,联合带和子宫肌层受肿块压迫变薄,有时可中断。肿块信号多不均匀,表现为T1WI等信号,T2WI高信号,DWI明显高信号,肿块可伴有出血、坏死;增强扫描肿块实性部分、间隔明显强化,可呈结节样或网格样强化[6]。镜下特点:肿瘤组织呈不规则舌状或岛状浸润,凸入淋巴管内生长;肿瘤细胞异型性小,核分裂象少见,肿瘤内有丰富的网状纤维和纤细分支状血管网;少数肿瘤可向性索样、平滑肌、横纹肌、上皮样、骨样、腺样或脂肪等分化[7]。多样性分化使肿瘤缺乏典型的生长方式,影像表现不一,是导致诊断困难的主要原因。
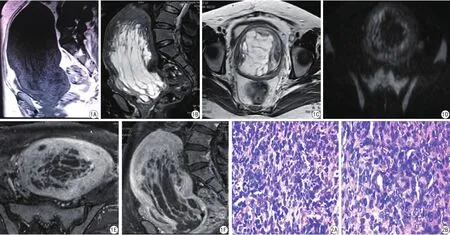
图1 A:T1WI示子宫明显增大,宫腔扩张,病变等或低信号;B:T2WI压脂序列,示病变多发纤细分隔呈等信号,多房囊变呈高信号;C:T2WI序列横断面,示病变多发囊变呈高信号; D:DWI,b=800,示实性部分及分隔稍高信号;E~F:增强扫描,病变实性成分T1WI明显强化,呈蜂窝状 图2 术后病理:内膜(HE ×200)结合切片及免疫组化结果,符合低级别子宫内膜间质肉瘤,肉瘤组织侵犯子宫肌层>1/2Fig. 1 Patient, female, 51 years old. A: T1WI The uterus increased obviously and the height of uterine cavity enlarged such or low signal. B: T2WI-STIR Such signal visible multiple fne separation signal; there were multiple cystic high signal. C: T2WI Multiple cystic lesions with high signal. D: DWI The solid part and the separation of the lesion showed slightly higher signal. E, F: The solid part of the lesion were signifcantly enhanced honeycomb change. Fig. 2 Postoperative pathology: Intima (HE ×200) combined with HE slices and immunohistochemistry results, in accordance with the low grade endometrial stromal sarcoma, sarcomatissue invasion of uterine muscular layer>1/2.
本例患者为绝经期妇女,MR表现为宫腔内蜂窝状囊性占位,其分隔呈纵向分布、蠕虫状改变,具有特征性。临床工作中须与以下子宫肿瘤相鉴别:(1)子宫肌瘤,子宫肌瘤有假包膜,边界清晰,结合带多完整,LGESS结合带多受侵,肿瘤边界不清,T2WI上病变周围有特征性的低信号轮缘。(2)子宫内膜癌,子宫内膜癌相对乏血供,呈渐进性强化,与LGESS早期明显强化可鉴别。(3)子宫腺肌症,子宫腺肌症的子宫肌层弥漫受累,结合带增厚,直径大于1.2 cm,病灶与周围组织边界不清,病变随月经周期而变化。(4)侵袭性葡萄胎,侵袭性葡萄胎多见于育龄期女性,常发生于子宫基层内,宫腔内多发大小不等的T1WI低信号、T2WI高信号结节影,分布不均,呈葡萄串样,在DWI上呈等或稍高信号,伴周围紊乱的血管流空信号,增强扫描宫腔、肌层囊性病灶边缘环形强化,结节多呈中度强化[8],临床HCG明显增高,受其影响,卵巢形成黄化囊肿而增大。
囊性LGESS相对罕见,影像学资料较为缺乏,需要不断收集,进一步学习整理。利用MRI较高的软组织分辨力的优势,不仅能观察到肿瘤的大小、形态及周围组织关系,还能反映肿瘤组织的特征性改变[9],结合临床症状,综合分析可做出诊断。
[References]
[1] Liokumovich P, Goldberg I, Davidson B, et al. Expression of metalloproteinases endometrial stromal sarcoma:immunohistochemical study using image analysis. J Clin Pathol 1999, 52(3): 198-202.
[2] Puliyath G, Nair VR, Singh S. Endometrial stromal sarcoma. Indian J Med Paediatr Oncol, 2010, 31(1): 21-23.
[3] Kang DO, Choi SI, Oh JY, et al. Endometrial stromal sarcoma presented as an incidental lung mass with multiple pulmonary nodules. Tuberc Respir Dis, 2014, 76(3): 131-135.
[4] Ali RH, Rouzbahman M. Endometrial stromal tumours revisited: an update based on the 2014 WHO classification. J Clin Pathol, 2015, 68(5): 325-332.
[5] Chen J, Yang TZ, Yang F, et al. Ultrasonic manifestations of uterine endometrial stromal sarcoma. Chin J Med Imaging Technol, 2014, 30(4): 600-602.陈娇, 杨太珠, 杨帆. 子宫内膜间质肉瘤超声表现. 中国医学影像技术, 2014, 30(4): 600-602.
[6] Liu JJ, Wang J, He BJ, et al. MRI manifestations of endometrial stromal sarcoma: a report of 2 cases and literature review. J Rare Uncom Dis, 2010, 17(2): 31-35.刘静静, 王劲, 何炳均, 等. 子宫内膜间质肉瘤的MRI表现(附2例报告及文献回顾). 罕少疾病杂志, 2010, 17(2): 31-35.
[7] Chen RS, Xiong YQ, Sheng YY, et al. The clinicopathologic analysis of lowgread endometrial stromal sarcoma. Jiangxi Med J, 2010, 45(2): 99-101.陈任生, 熊迎秋, 盛以芸. 低度恶性子宫内膜间质肉瘤临床病例分析. 江西医药, 2010, 45(2): 99-101.
[8] Jing YP, Zhang Y, Cheng JL. MRI diagnosis of gestational trophoblastic diseases with pathologic correlation. Radiol Practice, 2012, 27(3): 333-336.荆彦平, 张焱, 程敬亮, 等. 妊娠滋养细胞疾病的MRI诊断及病理对照. 放射学实践, 2012, 27(3): 333-336.
[9] Xie YH, Fan Y, Zhou Y, et al. Magnetic resonance imaging in diagnosis of ovarian follicular membrane cell tumor: case report. Chin J Magn Reson Imaging, 2016, 7(2): 140-141.谢玉海, 范影, 周燕, 等. 磁共振诊断卵巢纤维卵泡膜细胞瘤一例.磁共振成像, 2016, 7(2): 140-141.
Cystic low grade endometrial stromal sarcoma:one case report
LIU Ying-qi1, ZHANG Jing2*
30 June 2016, Accepted 15 Aug 2016
Endometrial neoplasms; Magnetic resonance imaging
子宫内膜肿瘤;磁共振成像
张静,E-mail:lz2001tong@163.com
*Correspondence to: Zhang J, E-mail: lz2001tong@163.com
2016-06-30 接受日期:2016-08-15
R445.2;R737.33
B
10.12015/issn.1674-8034.2016.09.013