同期胸腹主动脉腔内修复术的临床分析
曾庆龙郭 曦黄小勇吴文辉李铁铮刘光锐孙立忠黄连军*首都医科大学附属北京安贞医院 北京市心肺血管疾病研究所心脏外科,北京 0009首都医科大学附属北京安贞医院 北京市心肺血管疾病研究所介入诊疗科,北京 0009
同期胸腹主动脉腔内修复术的临床分析
曾庆龙1郭 曦2黄小勇2吴文辉2李铁铮2刘光锐2孙立忠1黄连军2*1首都医科大学附属北京安贞医院 北京市心肺血管疾病研究所心脏外科,北京 1000292首都医科大学附属北京安贞医院 北京市心肺血管疾病研究所介入诊疗科,北京 100029
摘要:目的评价同期胸主动脉腔内修复术(thoracic endovascular aortic repair,TEVAR)与腹主动脉腔内修复术(endovascular aortic repair,EVAR)的临床效果,总结经验。方法回顾性分析2010-09—2015-06北京安贞医院大血管诊治中心21例多水平主动脉病变(multilevel aortic diseases,MLAD)患者资料,男性20例,女性1例,年龄54~77岁,平均年龄(65±7)岁。患者术前均行胸腹主动脉CTA明确诊断,于局麻下行同期胸腹主动脉腔内修复术。术后1、3、6个月及每年定期CTA随访。结果手术技术成功率为100%,胸主动脉支架覆盖长度范围为15~27 cm,平均长度为(20.4±4.7)cm。无术后30 d死亡病例,无严重心肺并发症及造影剂肾病发生。2例(9.5%)患者术后出现脊髓缺血表现,予积极升压、静脉大剂量激素及脑脊液引流治疗后缓解。随访2~59个月,1例患者术后半年因为急性主动脉破裂死亡,2例患者分别于术后9个月与48个月出现Ⅰb型内漏,1例植入髂腿延长支架后缓解,1例因为严重合并症行保守治疗。结论同期TEVAR和EVAR为MLAD提供了一种相对安全并且有效的治疗选择。
关键字:多水平主动脉病变;急性主动脉综合征;腔内修复术;脊髓缺血;造影剂肾病
据文献报道,MLAD指同时累及胸降主动脉与腹主动脉的多水平病变,病变性质包括动脉瘤、急性主动脉综合征(Acute aortic syndrome,AAS)(主动脉穿通性溃疡、主动脉壁间血肿及主动脉夹层)等,其中多见腹主动脉瘤合并胸主动脉瘤,有数据显示10%~29%胸主动脉瘤患者合并腹主动脉瘤[1-5]。此外,AAS合并腹主动脉瘤亦不少见[2-8]。目前单一水平主动脉病变的外科治疗经验与日俱增,临床治疗效果满意。但是多发主动脉病变的处理依然棘手,胸腹主动脉病变广泛,需要更大的手术范围和可能2次手术,预示手术并发症的发生率和死亡率更高,尤其对合并AAS的MLAD患者治疗更具有挑战性[9-11]。近20年来,TEVAR与EVAR在临床广泛应用,彻底革新了主动脉病变的治疗策略,成为传统主动脉疾病开放手术之外的重要选择,甚至首选[12-14]。对北京安贞医院21例同期TEVAR与EVAR治疗MLAD患者资料进行回顾性分析,总结其治疗经验。
1 对象和方法
1.1对象
2010-09—2015-06北京安贞医院大血管诊治中心行同期TEVAR与EVAR治疗MLAD患者21例,男性20例,女性1例,年龄54~77岁,平均年龄为(65±7)岁。患者均术前行全主动脉CTA明确诊断和评估腔内治疗的可行性。胸主动脉病变均为动脉瘤4例,AAS 17例,包括单纯主动脉穿通性溃疡8例,其中2例发生破裂,主动脉壁间血肿合并穿通性溃疡6例,B型主动脉夹层3例。胸痛13例,腹痛4例,主动脉破裂2例。所有患者腹主动脉病变为腹主动脉瘤,瘤体直径为5.9~10 cm。临床合并症方面,高血压19例,冠心病5例,脑梗死4例,肾功能不全3例,糖尿病2例,长期吸烟史9例。
1.2方法
所有患者均在局部麻醉下,外科游离或者经皮穿刺股动脉入路,行同期TEVAR与EVAR术。2例患者发生胸主动脉破裂,行急诊腔内修复术,余患者均在予药物保守治疗后于亚急性期(发病2周~2个月)进行治疗。术中常规行主动脉造影明确病变,同时评估支架锚定区与入路血管解剖条件。治疗顺序方面,一般先行TEVAR以隔绝更为凶险的胸主动脉病变,再行EVAR,以此保证腹主动脉支架的稳定性,并且规避因为先进行EVAR后进行TEVAR造成入路困难的风险。该组仅有1例患者因为双侧髂动脉多发狭窄,考虑先行EVAR,以重建入路后行TEVAR。维持术中及术后血压>130/80 mm Hg(1 mm Hg =0.133 kPa),术后低分子肝素抗凝,静点大剂量激素,预防性脑积液引流,以减轻脑脊液压力,增加脊髓灌注,预防脊髓缺血。此外,围手术期生理盐水充分水化扩容,术中合理运用造影剂的量,围手术期监测肾功能,以预防造影剂肾病的发生。
在支架使用方面因为胸主动脉病变长而广泛,6例需要2枚支架置入,余15例置入1枚支架。胸主动脉支架类型包括6枚Zenith TX2(COOK,Denmark),7枚Valiant (Medtronic,USA),3枚Ankura (Lifetech,China),6枚E-vita(Jotec,Germany),4枚Hercules(Microport,China)和1枚Grikin(GRIKIN,China)。腹主动脉支架系统包括4 枚Zenith Flex(COOK,Denmark),8枚Endurant(Medtronic,USA),3枚Excluder(Gore,USA)和6枚Hercules(Microport,China)。
1.3随访及统计学分析
随访时间为术后1、3、6、12个月,之后每年均进行全主动脉CTA随访,观察支架位置、形态及内漏等支架相关并发症。本组患者均获得随访,随访时间为2~59个月。采用IBM SPSS 21.0软件包进行统计学分析。计量资料的平均数采用(x±s)表示。
2 结果
本组手术技术成功率为100%,手术110~240 min,平均手术时间为(157.6±45.6)min;住院4~30 d,平均住院时间为(10.7±4.9)d。胸主动脉支架覆盖长度15~27 cm,平均覆盖长度为(20.4±4.7)cm。因为近端锚定区不足(<15 mm),同期行烟囱术重建左锁骨下动脉2例,重建单侧最低肾动脉2例(图1);3例患者髂总动脉瘤样扩张,分别行左侧髂内动脉、右侧髂内动脉及双侧髂内动脉封闭。无术后30 d死亡病例,无严重心肺并发症及造影剂肾病发生。2例(9.5%)患者术后即出现脊髓缺血,表现为双下肢轻瘫,肌力减退(4级),二便无障碍,予积极升压、静脉大剂量激素及脑脊液引流治疗,术后肌力逐渐恢复(5级-),回归日常生活。随访2~59个月,平均随访时间为(25.9±17.6)个月。1例患者术后半年发生急性主动脉破裂死亡。2例患者分别于术后9个月与48个月因为右侧髂动脉扩张,发生Ⅰb型支架内漏,1例植入髂腿延长支架后缓解,1例因合并严重的冠心病行保守治疗。
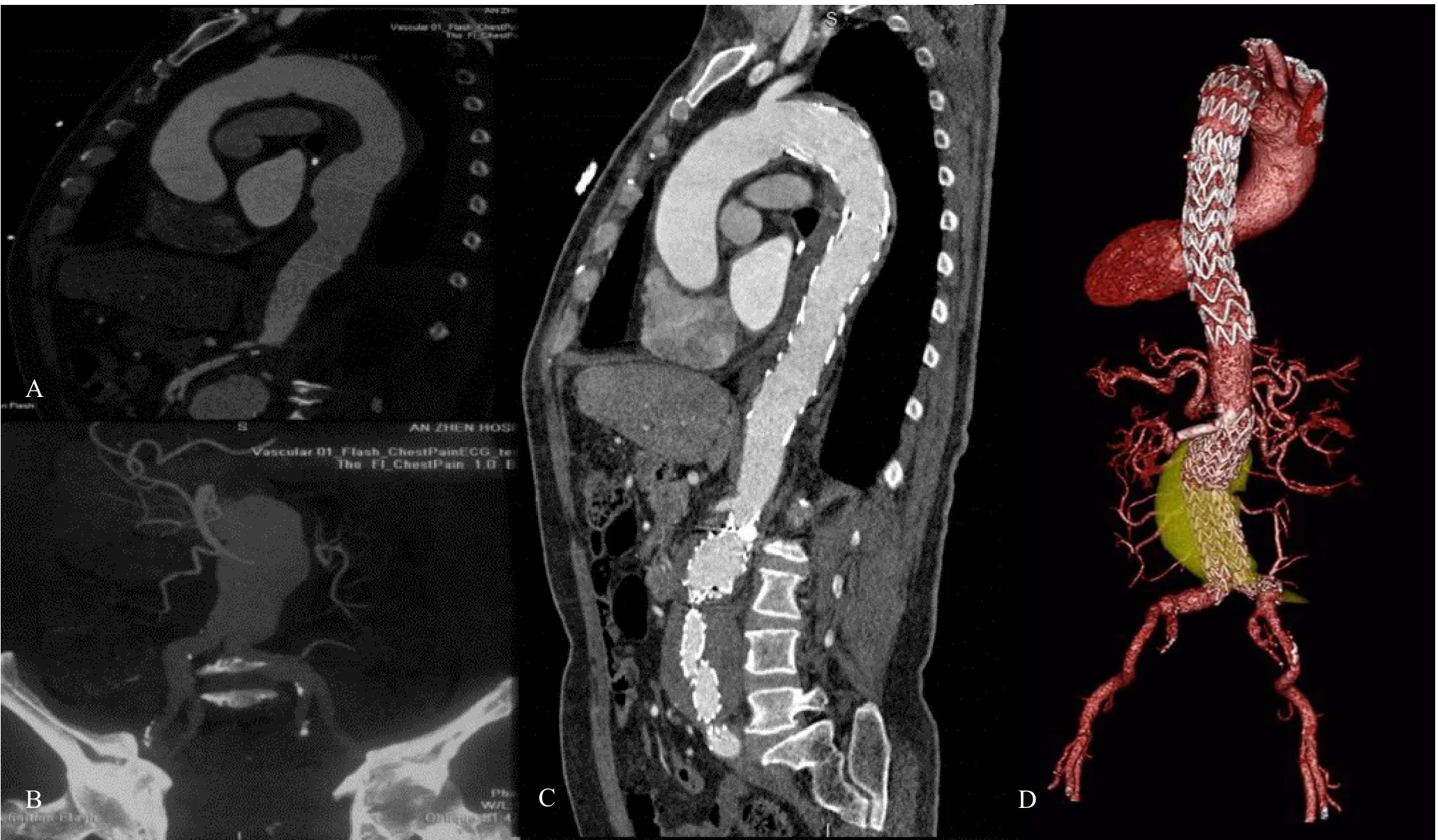
图1 患者,男性,76岁,因“胸痛1个月”入院治疗
3 讨论
在组织学与解剖学上,主动脉自胸段至腹段存在差异,但是临床逐渐将主动脉视为心血管系统中一个整体的器官[15]。在退行性病变、动脉粥样硬化、遗传因素及炎症等相同背景下,主动脉多水平均可受累。病理性质涵盖动脉瘤、穿通性溃疡、主动脉壁间血肿及动脉夹层等,其中以动脉瘤多见[1-5,16-18]。MLAD确切发生率及组成比例尚无流行病学调查报道。一项纳入4320例胸或者腹主动脉疾病患者的多中心试验研究数据[3]显示,1.8%患者有MLAD,其中胸主动脉病变中动脉瘤占68.8%,动脉夹层占18.1%,溃疡占12.9%。而在本组报道的MLAD患者胸主动脉病变中仅有4例动脉瘤,余17例为AAS(包括单纯主动脉穿通性溃疡8例,其中2例发生破裂;主动脉壁间血肿合并穿通性溃疡6例;B型主动脉夹层3例)。但是腹主动脉病变均为动脉瘤。术前全主动脉CTA检查是发现MLAD的必要手段,有利于整体评估主动脉病变及解剖条件,决定腔内治疗策略[15]。
目前MLAD研究仅局限于个案或者小样本病例报道,其治疗策略尚缺乏临床指南建议。早期采取多水平主动脉开放手术治疗,可以分期或者同期进行[9-11]。分期手术患者需要经受2次手术,并且难以预估在手术间隔期间残余主动脉病变的破裂风险。而同期手术,理论上会带来更高手术并发症和死亡风险。但是有研究显示,保守治疗后3年与7年的生存率分别为48%与12%,单纯胸或者腹主动脉水平的外科手术生存率为48%与12%,同期胸腹主动脉病变外科手术则分别为64%与34%,其结果提示同期外科手术的早期与远期治疗结果似乎更佳[10,11,16-18]。同期胸腹主动脉开放手术极具挑战性,创伤巨大,心肺并发症风险极高,尤其对合并心肺疾病的高危患者存在禁忌。
近20多年,腔内修复术彻底革新了主动脉疾病的治疗策略,凭借其微创,低并发症发生率和死亡率的优势,逐渐在主动脉疾病治疗中崭露头角[12-14]。有学者在外科高危患者中,尝试运用杂交手术、分期或者同期腔内修复治疗MALD,其临床效果满意,而其严重并发症发生率并未明显增加。有关同期TEVAR与EVAR应用于MLAD文献资料[2-5,18]显示,胸主动脉病变以动脉瘤多见,ASS仅占小比例,治疗结果提示患者短中期随访(范围1~108个月)、生存率(75%~100%)及2次干预率(0~25%)尚可以接受。本组研究胸主动脉病变以AAS为主(占80.9%),临床诊治更为迫切,但是治疗结果却与文献报道相符,随访期间生存率为95.2%,2次干预率为4.8%。综合文献研究与本中心研究结果,有理由认为同期TEVAR和EVAR是MLAD治疗的有效方法,甚至对合并AAS患者,其技术成功率与生存率较高。
脊髓缺血一直是主动脉腔内修复术严重的并发症之一,下肢轻瘫或者截瘫,严重影响生活质量[19]。主动脉腔内修复术避免了在开放手术中主动脉阻断与体外循环等有创操作,但是同时直接覆盖了脊髓供血动脉,使脊髓缺血风险增加。在腔内治疗过程中,脊髓缺血的危险因素包括主动脉长段覆盖、左侧锁骨下动脉覆盖、围手术期低血压、既往腹主动脉置换或者有腔内治疗病史等[20]。MLAD腔内治疗需要胸段与腹段主动脉同时覆盖,肋间动脉、腰动脉大量丢失,明显增加了脊髓缺血的风险。文献报道同期胸腹主动脉腔内治疗后脊髓缺血的发生率达0~13.6%,本组研究2例(9.5%)出现脊髓缺血,表现为双侧下肢轻瘫,肌力减退(4级),二便无障碍。其中1例胸主动脉覆盖长度为250 mm,术中发生短暂性低血压(平均血压<50 mm Hg)。对于预防和治疗脊髓缺血,作者建议如下[21,22]:⑴ 避免左侧锁骨下动脉覆盖,必要时行烟囱术或者转流术重建;⑵ 在隔绝病变基础上尽可能保留低位肋间动脉;⑶ 维持术中及术后血压≥130/80 mm Hg,保证脊髓灌注;⑷ 术后常规抗凝及静脉予大剂量激素治疗,减轻脊髓缺血损伤及炎症反应。同时监测脑脊液压力,脑积液引流(<10 ml/h),维持脑脊液压力<18 cm H2O。本组脊髓缺血患者在经过积极升压、抗凝、静脉大剂量激素及脑脊液引流治疗后症状逐渐缓解。
造影剂肾病是医院获得性急性肾衰竭的重要原因,约50%病例是心血管介入手术所致[23]。在同期TEVAR与EVAR术中有更多的造影剂运用,造影剂肾病的风险增加,尤其术前肾功能不全者[24,25]。围手术期充分水化,合理优化选用造影剂和剂量,并且动态监测肾功能,可以有效预防和早期处理造影剂肾病[25]。本组研究患者围手术期监测肾功能,无造影剂肾病并发症病例。
总之,同期TEVAR与EVAR为MLAD提供了另一种有效的治疗选择。本研究报道了一组MLAD患者的同期腔内治疗结果,近中期临床治疗效果满意。本组研究样本量小,随访期短,尚需要长期、大样本研究。
参考文献
[1]Aguiar Lucas L, Rodriguez-Lopez JA, Olsen DM, et al. Endovascular repair in the thoracic and abdominal aorta: no increased risk of spinal cord ischemia when both territories are treated. J Endovasc Ther, 2009, 16: 189-196.
[2]Xanthopoulos DK, Papakostas JC, Arnaoutoglou HM, et al. Simultaneous endovascular stent-graft repair of descending thoracic and abdominal aortic pathologies. Report of four cases. Int Angiol, 2010, 29: 273-277.
[3]Piffaretti G, Bonardelli S, Bellosta R, et al. Spinal cord ischemia after simultaneous and sequential treatment of multilevel aortic disease. J Thorac Cardiovasc Surg, 2014, 148: 1435-1442.
[4]Scali ST, Feezor RJ, Chang CK, et al. Safety of elective management of synchronous aortic disease with simultaneous thoracic and aortic stent graft placement. J Vasc Surg, 2012, 56: 957-964.
[5] Kirkwood ML, Pochettino A, Fairman RM, et al. Simultaneous thoracic endovascular aortic repair and endovascular aortic repair is feasible with minimal morbidity and mortality. J Vasc Surg, 2011, 54: 1588-1591.
[6]Joyce JW, Fairbairn JF, Kincaid OW, et al. Aneurysms of the Thoracic Aorta. A Clinical Study with Special Reference to Prognosis. Circulation, 1964, 29: 176-181.
[7]de Bakey ME, McCollum CH, Graham JM. Surgical treatment of aneurysms of the descending thoracic aorta: long-term results in 500 patients. J Cardiovasc Surg (Torino), 1978, 19: 571-576.
[8]Pressler V, McNamara JJ. Thoracic aortic aneurysm: natural history and treatment. J Thorac Cardiovasc Surg, 1980, 79: 489-498.
[9]Gloviczki P, Pairolero P, Welch T, et al. Multiple aortic aneurysms: the results of surgical management. J Vasc Surg, 1990, 11: 19-27; discussion 27-28.
[10]Crawford ES, Cohen ES. Aortic aneurysm: a multifocal disease. Presidential address. Arch Surg, 1982, 117: 1393-1400.
[11]Davies RR, Goldstein LJ, Coady MA, et al. Yearly rupture or dissection rates for thoracic aortic aneurysms: simpleprediction based on size. Ann Thorac Surg, 2002, 73: 17-27; discussion 27-28.
[12]Dake MD, Miller DC, Semba CP, et al. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med, 1994, 331: 1729-1734.
[13]Dake MD, Kato N, Mitchell RS, et al. Endovascular stentgraft placement for the treatment of acute aortic dissection. N Engl J Med, 1999, 340: 1546-1552.
[14] Schermerhorn ML, Buck DB, O'Malley AJ, et al. Long-Term Outcomes of Abdominal Aortic Aneurysm in the Medicare Population. N Engl J Med, 2015, 373: 328-338.
[15]Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J, 2014, 35: 2873-2926.
[16]Moon MR, Mitchell RS, Dake MD, et al. Simultaneous abdominal aortic replacement and thoracic stent-graft placement for multilevel aortic disease. J Vasc Surg, 1997, 25: 332-340.
[17]Meguid AA, Bove PG, Long GW, et al. Simultaneous stentgraft repair of thoracic and infrarenal abdominal aortic aneurysms. J Endovasc Ther, 2002, 9: 165-169.
[18]Castelli P, Caronno R, Piffaretti G, et al. Endovascular repair for concomitant multilevel aortic disease. Eur J Cardiothorac Surg, 2005, 28: 478-482.
[19]DeSart K, Scali ST, Feezor RJ, et al. Fate of patients with spinal cord ischemia complicating thoracic endovascular aortic repair. J Vasc Surg, 2013, 58: 635-642.
[20]Ullery BW, Cheung AT, Fairman RM, et al. Risk factors, outcomes, and clinical manifestations of spinal cord ischemia following thoracic endovascular aortic repair. J Vasc Surg, 2011, 54: 677-684.
[21]黄小勇,黄连军,郭曦,等. “两段式” 覆膜支架置入术个性化治疗Stanford B 型主动脉夹层的效果[J]. 中华心血管病杂志,2015,43(1):39-43 .
[22]郭曦,黄小勇,李彭,等. 覆膜支架长段覆盖降主动脉实施腔内修复术对脊髓血供的影响[J]. 中华胸心血管外科杂志,2014,30(009):539-542.
[23] Detrenis S, Meschi M, Bertolini L, et al. Contrast medium administration in the elderly patient: is advancing age an independent risk factor for contrast nephropathy after angiographic procedures? J Vasc Interv Radiol, 2007, 18: 177-185.
[24]Tepel M, Van der Giet M, Schwarzfeld C, et al. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med, 2000, 343: 180-184.
[25]Tepel M, Aspelin P, Lameire N. Contrast-induced nephropathy: a clinical and evidence-based approach. Circulation, 2006, 113: 1799-1806.
A clinical study of simultaneous thoracic endovascular aortic repair and endovascular aortic repair
ZENG Qing-long1GUO Xi2HUANG Xiao-yong2WU Wen-hui2LI Tie-zheng2LIU Guang-rui2SUN Li-zhong1HUANG Lian-jun2*
1Department of heart Institute, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart Lung and Blood Vessel Diseases, Beijing 100029,China
2Department of Interventional Diagnosis and Treatment, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart Lung and Blood Vessel Diseases, Beijing 100029, China
Abstract:ObjectiveTo evaluate the efficacy of simultaneous thoracic endovascular aortic repair (TEVAR) and endovascular aortic repair (EVAR) and to summarize our experience. MethodsA total of 21 patients (20 men; mean 65±7 years, range 54-77) underwent simultaneous TEVAR and EVAR between Sept 2010 and Jun 2015 at a single center were retrospectively reviewed. All patients were diagnosed with concomitant thoracic aortic diseases (aneurysm and acutebook=12,ebook=16aortic syndrome) and abdominal aortic aneurysm (AAA) by preoperative CTA. Local anesthesia, perioperative relative high arterial pressure (above 130/80 mm Hg) control, perioperative hydration and preventive high-dose corticosteroid were given to all cases, 2 of whom received an emergent simultaneous endovascular repair. All patients were followed up postoperative 1 month, 3 month, 6 months, and yearly thereafter. Technique success, procedure related complications were evaluated. ResultsThe technical success rate was 100%. The length of thoracic coverage was 20.4±4.7 cm (range 15-27). All patients got survival postoperative 30 days. No patients developed acute cardiopulmonary complications and contrast induced nephropathy. 2 patient developed transient lower extremity weakness that resolved with blood pressure elevation, cerebrospinal fluid drainage and intravenous drip high-dose corticosteroid. Over 2 to 59 months follow up, 1 patient was died of aneurysm rupture at postoperative 6 month, 2 patients developed type Ⅰb endoleak at postoperative 9 month and 48month respectively, one patient was successfully sealed by iliac stent-graft extension, the other received conservative treatment. ConclusionCombined TEVAR and EVAR can be performed successfully in cases with multilevel aortic diseases (MLAD). When anatomically feasible, simultaneous TEVAR and EVAR can be considered as a feasible and safe alternative to MLAD.
Keywords:multilevel aortic diseases; acute aortic syndrome; endovascular aortic repair; spinal cord ischemia; contrast induced nephropathy
*通信作者:黄连军,E-mail:huanglianjun2008@163.com
文章编号:2096-0646.2016.02.01.03