心肌灌注显像联合冠状动脉钙化积分一站式检查对冠心病的诊断价值
One-step Examination of Myocardial Perfusion Imaging Combined with Coronary Artery Calcium Score in Diagnosis of Coronary Artery Disease
王建锋1 WANG Jianfeng袁建伟2 YUAN Jianwei王跃涛1 WANG Yuetao周瑞珏3 ZHOU Ruijue杨 玲3 YANG Ling邵晓梁1 SHAO Xiaoliang陆培奇1 LU Peiqi
心肌灌注显像联合冠状动脉钙化积分一站式检查对冠心病的诊断价值
One-step Examination of Myocardial Perfusion Imaging Combined with Coronary Artery Calcium Score in Diagnosis of Coronary Artery Disease
王建锋1WANG Jianfeng
袁建伟2YUAN Jianwei
王跃涛1WANG Yuetao
周瑞珏3ZHOU Ruijue
杨玲3YANG Ling
邵晓梁1SHAO Xiaoliang
陆培奇1LU Peiqi
【摘要】目的 心肌灌注显像(MPI)联合冠状动脉钙化积分(CACS)一站式检查可同时获得冠状动脉功能信息和解剖信息,本研究探讨MPI联合CACS一站式检查对冠心病(CAD)的诊断价值。资料与方法回顾性分析行MPI联合CACS一站式检查及冠状动脉造影(ICA)的188例可疑CAD患者,以ICA结果作为诊断 “金标准”,分析MPI、CACS及两者联合对CAD的诊断效能。结果①188例疑似CAD患者中CAD验前概率中度可能者150例(79.8%),高度可能者38例(20.2%)。ICA诊断为CAD 73例,非CAD 115例。②MPI诊断CAD的敏感度、特异度、准确度、阳性预测值、阴性预测值分别为65.8%、75.7%、71.8%、63.1%、77.7%。③CAD组CACS明显高于非CAD组[(494.96±99.60)分比(38.15±16.03)分,P<0.05]。根据受试者操作特征曲线,CACS诊断CAD的最佳界值为96.45分,以CACS≥96.45分作为诊断CAD的标准,其诊断CAD的敏感度、特异度、准确度、阳性预测值、阴性预测值分别为60.3%、93.9%、80.8%、86.3%、78.8%。④MPI联合CACS诊断CAD的敏感度高于MPI(80.8%比65.8%,P<0.05),其特异度(71.3%比75.7%)和准确度(75.0%比71.8%)差异无统计学意义(P>0.05);MPI联合CACS诊断CAD的敏感度高于CACS(80.8%比60.3%,P<0.05),特异度低于CACS(71.3% 比93.9%,P<0.05),其诊断准确度(75.0%比80.8%)差异无统计学意义(P>0.05)。结论MPI联合CACS一站式检查可减少单用MPI或CACS对CAD的漏诊,提高CAD的诊断敏感度,对CAD中度可能患者的诊断具有重要价值。
【关键词】冠心病;体层摄影术,发射型计算机,单光子;体层摄影术,X线计算机;99m锝甲氧基异丁基异腈;心肌再灌注;钙质沉着症;冠状血管造影术
论著Original Research
作者单位
1. 常州市第一人民医院核医学科江苏常州213003
2. 广东药学院附属第一医院核医学科广东广州510080
3. 常州市第一人民医院心内科江苏常州213003
Department of Nuclear Medicine, Changzhou First People's Hospital, Changzhou213003, China
Address Correspondence to: WANG Yuetao
E-mail: yuetao-w@163.com
江苏省卫生厅科技项目(H201349);广东省科技计划项目(2012B031800322);常州市科技支撑-社会发展项目
(CE20135063)。
R541.4;R445.6
修回日期:2015-11-18
中国医学影像学杂志
他们性格迥然,爱好有别,但对市场、生存、竞争天生敏感,绝不含糊。他们能够忍受:高强度工作、长时间压力、不确定风险。
2016年 第24卷1期:12-15,25
冠心病(coronary artery disease,CAD)是冠状动脉病变导致心肌缺血、缺氧引起的心脏病,目前缺血性心脏病死亡率每年上升幅度已居各类心血管病死亡率首位[1],如何早期、准确诊断CAD是目前关注的焦点。心肌灌注显像(myocardial perfusion imaging,MPI)作为诊断CAD的一种无创功能影像检查,能直接反映是否发生心肌缺血及心肌缺血的范围、程度,但不能显示冠状动脉解剖形态学改变,其诊断CAD存在一定的假阳性和假阴性[2]。冠状动脉钙化积分(coronary artery calcium score,CACS)对发现冠状动脉粥样硬化、了解斑块分布及诊断CAD有重要价值[3],但其无法评价冠状动脉血流动力学变化,不能提供心肌细胞血流灌注等信息。MPI联合CACS一站式检查可同时获得冠状动脉功能信息和解剖信息,但目前国内外关于MPI联合CACS诊断CAD的研究较少,其应用价值尚无定论。本研究探讨MPI联合CACS对CAD的诊断效能,探讨其与单用MPI、CACS检查相比是否具有增益价值。
1 资料与方法
1.1研究对象 回顾性分析2010年12月—2014年8月于常州市第一人民医院和佛山市第一人民医院因胸闷、胸痛就诊并行MPI联合CACS一站式检查及冠状动脉造影(ICA)的188例可疑CAD患者,其中男128例,女60例,平均年龄(60.02±9.20)岁。排除标准:①既往有明确心肌梗死病史;②冠状动脉支架植入术后或冠状动脉搭桥术后;③严重心律失常;④血浆肌钙蛋白测试阳性;⑤年龄<18岁;⑥孕妇。参照Wolk等[4]的方法,根据年龄、性别及临床症状对188例可疑CAD患者进行CAD验前概率风险评估。
1.2仪器与方法 采用Siemens Symbia T16型SPECT/CT仪,显像剂为99锝m-甲氧基异丁基异腈(99Tcm-MIBI),放化纯>95%,注射剂量为740~1110 MBq。检查前停用β受体阻滞剂、硝酸酯类等影响心率或扩张冠状动脉的药物。MPI采集条件:平行孔低能高分辨准直器,矩阵128×128,放大倍数1.45,双探头成90°,各旋转90°,共180°采集,6°/帧,每帧采集35 s,门控采集将每个心动周期分为8帧。采用Butterworth函数滤波反投影重建后,得到心脏短轴、水平长轴和垂直长轴图像。CACS采用横轴位平扫,采用回顾性心电门控技术,在60%~80% R-R间期采集数据。扫描参数:管电压130 kV,电流100 mAs,层厚3 mm,扫描范围约20 cm。
1.3图像分析由2名以上核医学医师共同判读同机MPI和CACS图像结果。心肌放射性分布采用17节段法,MPI图像上同一节段心肌连续2个或2个以上层面、2个轴向同时存在放射性分布稀疏或缺损为阳性,MPI表现为可逆性放射性分布减低或缺损、固定性放射性分布减低或缺损者分别诊断为心肌缺血、心肌梗死,均定义为CAD。
1.4CACS评分使用Agatston自动分析软件,并将各支血管钙化灶记分之和得出该血管钙化总积分;冠状动脉分支的观察按解剖学定义分4大支:即左主干、左前降支、左回旋支和右冠状动脉,其中对角支的钙化归入左前降支,钝缘支的钙化归入左回旋支。采用受试者操作特征(ROC)曲线确定CACS诊断CAD的界值,MPI联合CACS诊断CAD的标准为两者其一为阳性,两者均为阴性则排除CAD。
1.5统计学方法采用SPSS 17.0软件,计量资料比较用成组资料t检验,计数资料比较采用χ2检验;以ICA显示冠状动脉狭窄≥50%为诊断CAD的“金标准”,依据ROC曲线获得CACS诊断CAD的最佳界值,计算MPI联合CACS与单用MPI和CACS诊断CAD的敏感度、特异度、准确度、阳性预测值、阴性预测值,P<0.05表示差异有统计学意义。
2 结果
2.1概率风险评估188例患者中,CAD中度可能150例(79.8%),高度可能38例(20.2%)。以ICA显示冠状动脉狭窄程度≥50%作为诊断CAD的标准,其中73例诊断为CAD,115例非CAD。
2.2MPI诊断CAD的效能188例患者中,MPI诊断CAD 76例,非CAD 112例,其诊断CAD的效能见表1、2。
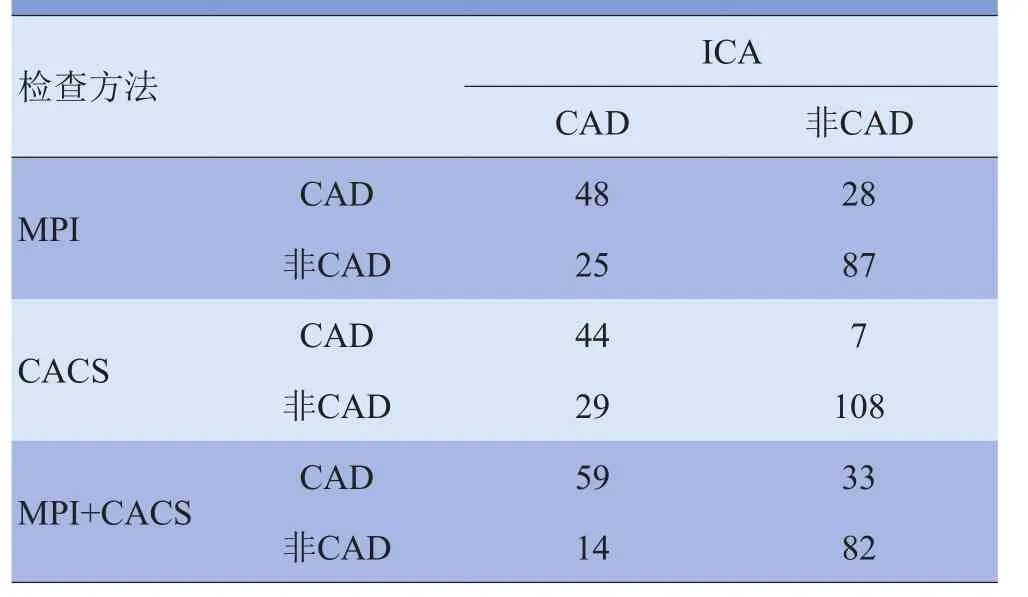
表1 MPI、CACS及两者联合诊断CAD与ICA结果比较(例)
2.3CACS诊断CAD的效能CAD组CACS为(494.96± 99.60)分,明显高于非CAD组的(38.15±16.03)分,差异有统计学意义(t=4.528,P<0.05)。188例患者中,105例CACS=0分,83例CACS>0分。ROC曲线(图1)显示,当CACS为96.45分时,其对CAD的诊断效能最高,曲线下面积为0.81。以CACS≥96.45分作为诊断CAD的标准,其诊断CAD的效能见表2。
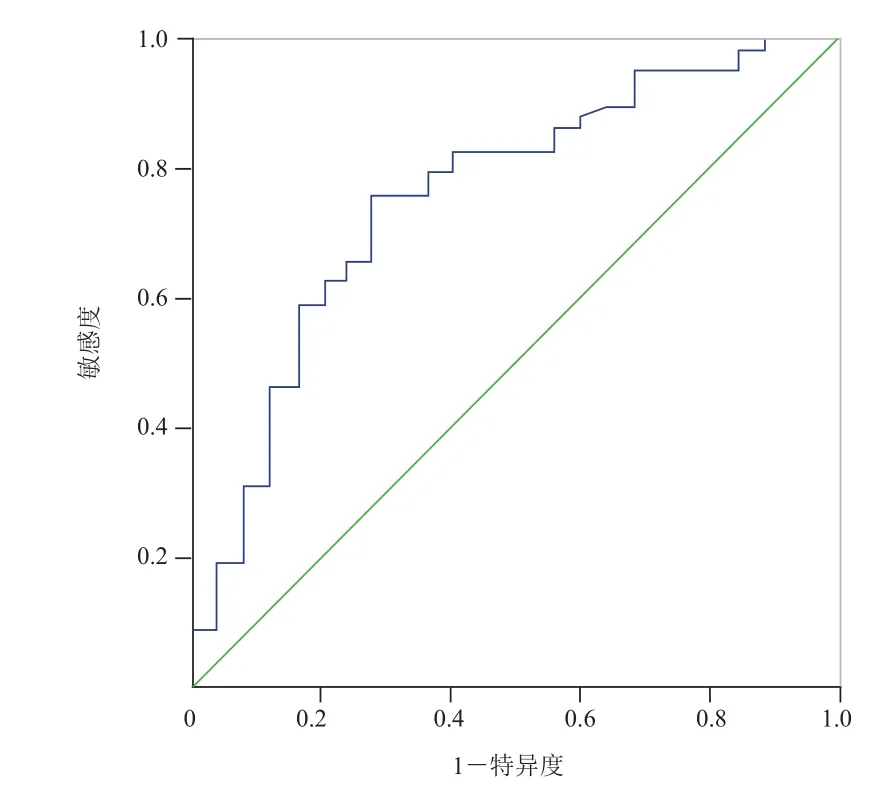
图1 CACS诊断CAD的ROC曲线
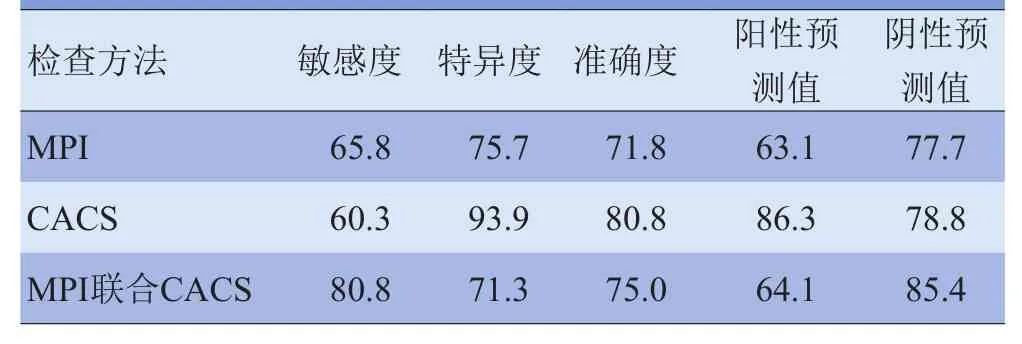
表2 MPI、CACS与MPI联合CACS对CAD的诊断效能比较(%)
2.4MPI联合CACS与MPI、CACS对CAD的诊断效能比较MPI联合CACS对CAD的诊断效能见表2。CACS可纠正MPI漏诊CAD 11例(图2),MPI联合CACS诊断CAD的敏感度高于MPI,差异有统计学意义(χ2=4.233,P<0.05);其诊断特异度和准确度差异无统计学意义(χ2=0.558、0.490,P>0.05);阳性预测值及阴性预测值稍高于MPI,但差异无统计学意义(χ2=0.017、2.032,P>0.05)。
MPI可纠正CACS漏诊CAD 15例,MPI联合CACS诊断CAD的敏感度高于CACS,差异有统计学意义(χ2=7.417,P<0.05);特异度低于CACS,差异有统计学意义(χ2=20.458,P<0.05);准确度差异无统计学意义(χ2=1.871,P>0.05);阴性预测值略高于CACS,但差异无统计学意义(χ2=1.626,P>0.05);阳性预测值低于CACS,差异有统计学意义(χ2=7.986,P<0.05)。
3 讨论
MPI能直接反映心肌缺血的部位、范围及程度,是诊断CAD的无创功能影像技术之一,但目前对MPI诊断CAD的敏感度和特异度尚存在争议[5]。本研究中MPI诊断CAD的敏感度和特异度分别为65.8%、75.7%,与王荣福等[6]的研究结果相似。Underwood等[7]的Meta分析纳入8964例患者,结果显示MPI诊断CAD的敏感度为86%,特异度为74%,其敏感度明显高于本研究结果,可能与本研究纳入的人群多为CAD中度可能的患者有关。近年欧洲心脏病学会和美国心脏病学会指南[2,8]对于CAD中度可能的患者推荐行无创功能或影像检查,而对于CAD高度可能的患者推荐行ICA,因此本研究可以较真实地反映目前可疑CAD患者进行MPI检查的状况。
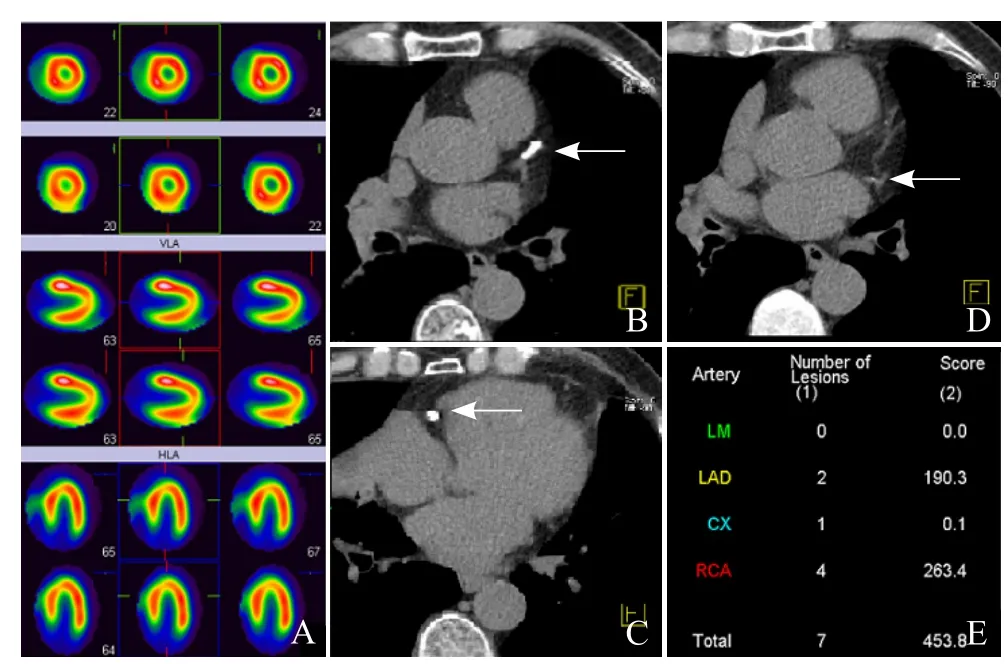
图2 男,65岁,CAD,ICA提示LAD中段狭窄70%,RCA近中段狭窄50%。MPI示放射性摄取未见异常(A);CT示LAD、RCA、LCX均可见钙化(箭,B~D);Agatston分析软件示LAD、RCA、LCX的钙化积分分别为190.3分、263.4分、0.1分,CACS为453.8分(E)。ICA:冠状动脉造影;LAD:左前降支;RCA:右冠状动脉;LCX:左回旋支
本研究发现,MPI诊断CAD具有一定的价值,但仍存在较高的假阳性和假阴性。因此,针对CAD验前概率为中度可能的患者,单纯依靠MPI诊断CAD存在一定的局限性,尤其是当冠状动脉狭窄处于临界病变(ICA显示冠状动脉狭窄50%~70%)时可能并未造成冠状动脉血流动力学改变,此时MPI可能无明显异常改变;而当冠状动脉弥漫性病变时,冠状动脉供血区心肌血流灌注一致性减低,出现“均衡性缺血”也可能造成MPI诊断出现假阴性[9]。
CACS通过检测冠状动脉钙化斑块诊断CAD,CACS>0分代表有冠状动脉粥样硬化,但并不表明一定有阻塞性CAD(冠状动脉狭窄>50%)[10]。Sun等[11]研究证实CAD组CACS高于非CAD组,与本研究结果一致,表明CACS可用于诊断CAD。Tota-Maharai等[12]报道CACS>0分诊断阻塞性CAD的敏感度和特异度分别为96%~100%、30%~58%,目前国内外关于CACS诊断CAD的最佳界值尚无统一标准。美国心脏病学会推荐CACS≥100分为诊断CAD的界值,但以西方人数据为依据的CACS在CAD诊断和预后判断中的标准或界值是否适合所有种族人群一直存在争议[13]。目前国内尚无关于CACS诊断CAD最佳界值的报道。本研究依据ROC曲线获得CACS诊断CAD的最佳界值为96.45分,其诊断CAD的敏感度及特异度分别为60.3%、93.9%,特异度较高,表明当临床可疑CAD患者CACS≥96.45分时应高度警惕CAD的可能。但其敏感度较低可能是因为冠状动脉粥样硬化处于不同的病理阶段,其斑块组成成分不一,当斑块成分主要为脂质或(和)纤维成分时,则检测不出钙化或CACS很低,而此时冠状动脉狭窄程度可能≥50%[14]。
CAD的综合诊断既要了解心肌血流灌注信息,也要了解冠状动脉解剖学信息,单一影像检查容易造成CAD的误诊和漏诊[15]。MPI与CACS对CAD的诊断各有优势,也各有不足。Gaemperli等[16]报道MPI联合异机CT所得的CACS对CAD的诊断效能高于单独MPI或CACS,但由于是两项检查且费时繁琐,使其临床应用受限。目前随着SPECT/CT的广泛应用,MPI联合CACS可同机完成。本研究应用SPECT/CT完成MPI联合CACS一站式检查,结果发现MPI联合CACS诊断CAD的敏感度均高于单用MPI和CACS,与单用MPI相比,MPI联合CACS使CAD假阴性减少了11例,其诊断敏感度由65.8%提高到80.8%,表明通过CACS形态解剖学显像减少了因临界病变、3支病变等导致MPI对CAD的漏诊,明显提高了CAD的诊断敏感度。与单用CACS比较,MPI联合CACS减少了15例假阴性,敏感度由60.3%提高至80.8%,通过血流动力学功能显像减少了非钙化性斑块造成的CAD漏诊,提高了CAD的诊断敏感度。此外,本研究中,MPI和CACS均阳性的29例患者最终均证实为CAD,表明两项检查均阳性的患者CAD可能性大。本研究中,MPI阳性者CACS明显高于MPI阴性者,与文献[17]报道一致,提示心肌缺血与CACS有一定的关系,随着CACS的增加,CACS有可能成为引起MPI异常的重要因素。
总之,MPI诊断CAD有一定的价值,但对冠状动脉临界病变及3支病变存在假阴性;CACS诊断CAD最佳界值为96.45分,CACS≥96.45分时应高度警惕CAD的可能;MPI联合CACS一站式检查可减少单独MPI或CACS对CAD的漏诊,对CAD中度可能患者的诊断筛查具有应用价值。本研究因样本量较少,未分析冠状动脉各分支的钙化积分与相应病变血管血流异常的关系,有待后续进一步研究证实。
参考文献
[1]陈伟伟, 高润霖, 刘力生, 等. 中国心血管病报告2013概要.中国循环杂志, 2014, 29(7): 487-491.
[2]Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force of Cardiology. Eur Heart J, 2013, 34(38): 2949-3003.
[3]张源芳, 彭北杨, 张滨, 等. 多层螺旋CT冠脉钙化积分诊断冠心病及风险预测的临床价值. 中国医学影像学杂志, 2004, 12(5): 334-337.
[4]Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force,American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol, 2014, 63(4): 380-406.
[5]范中杰, 陈黎波, 李方, 等. 腺苷负荷试验心肌核素显像对冠心病诊断价值的评估. 中华内科杂志, 2006, 45(2): 112-115.
[6]王荣福, 邱艳丽, 王立勤, 等.99Tcm-MIBI心肌灌注显像诊断效能与安全性评价的回顾性研究. 中华核医学与分子影像杂志, 2012, 32(6): 413-417.
[7]Underwood SR, Anagnostopoulos C, Cerqueira M, et al. Myocardial perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging, 2004, 31(2): 261-291.
[8]Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/ AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol, 2012, 60(24): e44-e164.
[9]姚稚明, 王蒨, 田月琴, 等. ATP介入心肌灌注显像诊断冠心病的多中心研究. 中华核医学与分子影像杂志, 2014, 34(4): 292-295.
[10]Greenland P, Bonow RO, Brundage BH, et al. ACCF/
AHA 2007 clinical expert consensus document on coronary artery Calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/ AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography). J Am Coll Cardiol, 2007, 49(3): 378-402.
[11]Sun Z, Ng KH. Multislice CT angiography in cardiac imaging. Part II: clinical applications in coronary artery disease. Singapore Med J, 2010, 51(4): 282-289.
[12]Tota-Maharai R, Mcevov JW, Blaha MJ, et al. Utility of coronary artery calcium scoring in the evaluation of patients with chest pain. Crit Pathw Cardiol, 2012, 11(3): 99-106.
[13]von Ziegler F, Brendel M, Uebleis C, et al. SPECT myocardial perfusion imaging as an adjunct to coronary calcium score for the detection of hemodynamically significant coronary artery stenosis. BMC Cardiovasc Disord, 2012, 12: 116.
[14]Lee MS, Chun EJ, Kim KJ, et al. Asymptomatic subjects with zero coronary calcium score: coronary CT angiographic features of plaques in event-prone patients. Int J Cardiovasc Imaging, 2013, 29(1, SI): 29-36.
[15]van JM, Schuijf JD, Gaemperli O, et al. Incremental prognostic value of multislice computed tomography coronary angiography over coronary artery calcium scoring in patients with suspected coronary artery disease. Eur Heart J, 2009, 30(21): 2622-2629.
[16]Gaemperli O, Schepis T, Valenta I, et al. Cardiac image fusion from stand-alone SPECT and CT: clinical experience. J Nucl Med, 2007, 48(5): 696-703.
[17]Schepis T, Gaemperli O, Koepfli P, et al. Added value of coronary artery calcium score as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediaterisk population. J Nucl Med, 2007, 48(9): 1424-1430.
(本文编辑张春辉)
Chinese Journal of Medical Imaging 2016 Volume 24(1): 12-15, 25
【Abstract】Purpose The one-step examination of myocardial perfusion imaging (MPI) combined with coronary artery calcium score (CACS) can obtain both coronary functional information and anatomical information simultaneously, this paper aims to evaluate the value of the one-step examination of MPI combined with CACS for detecting coronary artery disease (CAD).Materials and Methods 188 cases who underwent onestep examination of MPI combined with CACS and invasive coronary angiography (ICA) because of chest tightness, chest pain with suspected coronary artery disease were analyzed retrospectively, with the results of ICA used as "gold standard", the diagnostic efficacy of MPI, CACS and one-step examination with combination of the two techniques for CAD was investigated.Results ① Pre-test probability of CAD was intermediate in 79.8% (150/188), and high in 20.2% (38/188) cases. Seventy-three cases were confirmed as CAD and 115 of 188 patients were negative according to ICA.②The sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) for the diagnosis of CAD by MPI were 65.8%, 75.7%, 71.8%, 63.1% and 77.7%, respectively.③The CACS of CAD group was significantly higher than the non-CAD group (494.96±99.60 vs. 38.15±16.03, P<0.05). According to the features of the ROC curve, the best threshold for the diagnosis of CAD with CACS was 96.45, with CACS ≥96.45 as the positive standard in diagnosis of CAD, the sensitivity, specificity, accuracy, PPV and NPV for the diagnosis of CAD by CACS were 60.3%, 93.9%, 80.8%, 86.3% and 78.8%, respectively.④The sensitivity of MPI combined with CACS were significantly higher than MPI (80.8% vs. 65.8%, P<0.05), while the specificity (71.3% vs.75.7%, P>0.05) and accuracy (75.0% vs. 71.8%, P>0.05) showed no statistically significant difference; the sensitivity of MPI combined with CACS were significantly higher than CACS (80.8% vs. 60.3%, P<0.05), while the specificity was lower than CACS (71.3% vs. 93.9%, P<0.05) and the accuracy showed no statistically significant difference (75.0% vs. 80.8%, P>0.05).Conclusion The one-step examination of MPI combined with CACS can reduce coronary heart disease misdiagnosis, improve the diagnostic sensitivity of CAD compared with the MPI or CACS, with high application value for the diagnosis of CAD, especially in moderate risk groups.
【Key words】Coronary disease; Tomography, emission-computed, single-photon; Tomography, X-ray computed; Technetium Tc 99m sestamibi; Myocardial reperfusion; Calcinosis; Coronary angiography
收稿日期:2015-09-06
中图分类号
基金项目
通讯作者王跃涛
Doi:10.3969/j.issn.1005-5185.2016.01.004