查尔森合并症指数对脓毒症患者预后的评估价值
边士淇,寿松涛,李 望,赵静静
查尔森合并症指数对脓毒症患者预后的评估价值
边士淇,寿松涛,李 望,赵静静

脓毒症;查尔森合并症指数;急性生理与慢性健康状况评分系统Ⅱ;预后;死亡
边士淇,寿松涛,李望,等.查尔森合并症指数对脓毒症患者预后的评估价值[J].中国全科医学,2015,18(14):1637-1640.[www.chinagp.net]
Bian SQ,Shou ST,Li W,et al.Appraisal value of charlson comorbidities index in the prognosis of septic patients[J].Chinese General Practice,2015,18(14):1637-1640.
脓毒症症状复杂,主要受遗传、感染类型、治疗时机、治疗方法以及其他不确定因素的影响[1]。感染高发于酗酒者、营养不良者、慢性肝肾或心血管疾病者,以及癌症或糖尿病患者[2-3]。据统计,癌症患者中约有9%死于脓毒症,而1/6的脓毒症患者患有癌症[4]。因此,有学者指出,脓毒症合并症增加了死亡风险。
Charlson等[5]提出的查尔森合并症指数(CCI)已被证明对重症监护病房(ICUs)住院患者的1年生存率具有很高的预测价值。对于住院危重患者病死率也有很好的预测价值[6-9]。与其他评分量表,如急性生理与慢性健康状况评分系统(Acute Physiology and Chronic Health Evaluation,APACHE)及脓毒症相关性器官功能衰竭评分(Sepsis-related Organ Failure Assessment,SOFA)相比,CCI基本上可以单独依靠病历资料进行评估,且计算快速、简便、价廉。然而CCI相较于其他疾病评分对危重患者结局预测的有效性和实用性目前仅得到了有限的数据支持[6-7,10],在脓毒症患者中的研究也较少[11-12]。本研究分析了CCI对脓毒症患者死亡风险的评估价值,并与APACHEⅡ评分进行比较。
1 资料与方法
1.1 一般资料 回顾性分析2012年12月—2014年7月入住天津医科大学总医院急诊医学科病房,出院诊断为脓毒症患者的病历资料。纳入标准:(1)患者出院诊断为脓毒症;(2)年龄≥18岁;(3)患者病历资料齐全。排除标准:(1)手术后的患者;(2)入院时间不满24 h者。
1.2 诊断标准 脓毒症及严重脓毒症的诊断标准按照美国胸科医师协会/危重病医学会(ACCP/SCCM)联席会议制定的标准[13]。患者的管理及治疗均按照相关的指南标准执行[13-14]。
1.3 观察指标及分组 收集患者的一般资料,包括性别、年龄、既往基础疾病、28 d预后、出院时转归、住院时间等。按照患者28 d预后情况分为死亡组和存活组。根据APACHEⅡ量表收集患者入院24 h内各项指标的最差值,计算APACHEⅡ评分[15]。根据患者基础疾病情况计算CCI评分[5],评分量表见表1。
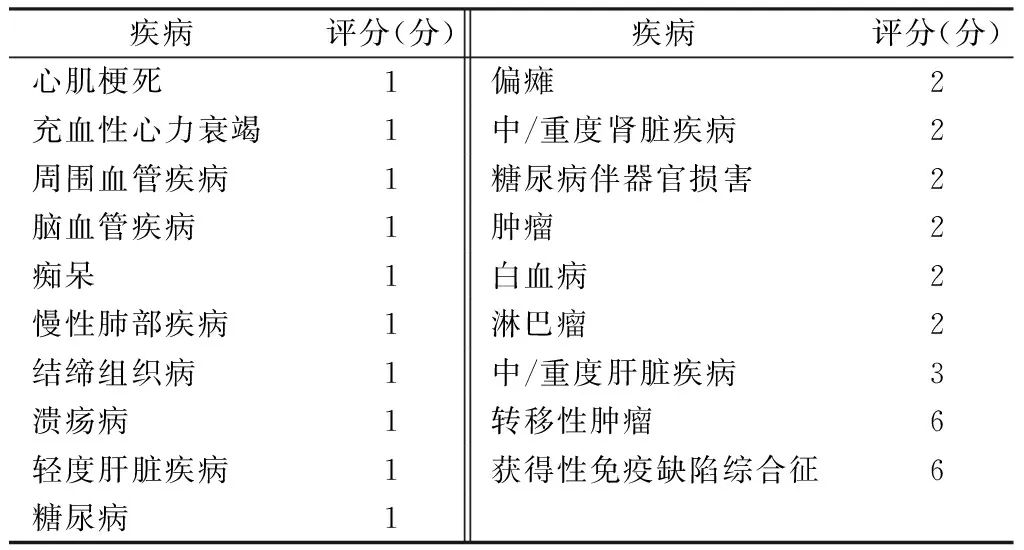
表1 CCI评分量表
2 结果
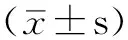
2.1 基本资料及临床指标对预后的影响 共204例患者纳入研究:其中男125例(61.3%),女79例(38.7%);脓毒症121例(59.3%),严重脓毒症66例(32.4%),脓毒症休克17例(8.3%);存活组132例(64.7%),死亡组72例(35.3%)。年龄(66.5±17.4)岁,APACHEⅡ评分(13.2±7.2)分,CCI评分(2.9±2.3)分。
单因素分析结果显示,年龄、APACHEⅡ评分、CCI评分、感染情况、充血性的心力衰竭、中/重度肾脏疾病及中/重度肝脏疾病对脓毒症患者28 d预后有影响(P<0.05,见表2)。
表2 脓毒症患者28 d预后的单因素分析
注:APACHEⅡ=急性生理与慢性健康状况评分系统Ⅱ,CCI=查尔森合并症指数;*为t值
2.3 Logistic回归分析 选取单因素分析中有统计学意义的变量为自变量,以预后(死亡/存活)为因变量进行多因素Logistic回归分析,结果显示:APACHEⅡ评分和CCI评分是预测脓毒症患者28 d预后的独立因素(P<0.01,见表4)。
2.4 CCI评分和APACHEⅡ评分评估脓毒症患者预后的ROC曲线 绘制两种评分评估脓毒症患者28 d预后的ROC曲线,CCI评分ROC曲线下面积为0.708〔95%CI(0.635,0.782),P<0.01〕,APACHEⅡ评分ROC曲线下面积为0.816〔95%CI(0.758,0.874),P<0.01,见图1〕,两评分ROC曲线下面积间差异有统计学意义(Z=2.269,P<0.05)。
表3 不同CCI评分脓毒症患者28 d病死率〔n(%)〕
Table 3 Comparison of 28 days mortality rate of septic patients with different CCI scores

CCI评分(分)例数病死率CCI评分(分)例数病死率0253(12.0)684(4/8)1376(16.2)785(5/8)23310(30.3)840 34419(43.2)941(1/4)42610(38.5)1010 5136(46.2)1110
表4 影响脓毒症患者28 d预后的多因素Logistic回归分析
Table 4 Multivariable Logistic regression analysis on influencing factors for 28 days prognosis of septic patients

临床指标bSEWaldχ2值dfP值OR(95%CI)年龄0.0050.0140.14010.7091.005(0.979,1.032)APACHEⅡ评分0.1700.03227.5761<0.0011.185(1.112,1.263)CCI评分0.2480.0937.06410.0081.281(1.067,1.538)严重脓毒症-0.9630.8512.07110.1870.387(0.113,1.447)脓毒症休克-1.0530.7212.13010.1440.349(0.085,1.132)充血性心力衰竭-0.3220.4990.41710.5190.725(0.272,1.927)中/重度肾脏疾病-0.4140.5820.50610.4770.661(0.211,2.069)中/重度肝脏疾病-0.8660.7221.43610.2310.421(0.102,1.734)常数-2.7131.2804.49610.0340.066

图1 CCI评分和APACHEⅡ评分预测脓毒症患者28 d预后的ROC曲线
Figure 1 ROC curves of CCI and APACHEⅡ score for predicting 28 d prognosis of septic patients
3 讨论
3.1 CCI评分 多项研究分析了脓毒症患者的致死因素,并指出除了急性器官损害的定量数据,基础疾病情况也与其病死率相关[2,17-20]。因此,恶性肿瘤、肝硬化、充血性心力衰竭及HIV感染等,被认为与不良结局有关[21],而感染本身的特点对预后的影响似乎不是很大[19,22-23]。Charlson等[5]提出了CCI评分系统,提供了一个可靠的分层方法,其包括19种基础疾病,按疾病权重计分,累加之和即为患者的基础疾病评分。
一些研究认为,CCI评分对于腹膜透析[24]、不同类型恶性肿瘤[25-26]、感染性心内膜炎[27]及金黄色葡萄球菌血症患者[12]能够准确预测病死率。在与脓毒症相关的研究中,有学者指出,合并症是影响脓毒症患者病死率及医疗资源利用的重要因素之一,通过CCI评分可以较好地预测脓毒症患者的预后[11]。本研究结果显示,死亡组与存活组CCI评分间有显著差异,提示患者死亡风险与CCI评分相关。趋势χ2检验显示,随CCI评分升高(0~7分),病死率相应增加;CCI评分在8~10分时,与病死率相关性不明显。其原因可能为8~10分段患者例数较少,造成误差较大。Logistic回归分析显示:CCI评分和APACHEⅡ评分均是预测脓毒症患者28 d预后的独立因素。
3.2 CCI评分和APACHEⅡ评分比较 APACHEⅡ是Knaus等[15]在APACHEⅠ基础上进行修订,于1985年提出的评分系统,包括年龄评分、急性生理学评分及慢性健康状况评分3部分,是目前应用最为广泛的评分量表之一。本研究通过与APACHEⅡ评分进行对比,发现CCI评分的预测效能逊于APACHEⅡ评分,这与既往研究结果一致[7,26,28]。但APACHEⅡ评分需要根据量表收集患者入院后24 h内各项指标的最差值进行计算[15],高度依赖于临床情况和实验室检查结果,项目较多且计算较为繁琐。而CCI评分仅依据病史资料,计算简便。相较而言,CCI评分更为便捷。在患者临床情况难以判断、实验室数据尚不完善时,CCI评分可以发挥更显著的优势,为患者危险度分层、治疗策略的制定争取宝贵的时间。
3.3 不足与展望 本研究还存在一些不足之处:(1)作为回顾性研究,纳入病例数相对较少;(2)没有对患者入院28 d后的转归进行记录与分析;(3)在收集患者临床资料过程中可能存在潜在的偏倚。
鉴于其简便、快捷、高性价比等特点,CCI评分有较大的应用价值,尤其对于急诊及新入院患者的病情评估。希望今后有多中心大样本量的前瞻性队列研究,进一步验证本研究结论,并使CCI评分得到推广。
[1]Cohen J.The immunopathogenesis of sepsis[J].Nature,2002,420(6917):885-891.
[2]Dhainaut JF,Claessens YE,Janes J,et al.Underlying disorders and their impact on the host response to infection[J].Clinical infectious diseases,2005,41(Supple 7):S481-489.
[3]Esper AM,Moss M,Lewis CA,et al.The role of infection and comorbidity:factors that influence disparities in sepsis[J].Critical Care Medicine,2006,34(10):2576-2582.
[4]Angus DC,Linde-Zwirble WT,Lidicker J,et al.Epidemiology of severe sepsis in the United States:analysis of incidence,outcome,and associated costs of care[J].Critical Care Medicine,2001,29(7):1303-1310.
[5]Charlson ME,Pompei P,Ales KL,et al.A new method of classifying prognostic comorbidity in longitudinal studies:development and validation[J].Journal of Chronic Diseases,1987,40(5):373-383.
[6]Norena M,Wong H,Thompson WD,et al.Adjustment of intensive care unit outcomes for severity of illness and comorbidity scores[J].Journal of Critical Care,2006,21(2):142-150.
[7]Quach S,Hennessy DA,Faris P,et al.A comparison between the APACHE II and Charlson Index Score for predicting hospital mortality in critically ill patients[J].BMC Health Services Research,2009,9(1):129.
[8]Poses RM,Mcclish DK,Smith WR,et al.Prediction of survival of critically ill patients by admission comorbidity[J].Journal of Clinical Epidemiology,1996,49(7):743-747.
[9]D′Hoore W,Sicotte C,Tilquin C.Risk adjustment in outcome assessment:the Charlson comorbidity index[J].Methods of Information in Medicine,1993,32(5):382-387.
[10]Sogaard M,Schonheyder HC,Riis A,et al.Short-term mortality in relation to age and comorbidity in older adults with community-acquired bacteremia:a population-based cohort study[J].Journal of the American Geriatrics Society,2008,56(9):1593-1600.
[11]Yang Y,Yang KS,Hsann YM,et al.The effect of comorbidity and age on hospital mortality and length of stay in patients with sepsis[J].Journal of Critical Care,2010,25(3):398-405.
[12]Lesens O,Hansmann Y,Storck D,et al.Risk factors for metastatic infection in patients with Staphylococcus aureus bacteremia with and without endocarditis[J].European Journal of Internal Medicine,2003,14(4):227-231.
[13]Bone RC,Balk RA,Cerra FB,et al.Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis.The ACCP/SCCM Consensus Conference Committee.American College of Chest Physicians/Society of Critical Care Medicine[J].Chest Journal,1992,101(6):1644-1655.
[14]Dellinger RP,Levy MM,Carlet JM,et al.Surviving Sepsis Campaign:international guidelines for management of severe sepsis and septic shock:2008[J].Intensive Care Medicine,2008,34(1):17-60.
[15]Knaus WA,Draper EA,Wagner DP,et al.APACHE II:A severity of disease classification system[J].Critical Care Medicine,1985,13(10):818-829.
[16]Hanley JA.The meaning and use of the area under a receiver operating characteristic(ROC) curve[J].Radiology,1982(74):329-336.
[17]Freid MA,Vosti KL.The importance of underlying disease in patients with gram-negative bacteremia[J].Archives of Internal Medicine,1968,121(5):418-423.
[18]Pittet D,Thievent B,Wenzel R,et al.Importance of pre-existing co-morbidities for prognosis of septicemia in critically ill patients[J].Intensive Care Medicine,1993,19(5):265-272.
[19]Brun-Buisson C,Doyon F,Carlet J.Bacteremia and severe sepsis in adults:a multicenter prospective survey in ICUs and wards of 24 hospitals.French Bacteremia-Sepsis Study Group[J].American Journal of Respiratory and Critical Care Medicine,1996,154(3):617-624.
[20]Croce MA,Fabian TC,Waddle-Smith L,et al.Identification of early predictors for post-traumatic pneumonia[J].The American Aurgeon,2001,67(2):105-110.
[21]Alberti C,Brun-Buisson C,Chevret S,et al.Systemic inflammatory response and progression to severe sepsis in critically ill infected patients[J].American Journal of Respiratory and Critical Care Medicine,2005,171(5):461-468.
[22]Brun-Buisson C,Doyon F,Carlet J,et al.Incidence,risk factors,and outcome of severe sepsis and septic shock in adults:a multicenter prospective study in intensive care units[J].JAMA,1995,274(12):968-974.
[23]Rangel-Frausto MS,Pittet D,Costigan M,et al.The natural history of the systemic inflammatory response syndrome(SIRS):a prospective study[J].JAMA,1995,273(2):117-123.
[24]Fried L,Bernardini J,Piraino B.Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients[J].American Journal of Kidney Diseases,2001,37(2):337-342.
[25]Albertsen PC,Moore DF,Shih W,et al.Impact of comorbidity on survival among men with localized prostate cancer[J].Journal of Clinical Oncology,2011,29(10):1335-1341.
[26]Kobayashi Y,Miura K,Hojo A,et al.Charlson Comorbidity Index is an independent prognostic factor among elderly patients with diffuse large B-cell lymphoma[J].Journal of Cancer Research and Clinical Oncology,2011,137(7):1079-1084.
[27]Fedeli U,Schievano E,Buonfrate D,et al.Increasing incidence and mortality of infective endocarditis:a population-based study through a record-linkage system[J].BMC Infectious Diseases,2011,11(1):48.
[28]Needham DM,Scales DC,Laupacis A,et al.A systematic review of the Charlson comorbidity index using Canadian administrative databases:a perspective on risk adjustment in critical care research[J].Journal of Critical Care,2005,20(1):12-19.
(本文编辑:赵跃翠)
Appraisal Value of Charlson Comorbidities Index in the Prognosis of Septic Patients
BIANShi-qi,SHOUSong-tao,LIWang,etal.
GeneralHospitalofTianjinMedicalUniversity,Tianjin300052,China

Sepsis;CCI;APACHEⅡ;Prognosis;Death
300052天津市,天津医科大学总医院
R 631
A
10.3969/j.issn.1007-9572.2015.14.009
2014-11-20;
2015-03-10)