Effectofburden and origin sites ofpremature ventricular contractions on left ventricular function by 7-day Holter monitor
Wenhua Xu,Mingfang Li,Minglong Chen,Bing Yang,Daowu Wang,Xiangqing Kong,
Hongwu Chen1,Weizhu Ju1,Kai Gu1,Kejiang Cao1,Hailei Liu1,Qi Jiang1,Jiaojiao Shi1,Yan Cui2,✉, Hong Wang3,✉
1Department of Cardiology,the First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Nursing College of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
3Department of Respiratory,the First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China.
Effectofburden and origin sites ofpremature ventricular contractions on left ventricular function by 7-day Holter monitor
Wenhua Xu1,Δ,Mingfang Li1,Δ,Minglong Chen1,Bing Yang1,Daowu Wang1,Xiangqing Kong1,
Hongwu Chen1,Weizhu Ju1,Kai Gu1,Kejiang Cao1,Hailei Liu1,Qi Jiang1,Jiaojiao Shi1,Yan Cui2,✉, Hong Wang3,✉
1Department of Cardiology,the First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Nursing College of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
3Department of Respiratory,the First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China.
Recent studies have shown thatpremature ventricular contractions(PVCs)could enlarge the heart,butits risk factors are incompletely understood as a single 24-hour recording cannot reflect the true PVC burden due to day-to-day variability.Our purpose was to investigate the effect of burden and origin sites on leftventricular (LV)function in patients with PVCs by 7-day Holter electrocardiography(ECG).From May 2012 to August 2013,112 consecutive patients with PVCs were recruited from the authors’affiliated hospital.Allpatients received 2-dimensionaltransthoracic echocardiography,12-lead routing ECG and 7-days Holter ECG.Serum N-terminalprobrain natriuretic peptide(NT-proBNP)levels were measured.A totalof102 participants with PVCs were included in the finalanalysis.Origin of PVCs from the tricuspid annulus had the highestburden and NT-proBNP level.LV papillary muscle had a higher LV ejection fraction(EF)leveland a lower LV end-systolic dimension(ESD)than other PVC foci(P<0.05).The high burden group had a higher LV end-diastolic dimension(EDD)and LVESD but lower LVEF than the other two groups(P<0.05).Female,older age,physical work,and history of PVCs had a significantly positive correlation with symptoms.Male,older age,physical work,and high burden were positive predictors ofenlarged LVEDD,LVESD and higherserum NT-proBNP level,butlower LVEF.Seven-day dynamic ECG Holtermonitorshowed the true PVC burden on patientswith PVCs.PVCs with a lowerburden ororigin from the LV papillary muscle and the fascicle were relatively benign,while PVCs with a higherburden ororigin from the tricuspid annulus may lead to cardiac dysfunction.
premature ventricular contractions,burden,origin sites,left ventricular function
Introduction
Premature ventricular contractions(PVCs)are commonly encountered in daily clinical practice.Incidence of PVCs is related to the detection methods and study population.PVCs are common with an estimated prevalence of 1%-4%in the general population[1],and have been detected in 1%of subjects by standard 12-lead electrocardiography(ECG)and in 40%-75%of subjects by Holter ECG monitoring for 24-48 hours[2].
In normalsubjects,PVCs are usually associated with no clinical symptoms,but in some people they may cause incapacitating symptoms such as pectoralgia, palpitations,syncope and heart failure[3].Traditionally, subjects with PVCs have a benign prognosis in nonstructural heart disease[1,4].However,recent studies have found that PVCs lead to heart enlargement and even reversible cardiomyopathy[5-15].
It is still unknown why most patients with frequent PVCs have a benign course,while up to 1/3 of them develop cardiomyopathy.One possible explanation is that evaluation of PVC burden using 24-hour Holter monitoring may be inadequate and may misrepresent the true PVC burden of patients[16-17].PVCs arise from various locations in the ventricle,but the effects of origin site of PVCs on cardiac structure and function are stillcontroversial[18-20].This study evaluated if burden and origin sites of PVCs are associated with leftventricular(LV)function by 7 consecutive days ECG monitoring,and analyzed influencing factors of burden and the symptoms of PVC patients,so as to provide a more comprehensive basis for the treatment of PVC patients and improve their quality of life.
Patients and methods
Patients
From May 2012 to August 2013,112 consecutive patients with PVCs were recruited from the authors’affiliated hospital.All participants had at least one documented episode of PVCs by 12-lead surface ECG or 24-48 hour Holter ECG recording,and had not taken any anti-arrhythmic drugs for at least 5 half-lives.All patients provided informed consentand the study was approved by the localinstitutionalboard atthe authors’affiliated institution.
Exclusion criteria for patients were listed as follows: (a)structuralheartdisease;(b)liverorkidney dysfunction combined with other serious diseases,and life expectancy was less than 1 year;(c)PVCs caused by reversible causes(infection,electrolyte imbalance, and drugs,etc.);(d)unwillingness to sign informed consent.
Data acquisition
After medicalhistory inquiry and recording,physicalexamination was performed to exclude related disease.Serum N-terminal pro-brain natriuretic peptide (NT-proBNP)levels were determined,and 2-dimensionaltransthoracic echocardiography,12-lead routine ECG and 7-day-Holter ECG were performed in all patients.Some patients with a higher burden of PVCsunderwentcardiac electrophysiologicalexamination orcoronary angiography.Serum NT-proBNP level was analyzed as instructed by the manufacturer by electrochemiluminescence analyzer Roche Elecsys 2010 using a Roche NT-proBNP electrochemiluminescentimmunoassay kit(Roche Diagnostics,Rotkreuz, Switzerland).Measurement range of NT-proBNP was 5-35000 pg/mL.Normal values in male were 0-85 pg/mL(≤44 years),0-121 pg/mL(45-54 years),0-210 pg/mL(55-64 years),0-376 pg/mL(65-74 years) and 0-486 pg/mL(≥75 years).Normal values in female were 0-130 pg/mL(≤44 years),0-249 pg/mL (45-54 years),0-287 pg/mL(55-64 years),0-301 pg/ mL(65-74 years)and 0-738 pg/mL(≥75 years).
Cardio Trak CT Series Holter recorder from Hangzhou Medical Equipment Co.,Ltd.was used to record holographic 3-channel ECG for 7 days.Holter results were separatly analyzed by 2 cardiologists who were blinded to the ECG results.
Two-dimensional echocardiography
Two-dimensional(2D)ECG was obtained in each case using an ultrasound machine(Vivid7,GE Medical Systems,Milwaukee,WI,USA)with an M4S probe.Patients were examined in the leftlateral decubitus position,and images were acquired at end expiration to minimize global cardiac movement.LV end-diastolic and end-systolic diameters(EDD and ESD)were measured by 2D method from the parasternallong-axis view.They were recorded from 3 consecutive cycles in M mode using methods adopted by the American Society of Echocardiography.LV end-diastolic volume(EDV)and LV end-systolic volumes (ESV)were measured using Simpson biplane method, and LV ejection fraction(EF)was calculated as(EDVESV)/EDV.
Site of origin of PVCs
PVC burden refers to the ratio of the number of PVCs divided by the totalheart rate.Origin of PVCs was diagnosed by 12-lead ECG or electrophysiological examination.The site of origin of PVCs was analyzed by 2 clinicalelectrophysiologists who were blinded to the results.Mapped site of PVC ablation during the electrophysiologic study of 32 patients thatunderwent radiofrequency ablation was verified with ECG estimation.The criteria thatused to define the site oforigin of PVCs based on their ECG features were listed as follows[21-23]:(1)Right ventricular outflow tract(RVOT): left bundle branch block(LBBB)morphology with an inferior axis,tall R waves in the inferior leads inII,III,aVF and negative(QS)complexes in aVR and aVL,and an all-negative QRS or a small"r"wave in lead V1.(2)LV outflow tract(LVOT):right bundle branch block(RBBB)morphology,tall R waves in the inferior leads in II,III,aVF and negative(QS)complexes in I and aVL.(3)Mitralannulus:RBBB morphology similar to type A pre-excitation syndrome wave,tallR waves in lead V1,early precordialtransition to lead V2,and lead V6 form is RS ortype Rs.(4)The tricuspid annulus:LBBB morphology similar to type B pre-excitation syndrome wave.(5)The LV papillary muscle:RBBB morphology with a smallq wave preceding R wave in lead V1,leftanterioror posterior fascicular block which is not typical.(6)Fascicular:typical RBBB(rsR’)morphology with the superior(the leftposteriorfascicle)orinferior(the leftanteriorfascicle)axis. (7)The other sites:PVCs originated from LV free wall has a RBBB morphology with negative in aVL and lead I.PVCs originated from RV free wallhas a LBBB morphology with a non-inferior axis.PVCs originated from Greatcardiac vein has a LBBB morphology similar to RVOT origin butwith a more prominent"r"wave amplitude and duration in lead V1,in addition to a predominantly positive QRS complex in lead I,and more prominent"R"wave in lead V6[21-23].
Questionnaire
In ourstudy,self-madegeneraldataquestionnairewas applied to therecruited PVCpatients(The questionnaire is available online as Supplementary Table 1).According to previous studies[3,5,7-9,16-19,24],a structured general data questionnaire was designed specifically for PVC patients based on face-to-face interview to PVC patients by taking the advice by experts and panel discussions. The questionnaire included age,gender,education level, maritalstatus,occupation,symptoms,and history of PVCs,smoking state,alcoholintake,caffeinated beverages,and symptoms.
Each participantwasinterviewed by the investigatorin a standardized mannerbefore they took 7-consecutiveday echocardiography monitoring.Ifthe participantwas illiterate,the investigatorwould explain the questions to the patientand his/her relative,and helped the participant to complete the questionnaire.Ifthe participantwanted to fillitby themselves,they could finish itaccording to directions on the questionnaire.Ifthe data was notfilled out completely,we willcontactthe patients again foradditionalinformation.
Statistical analysis
Data were double-entered into Epidata 3.1 and analyzed by SPSS18.0.Continuous variables were expressed as mean±SD.Frequencies,percentages, means,and standard deviations were used to describe demographic and characteristics of the general data of PVC patients.Continuous variables were compared using one-way ANOVA(normal distributions) or Wilcoxon's rank sum test(for non-normal distributions).Equal varian ces assumed were assessed with the LSD test.Equal variances not assumed were assessed with Tamhane's T2 test.Categorical variables were compared using Fisher's exact test or x2-test.Correlations between variables were tested using the Spearman or Pearson test.Linear regression analysis wa s performed using backward elimination to determine significant variables for predicting LV function.All statistical tests were twotailed,and P<0.05 was considered statistically significant.
Results
Characteristics and burden of the participants
In total,questionnaireswere distributed to 112 patients, and 102 were effective samples(response rate was 91.07%).Seven cases were excluded because they removed the Holter recorders before the completion of monitoring periods.The remaining two questionnaires were excluded because the patients could notendure onsetof severe symptoms and then took anti-arrhythmic drugs.One questionnaire was excluded because the patientwas only 5 years old.The mean age of102 effective participants was 44.11±15.16(range 18-72)years, the mean duration of PVCs was 4.76±6.28(0.1-30) years,and the mean heart rate was 75.38±8.53(56-104)beats/minute.Thwenty-seven patients had primary hypertension,9 patients had diabetes mellitus,and 17 patients had hypercholesterolemia.
Characteristics and burden of the participants are shown in Table 1.The mean burden of 102 patients was 14.47%±11.88%(0.02-49.21)%.The patients were divided into the low burden group(<10%; n=42),the medium burden group(10%-20%; n=31),and the high burden group(>20%;n=29). No significant differences were found in age,gender, education level,marital status,occupation,history of PVCs,smoking,alcohol intake,caffeinated beverages,history of hypertension,diabetes mellitus,or hypercholesterolemia among the 3 burden groups. Table 2 demonstrates the number and percentage of symptoms in 102 patients with PVCs.Eight (7.84%)patients had no symptoms,16(15.69%) patients had 1 symptom,16(15.69%)patients had 2 symptoms,25(24.51%)patients had 3 symptoms, 20(19.61%)patients had 4 symptoms,5(4.85%)patients had 5 symptoms,7(6.86%)patients had 6 symptoms,and 5(4.90%)patients had 7 symptoms. Palpitations,fatigue and shortness of breath were the most common symptoms in patients with PVCs.
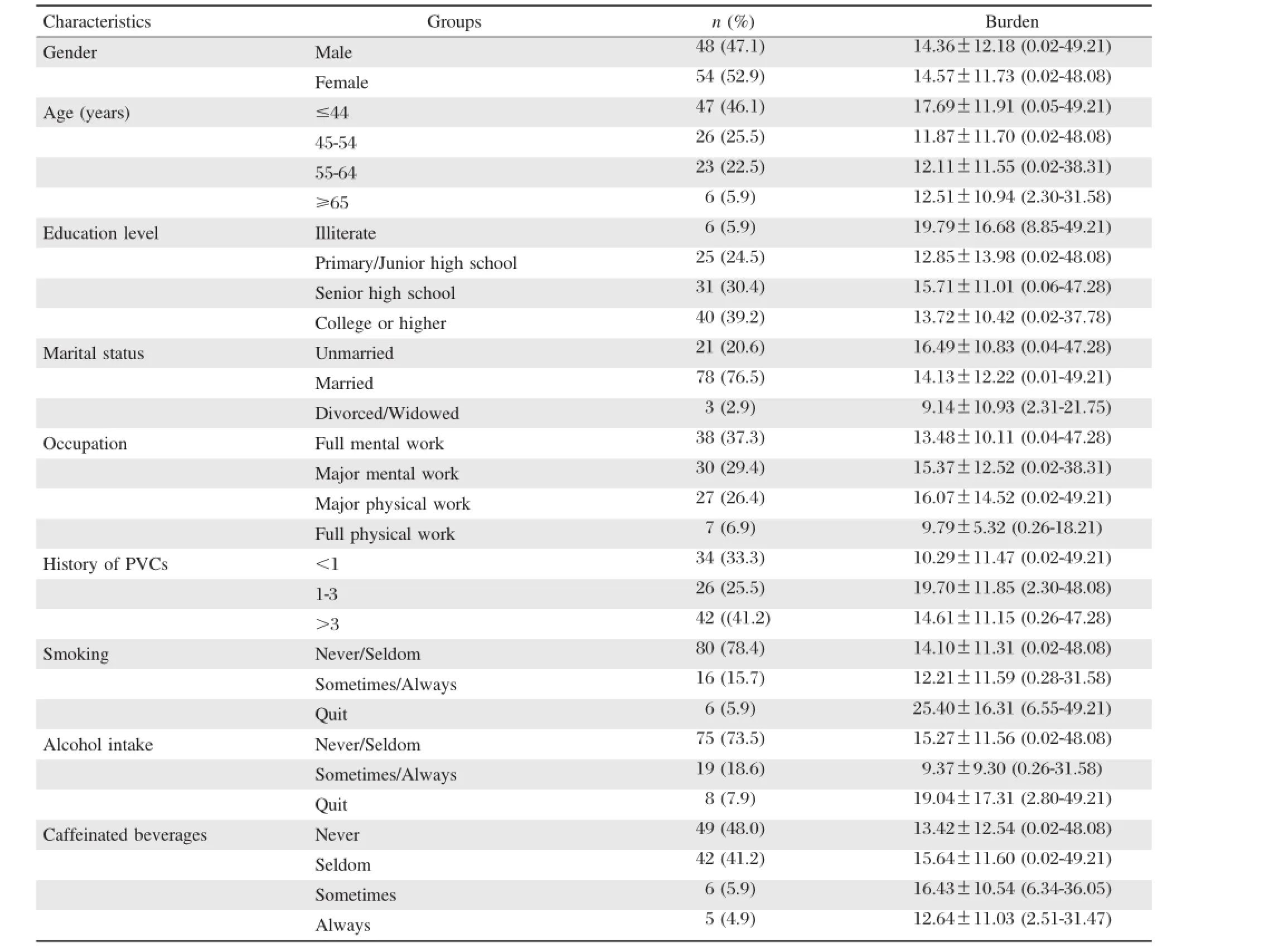
Table 1 Characteristics and burden of 102 PVC patients
Distribution of origin sites of PVCs
The origin of PVCs in 47 patients(46.1%)was from the RVOT,in 23 patients(22.6%)from the LVOT,in 5 patients(4.9%)from the mitralannulus,in 8 patients(7.8%)from the tricuspid annulus,in 5 patients(4.9%) from the LV papillary muscle,in 9 patients(8.8%)from the fascicle,and in the remaining 5 patients(4.9%)from the other parts(the pulmonary artery,the LV free wall and the epicardium).No significant differences were found in age,gender,and othervariables among the 7 origin sites.The burden in different origin sites of 102 patients with PVCs is shown in Fig.1.PVCs originated from the tricuspid annulus had the highestburden than those from other sites.PVCs originated from the LV papillary muscle and the fascicle had the lowestburden than those from other sites.
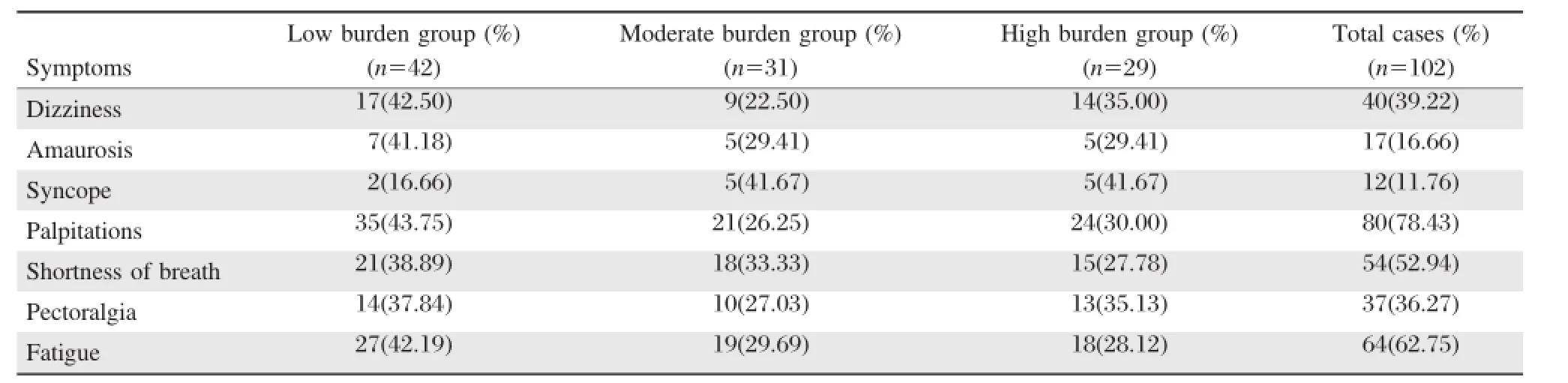
Table 2 Symptoms of 102 PVC patients
LV function
The median serum NT-proBNP contentwas 110.50 ng/L(25%-75%CI 45.00~108.00 ng/L).Ninety-one (89.2%)PVC patientshad normalNT-proBNP content, and 11(10.8%)patients had higher NT-proBNP levels. NT-proBNP levels in different groups are shown in Table 3.Patients with PVCs originated from RVOT showed lower NT-pro BNP levels than those from LVOT.Patients with PVCs originated from the mitral annulus,the LV papillary muscle and the fascicle had normal NT-proBNP level.We also found that patients with PVCs originated from the tricuspid annulus had the highest NT-proBNP level compared other different origin.The mean burdens of patients with normal NT-proBNP content and those with higher NT-proBNP levels were 12.90±10.50(0.02-48.08)% and 27.44±15.04(2.73-49.21)%,respectively.
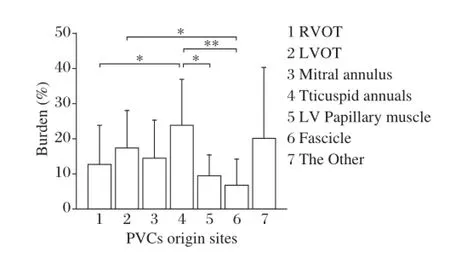
Fig.1 The burden in different origin sites of 102 PVCs patients.The y axis indicates the burden of premature ventricular contractions(PVCs).There was a statistically significant difference of burden among the tricuspid annulus with the right ventricular out tract (RVOT),the left ventricular(LV)papillary muscle,and the fascicle groups.There was a significantdifference ofburden between the fascicle and left ventricular out tract(LVOT group).*indicate P<0.05, **indicate P<0.01.Error bars,mean±SD.
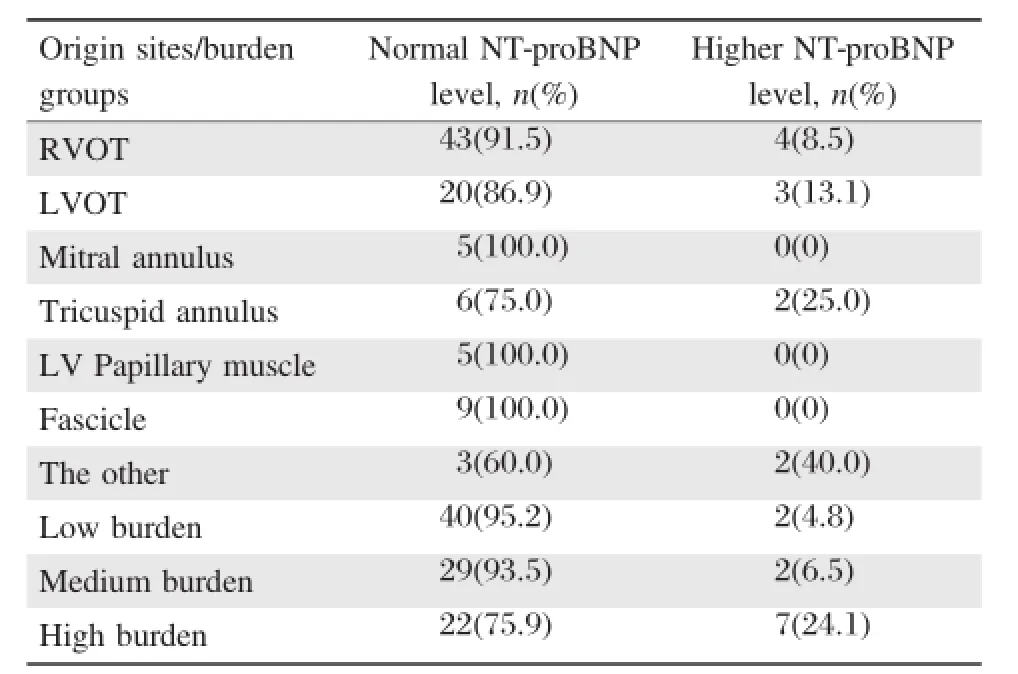
Table 3 Different origin sites/burden groups effect on NT-proBNP level of 102 PVCs patients
The mean value of LVEDD was 49.81±4.25(42-60)mm;the mean value of LVESD was 32.69±3.72 (26-44)mm in male,the mean value of LVEDD was 47.80±4.06(41-59)mm;the mean value of LVESD was 31.43±3.09(25-39)mm in female,and the mean value of LVEF was 33-73(63.14±5.21)mm.Table4 shows the effectof differentorigin sites on LVEDD, LVESD and LVEF of the 102 patients with PVCs. PVCs originated from the LV papillary muscle had a higher LVEF level and a lower LVESD than those from other PVC foci(P<0.05).Table 5 shows the effect of different burdens on LVEDD,LVESD and LVEF ofthe 102 patients with PVCs.The high burden group had a larger LVEDD and LVESD and lower LVEF than the other 2 groups(P<0.05).
Determinants of symptoms and LV function of patients with PVCs
Spearman correlations ofcharacteristics,burden,origin sites and LV function parameters with symptoms are shown in Table 6.Age had significantly positive correlation with palpitations(P=0.017)and fatigue (P=0.025).Significant positive correlation was found between physical work and shortness of breath (P=0.018).Female,physical work,and LVEF had significantly positive correlation with dizziness (P=0.018;P=0.012;P=0.025).Significantly positive correlation was found between female gender and amaurosis(P=0.033).Female and physicalwork were significantly positively correlated with syncope (P=0.025;P=0.032).By calculating all types of symptoms of each patient as their own totalsymptoms, we found that symptoms had a significantly positive correlation with female gender(P=0.013),older age (P=0.036),physical work(P=0.019)and history of PVCs(P=0.021).
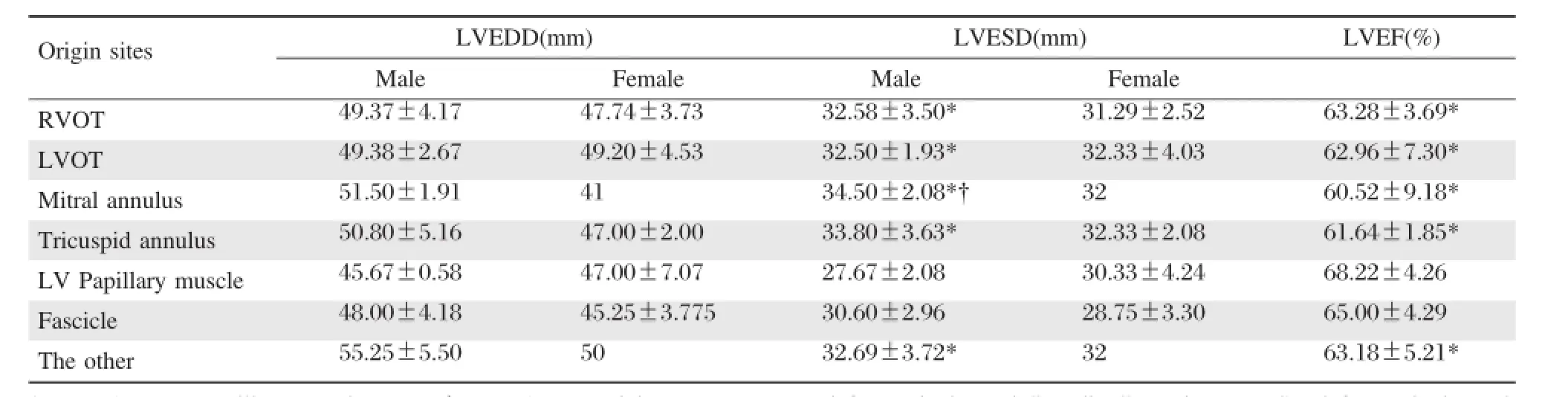
Table 4 Different origin sites and LVEDD,LVESD and LVEF
In backward regression analysis,the dependentvariables were NT-proBNP,LVEDD,LVESD and LVEF, respectively,and the independentvariables were the characteristics of participants,including age,gender, education level,occupation,history of PVCs,smoking status,alcohol intake,caffeinated beverages,burden and origin sites.Table 7 shows that higher burden was a predictor of higher level of NT-proBNP.Male and higher burden were predictors of larger LVEDD. Male,physical work,and higher burden were predictors of larger LVESD.Older age and higher burden were predictors of lower LVEF.
Discussion
Premature ventricular contractions(PVCs)commonly occur in the general population.They typically carry a good prognosis withoutstructuralheartdisease. However,recent studies found that PVCs have been implicated in the developmentof LV dysfunction and cardiomyopathy[8,17,19],but the risk factors and pathogenic mechanisms are incompletely understood. Generally,PVC burden should be assessed by continuous Holter monitoring for atleast24 hours.Thus,a single 24-hour recording may not reflect the true PVC burden and its detection rate was only(40-75)%due to day-to-day variability[2],a strong suspicion that frequent PVCs may lead to LV dysfunction may warrant extended Holterrecordingsof48 to 72 hours orseveral 24-hour Holter recordings[17].This study was the firstto use 7-day dynamic ECG Holter monitoring on patients with PVCs.The burden of all patients in this study were the mean data of 7 consecutive days.
In our study,102 consecutive patients with PVCs with no otheridentified causes ofcardiomyopathy underwent 7-day Holter monitoring.We found thatthe majority of patients had clinical symptoms,.Approximately three quarters of the patients reported palpitations,62.75% patients feltfatigue,and abouthalf of the patients had symptoms of shortness of breath.The high incidence of symptoms in our study may be associated with the source of patients who were alloutpatients seeking medicalcare.Interestingly,we found thatpatientswith PVCs in the high burden group had more severe symptoms of syncope than those in the low burden group.However, patients with PVCs in the low burden group had more mild symptoms of fatigue,palpitations and shortness of breath than those in the high burden group.Itisprobably due to patients with high burden PVCs had poorer cardiac function than those patients with low burden PVCs[21,25].Therefore,patients with high burden PVCs had more severe symptoms than patients with low burden PVCs.Moreover,patients with high burden PVCs had lessmildly symptomatic due to tolerance ofpoorcardiac function.Patients with low burden PVCs are moresensitive to those with mild symptoms such as palpitations and fatigue and shortness of breath.
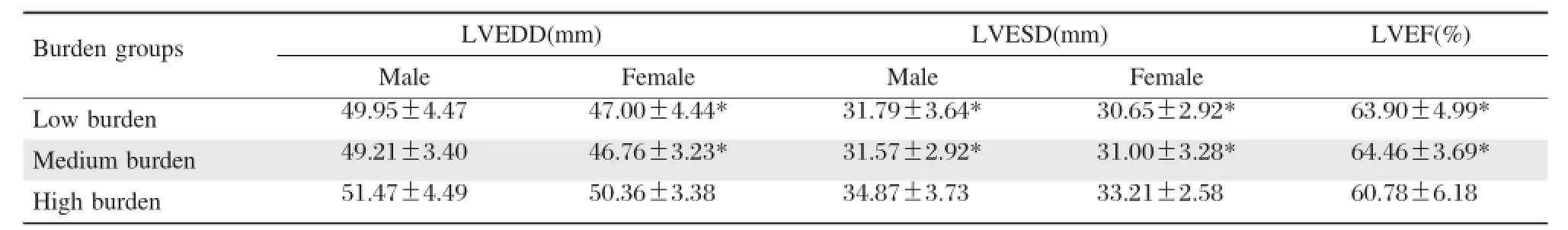
Table 5 Different burdens and LVEDD,LVESD and LVEF
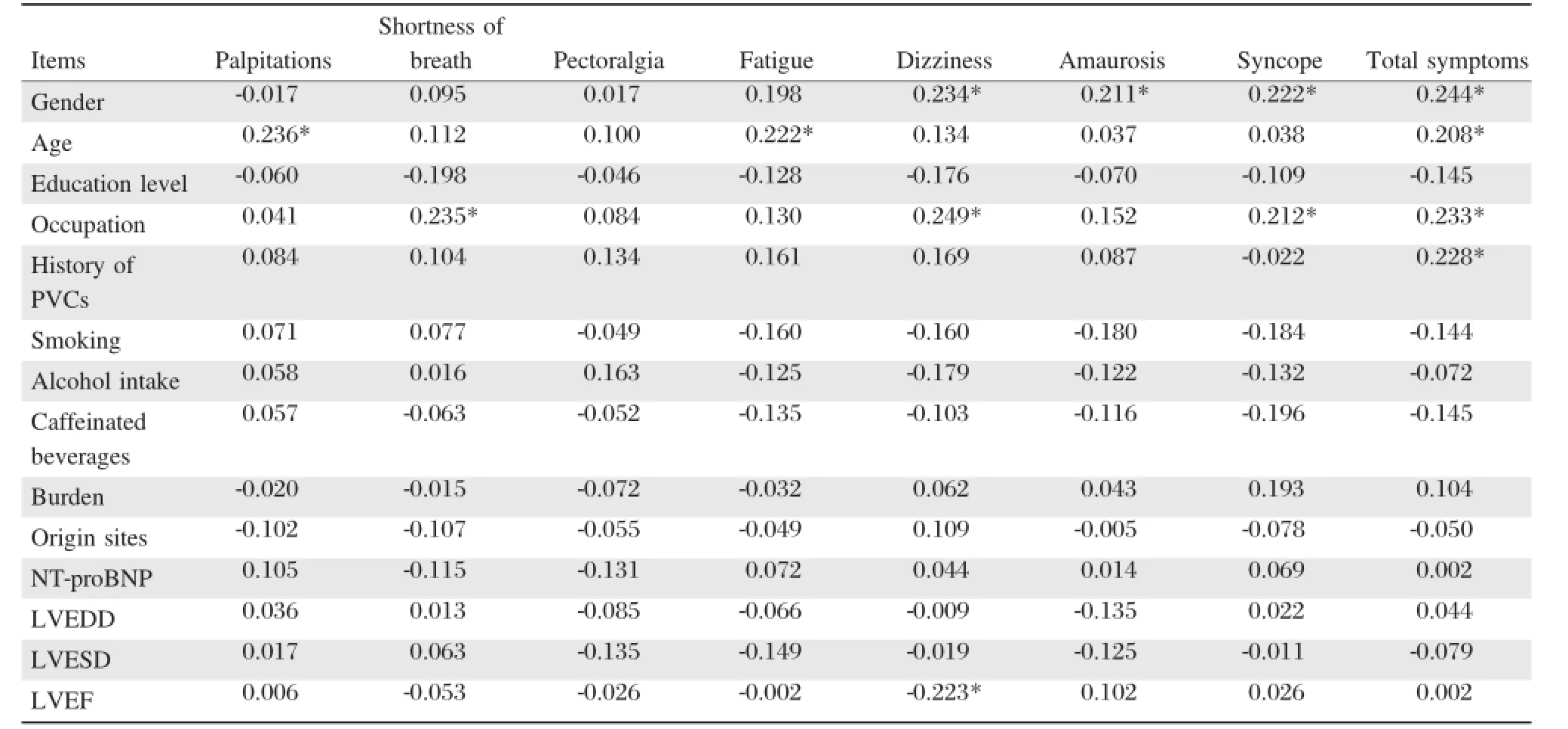
Table 6 Correlations of characteristics,burden,origin sites and left ventricular function parameters with symptoms
PVCs in moststructuralheartdiseases are originated from the leftventricle,whereas PVCs in mostpatients withoutstructuralheartdisease are originated from the rightventricle.Farzaneh etal.have demonstrated that, in patients without structural heart disease,80%PVCs were originated from the right ventricule,while the remaining 20%were originated from the LV[26].For those PVCs originated from the right ventricle,most of them are originated from RVOT,which is similar to ourfinding.RVOT wasthe mostcommon origin site (46.1%).LVOT was the second mostcommon origin site(22.6%).Our study also revealed that the PVCsoriginated from the tricuspid annulus had the largestburden,and the PVCs originated from the fascicle and the LV papillary muscle had the lowest burden(both less than 20%)than other sites.This is unique and different from the previous findings[21],which did not find any association between PVC burden and origin sites.This may be attributed to that a single 24-hour recording may not reflect the true PVC burden.In our study,we carried out 7-day Holter recording for all patients.
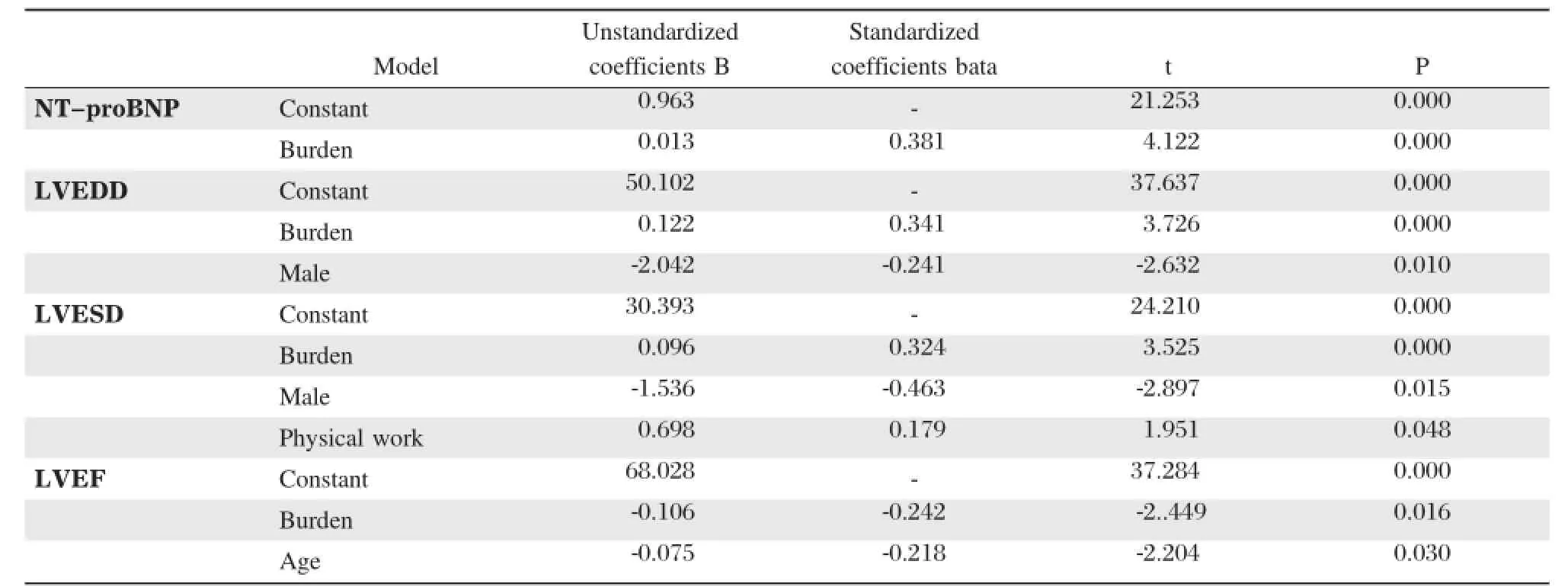
Table7 The regression analysis coefficients of predictors of NT-proBNP,LVEDD,LVESD and LVEF level in 102 PVCs patients
BNP or NT-proBNP is an important indicator for LV dysfunc tion a nd ea rly diagnosis of he art failure[27].BNP and NT-pro BNP are cardiovascular biomarkers that are released from cardiomyocytes in response to increases in ventricular wall stress[28]. Wallstress in a chamber is directly related to the diameter of the chamber and the transmural pressure and inversely related to the thickness ofthe wall[29].Recent evidence suggested that BNP can be used as a biomarker for non-heart failure mechanisms,preclinical diseases,and other pathologic states of myocardial disease[30-31].In this study,we demonstrated that the NT-pro BNP level of PVC patients originated from RVOT was lower than that from LVOT.This is supported by ourfindings and previous studies.Tada etal. reported thathigh BNP concentration was found more often in I-VT/PVCs originated from the LV than those from the rightventricle[32].This is similar to our finding,but we also found that patients with PVCs originated from the tricuspid annulus had the highest rate of higher NT-proBNP level.To our knowledge,this is the unique finding that patients with PVCs originated from the tricuspid annulus had the highest burden and NT-proBNP levelthan those from other foci. Our study also revealed that all patients with PVCs originated from the fascicle and the LV papillary muscle had a normal NT-pro BNP level.Patients with PVCs originated from the LV papillary muscle and the fascicle had higher LVEF butlower LVESD than those from other foci.This is not unique and is very similar to previous findings[21].Freddy et al.found a minority of patients with left-anterior or left-posterior fascicular PVCs had higher LVEF as compared to those with PVCs from other foci[21].
With the"bio-psycho-social"medicalmodel,healthrelated quality oflife isincreasingly used asa comprehensive index system to evaluate the efficacy endpoint,disease outcome and treatment outcomes.Although PVCs are notdirectly life-threatening,its onsetofclinicalsymptoms(such pectoralgia,palpitations,syncope,and etc.) seriously affectthe quality oflife in these patients,severe cases can lead to arrhythmogenic cardiomyopathy,even increase risk of sudden death.The symptoms seriously affected patients with PVCs in mentaland psychological aspects.Our study revealed thatfemale,older age,physical work,history of PVCs and NT-proBNP levels had significantly positive correlation with symptoms of PVC patients.Though males usually have a larger LVEDD and LVESD,there is a trend thatfemale patients with PVCs have reported more symptoms than male patients.It may be due to the social role function which males played made their threshold increases of complained physical discomfort,the discomfort of PVCs can be tolerated generally.Physiological differences made female patients more sensitive to physicalstimulus, and the discomfortsymptomsincreased the psychological pressure.Studies have shown that when the symptoms disappeared,the quality of life in patients with PVCs were increased,and the improvementwas more obvious in female than in male[33-34].Regression analysis also revealed that physical work was predictors of larger LVESD.PVCs patients whose work involves physical labor suffered more symptoms than mental worker. This may be attributed to the factthatphysicalworkers are engaged in more physicalactivitiesthan mentalworkers,which could induce the PVCsepisodes.Thisinterpretation is supported by previousstudies[35-37].Olderage was a predictor of lower LVEF,and that is why they had much more symptoms than young people.Patients with longer history of PVCs and higher NT-proBNP levels generally have more symptoms than those with shorter history of PVCs and lower NT-proBNP levels because of poor LV function[27-28].The other finding from our study was thathigher burden was a predictor of higher level of NT-porBNP,larger LVEDD,larger LVESD, and lower LVEF,which is very similar to the finding of previous studies[32,38].
The study limitations are listed as follows:the sample size ofthe patientpopulation was relatively smalland the data was collected from only one academic hospital ofone geographicallocation.Although in ourrecruited patients,there were 32 cases who underwentradiofrequency ablation,furtherfollow-up is needed to find out ifthere isa difference among differentorigin sitesand burden groups.Moreover,we did notassess the variety of PVCs in this study.Furthermore,the quality oflife was notevaluated in patients with PVCs.Furtherstudies are necessary to addressthese limitations.
In conclusion,ourresultsdemonstrated thatPVCswith lower burden or their origin from LV papillary muscle and fascicle were benign,while PVCswith higherburden ortheirorigin from tricuspid annulus may lead to cardiac dysfunction.Healthcare education should therefore be given to those PVC patientswho are olderin age,female, physicalworker,with long history of PVCs and high serum NT-proBNP levels so as to release the pressure caused by symptoms.Older in age,male,physicalworkand high burden patientsshould be followed up in case of decrease in LV function.
Acknowledgements
This work was supported by the innovation project in Jiangsu province,China,and the Program for Developmentof Innovative Research Team in the First Affiliated Hospital of NJMU(IRT-004).The funders had no role in study design,data collection and analysis,decision to publish,or preparation of the manuscript.
The authors gratefully acknowledge Qiang Tian, Rundi Qi,Cheng Wang,Xiaong Li,Fengxiang Zhang and Jing Wang for their contribution to this study as data collectors.Thanks for Professor Zuwen Zhang from Hangzhou Shaoyifu Hospital for kindly insructing the use of Cardio Trak CT Series Holter recorder. Finally,we express our sincere gratitude to the patients who participated in this study.
[1]Kennedy HL,Whitlock JA,Sprague MK,etal.Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy[J].N Engl J Med,1985, 312(4):193-197.
[2]Ng GA.Treating patients with ventricu lar ectopic beats[J].Heart,2006,92(11):1707-1712.
[3]Sheldon SH,Gard JJ,Asirvatham SJ.Premature ventricular contractions and non-sustained ventricular tachycardia: association with sudden cardiac death,risk stratification, and management strategies[J].Indian Pacing Electrophysiol J,2010,10(8):357-371.
[4]Gaita F,Giustetto C,Di Donna P,etal.Long-term followup ofrightventricularmonomorphic extrasystoles[J].J Am Coll Cardiol,2001,38(2):364-370.
[5]Blaauw Y,Pison L,van Opstal JM,et al.Reversal of ventricular premature beat induced cardiomyopathy by radiofrequency catheter ablation[J].Neth Heart J,2010, 18(10):493-498.
[6]Yarlagadda RK,Iwai S,Stein KM,et al.Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract[J].Circulation,2005,112(8):1092-1097.
[7]Taieb JM,Maury P,Shah D,etal.Reversalof dilated cardiomyopathy by the elimination of frequent left or right premature ventricular contractions[J].J Interv Card Electrophysiol,2007,20(1-2):9-13.
[8]Bogun F,Crawford T,Reich S,et al.Radiofrequency ablation of frequent,idiopathic premature ventricular complexes:Comparison with a control group without intervention[J].Heart Rhythm,2007,4(7):863-867.
[9]Bhushan M,Asirvatham SJ.The conundrum of ventricular arrhythmia and cardiomyopathy:Which abnormality came first[J].Curr Heart Fail Rep,2009,6(1):7-13.
[10]Herczku C,Kun C,Edes I,et al.Radiofrequency catheter ablation ofpremature ventricular complexes improved left ventricular function in a non-responder to cardiac resynchronization therapy[J].Europace,2007,9(5):285-288.
[11]Efremidis M,Letsas KP,Sideris A,et al.Reversal of premature ventricular complex-induced cardiomyopathy following successful radiofrequency catheter ablation[J]. Europace,2008,10(6):769-770.
[12]Ashikaga K,Tsuchiya T,Nakashima A,et al.Catheter ablation of premature ventricular contractions originating from the His bundle region[J].Europace,2007,9(9):781-784.
[13]Kanei Y,Friedman M,Ogawa N,et al.Frequent premature ventricular complexes originating from the rightventricular outflow tract are associated with left ventricular dysfunction[J].Ann Noninvasive Electrocardiol,2008, 13(1):81-85.
[14]Rhee KH,Jung JY,Rhee KS,etal.Tachycardiomyopathy induced by ventricular premature complexes:complete recovery after radiofreq uency catheter ablation[J]. Korean J Intern Med,2006,21(3):213-217.
[15]Ezzat VA,Liew R,Ward DE.Catheter ablation of premature ventricular contraction-induced cardiomyopathy[J]. Nat Clin Pract Cardiovasc Med,2008,5(5):289-293.
[16]Lee GK,Klarich KW,Grogan M,etal.Premature ventricular contraction-induced cardiomyopathy:a treatable condition[J].Circ Arrhythm Electrophysiol,2012,5(1): 229-236.
[17]Shanmugam N,Chua TP,Ward D.‘Frequent’ventricular bigeminy-a reversible cause of dilated cardiomyopathy. How frequent is'frequent'[J].Eur J Heart Fail,2006, 8(8):869-873.
[18]Baman TS,Lange DC,Ilg KJ,etal.Relationship between burden ofpremature ventricular complexes and leftventricular function[J].Heart Rhythm,2010,7(7):865-869.
[19]Takemoto M,Yoshimura H,Ohba Y,et al.Rad iofrequency catheter ablation of premature ventricular complexes from right ventricular outflow tract improves left ventricular dilation and clinical status in patients without structural heart disease[J].J Am Coll Cardiol,2005, 45(8):1259-1265.
[20]Hasdemir C,Ulucan C,Yavuzgil O,et al.Tachycardiainduced cardiomyopathy in patients with idiopathic ventricular arrhythmias:the incidence,clinical and electrophysiological characteristics,and the predictors[J]. J Cardiovasc Electrophysiol,2011,22(6):663-668.
[21]Freddy DCM,Syed FF,Noheria A,et al.Characteristics of premature ventricular complexes as correlates of reduced leftventricular systolic function:Study of the burden,duration,coupling interval,morphology and Site of Origin of PVCs[J].J Cardiovasc Electrophysiol,2011, 22(7):791-798.
[22]Tabatabaei N,Asirvatham SJ.Supravalvar arrhythmia: Identifying and ablating the substrate[J].Circ Arrhythm Electrophysiol,2009,2(3):316-326.
[23]Asirvatham SJ.Correlative anatomy for the invasive electrophysiologist:outflow tract and su pravalvar arrhythmia[J].J Cardiovasc Electrophysiol,2009,20(8): 955-968.
[24]Jia L,Yue-Chun L,Kang-Ting J,et al.Premature ventricularcontractions originating from the leftventricularseptum:results of radiofrequency catheter ablation in twenty patients[J].BMC Cardiovasc Disord,2011,11(2):27.
[25]Sun Y,Blom NA,Yu Y,etal.The influence of premature ventricular contractions on left ventricular function in asymptomatic children without structural heart disease: An echocardiographic evaluation[J].Int J Cardiovasc Imaging,2003,19(4):295-299.
[26]Farzaneh-Far A,Lerman BB.Idiopathic ventricular outflow tract tachycardia tachycardia[J].Heart,2005,91(2): 136-138.
[27]Morrow DA,Cannon CP,Jesse RL,et al.National academy of clinicalbiochemistry laboratory medicine practice guidelines:clinical characteristics and utilization of biochemical markers in acute coronary syndrome[J].Clin Chem,2007,53(4):552-574.
[28]De Lemos JA,Mc Guire DK,Drazner MH.B-type natriuretic peptide in cardiovascular disease[J].Lancet, 2003,362(9380):316-322.
[29]Munagala VK,Burnett JC Jr,Redfield MM.The natriuretic peptides in cardiovascular medicine[J].Curr Probl Cardiol,2004,29(12):707-769.
[30]McKie PM,Burnett JC Jr.B-type natriuretic peptide as a b iomark er beyond heart failure:Sp eculations and opportunities[J].Mayo Clin Proc,2005,80(8)1029-1036.
[31]Wang TJ,Larson MG,Levy D,et al.Plasma natriuretic peptide levels and the risk of cardiovascular events and death[J].N Engl J Med,2004,350(7):655-663.
[32]Tada H,Ito S,Shinbo G,et al.Significance and Utility of Plasma Brain Natriuretic Peptide Concentrations in Patients with Idiopathic Ventricular Arrhythmias[J]. Pacing Clin Electrophysiol,2006,29(12):1395-1403.
[33]Wool CA,Barsky AJ.Do women somatize more than men?Gender differences in somatization[J].Psychosomatics,1994,35(5):445-452.
[34]Kroenke K,Spitzer RL.Gender differences in the reportin g o f p h y sical an d so mato fo rm sy mp to ms[J]. Psychosom Med,1998,60(2):150-155.
[35]Joseph E.M,Veena S,Grant V.C,et al.Prevalence and prognostic significance of exercise-induced non-sustained ventricular tachycardia in asymptomatic volunteers:the Baltimore Longitudinal Study of Aging[J].J Am Coll Cardiol,2013,62(7):595-600.
[36]Yang JC,Wesley RC Jr,Froelicher VF.Ventricular tach ycardia d uring rou tine tread mill testing.Risk and prognosis[J].Arch Intern Med,1991,151(2):349-353.
[37]Morshedi-Meibodi A,Evans JC,Levy D,et al.Clinical correlates and prognostic significance of exercise-induced ventricular premature b eats in the community:th e Framingham Heart Study[J].Circulation,2004,109(20): 2417-2422.
[38]Sajadieh A,Nielsen OW,Rasmussen V,et al.Increased ventricular ectopic activity in relation to C-Reactive Protein,and NT-Pro-Brain natriuretic peptide in subjects with no apparent heart disease[J].Pacing Clin Electrophysiol,2006,29(11):1188-1194.
ΔWenhua Xu and Mingfang Li contributed equally to this work
✉Corresponding author:Prof.Hong Wang,Nanjing MedicalUniversity, the First Affiliated Hospital of Nanjing Medical University,300 Guangzhou Road,Nanjing,Jiangsu 210029,China.Tel/Fax:+86-25-83781867/+86-25-83781867 E-mail:hongwang@njmu.edu.cn;Prof. Yan Cui,Nursing College of Nanjing Medical University,Nanjing210029,140 Hanzhong Road,Nanjing,Jiangsu 210029,China.Tel/Fax: +86-25-83717168/+86-25-83717168,E-mail:cyan@njmu.edu.cn.
Received 02 March 2015,Revised 10 April 2015,Accepted 10 June 2015,Epub 15 June 2015
R331.3+6,Document code:A
The authors reported no conflict of interests.
©2015 by the Nanjing Medical University Press.All rights reserved.
 THE JOURNAL OF BIOMEDICAL RESEARCH2015年6期
THE JOURNAL OF BIOMEDICAL RESEARCH2015年6期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Platelets in hemostasis and thrombosis:Novelmechanisms of fibrinogen-independent platelet aggregation and fibronectinmediated protein wave of hemostasis
- Retinolbinding protein 4 correlates with and is an early predictor of carotid atherosclerosis in type 2 diabetes mellitus patients
- CC-chemokine receptor 7 and its ligand CCL19 promote mitralvalve interstitialcellmigration and repair
- Prevention ofatrialfibrillation with renin-angiotensin system inhibitors on essentialhypertensive patients:a meta-analysis of randomized controlled trials
- Epirubicin-gold nanoparticles suppress hepatocellular carcinoma xenograft growth in nude mice
- A susceptibility locus rs7099208 is associated with non-obstructive azoospermia via reduction in the expression of FAM160B1
