持续正压通气治疗癫合并阻塞性睡眠呼吸暂停综合征
赵 勇 时宝林 吴春丽 张晓霞 张言镇
赵 勇 时宝林△吴春丽 张晓霞 张言镇
目的 探讨持续正压通气(CPAP)对癫合并睡眠呼吸暂停综合征(OSA)患者癫发作频率的影响。方法42例癫合并OSA患者根据是否能够耐受呼吸机分为持续正压通气(CPAP)组20例和药物组22例,CPAP组给予CPAP加抗癫药物治疗,药物组给予抗癫药物治疗,比较2组治疗前与治疗4周和24周时的癫发作频率和呼吸暂停低通气指数(AHI)。结果2组治疗前癫发作频率和AHI差异无统计学意义(均P>0.05),CPAP组在治疗后4周和24周较治疗前发作频率明显减少(P<0.01),而药物组在治疗后4周和24周较治疗前发作频率无明显减少(P>0.05),治疗后4周和24周时,CPAP组的癫发作频率明显低于药物组(P<0.01),治疗24周后,CPAP组的AHI明显下降(P<0.01),而药物组AHI无变化(P>0.05)。结论CPAP治疗癫合并OSA患者,短期和长期均能明显减少癫发作。
睡眠呼吸暂停,阻塞性;癫;连续气道正压通气;药物疗法
阻塞性睡眠呼吸暂停综合征(OSA)可导致睡眠结构的破坏和睡眠剥夺,成人癫中有15.2%可合并OSA[1],剥夺睡眠可明显加重癫的发作,睡眠不足是癫的重要诱发因素[2]。有研究认为,控制OSA,增加供氧可有效控制癫合并OSA患者的发作[3],但国内相关研究少见,本研究拟通过持续正压通气(CPAP)添加治疗,改善癫合并OSA患者睡眠结构,减少癫发作。
1 资料与方法
1.2 分组 根据2011年4月中华医学会呼吸分会睡眠呼吸疾病学组制定的《阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)》标准[4],由呼吸内科、耳鼻喉科主治医师以上的2人共同分析结果,根据呼吸暂停低通气指数(AHI,次/h)和夜间血氧饱和度SpO2将受检者分为正常、轻、中、重度4组。轻度:AHI 5~15,夜间最低SaO20.85~0.90;中度:AHI>15~30,夜间最低SaO20.80~<0.85;重度:AHI>30,夜间最低SaO2<0.8。癫合并OSA患者共42例(5.7%)入组,均为中、重度OSA。42例均未进行正规药物治疗,其中男32例,女10例,年龄23~75岁,平均(51.83±13.17)岁;发病年龄23~65岁,平均(46.18±12.49)岁;病程0~12年,平均(5.07±3.49)年;均无热惊厥史,其中2例为同胞姐弟,余无癫家族史;发作频率为1次/月~12次/月;发作类型均为全身强直-阵挛性发作,其中30例为夜间发作,12例为白天夜间均有发作。42例患者均行头颅CT或MRI检查,均未见明显致灶,所有患者均行动态脑电图(AEEG)检查:所有患者均提示有背景慢活动,25例有癫样放电。根据患者是否能耐受呼吸机分为2组:CPAP组20例,给予CPAP加抗癫药物治疗;药物组22例,给予抗癫药物治疗,2组年龄、性别、AHI、ESS评分、体质量指数(BMI)、脑电图是否放电,是否睡眠发作,癫发作频率差异无统计学意义(P<0.05),具有可比性,见表1。
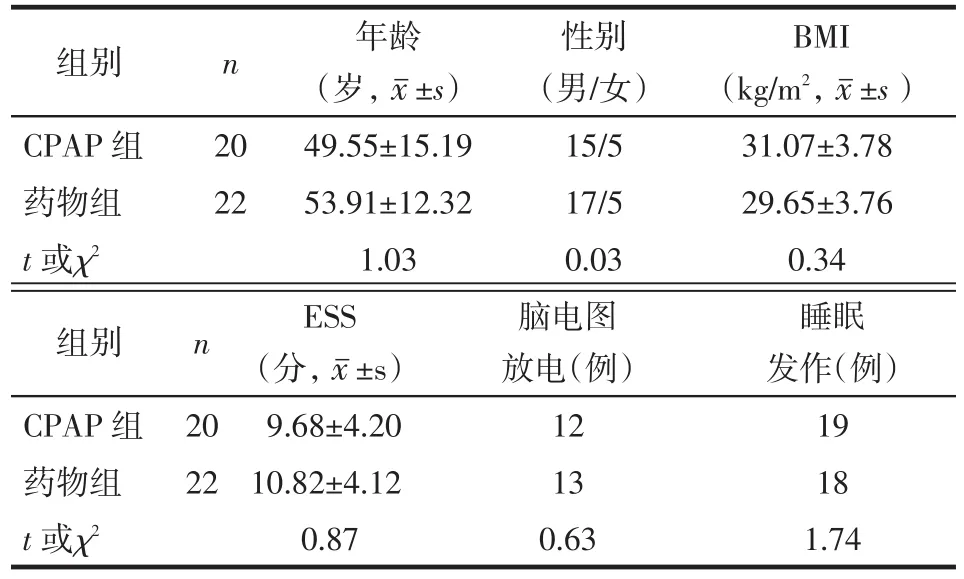
Tab.1 Comparison of clinical feature between two groups表1 2组患者临床资料比较
1.3 治疗过程 应用美国邦德(Rem Brandt)公司19导睡眠监测系统(Monet 19导)对2组患者进行睡眠监测,监测夜间睡眠9 h以上,患者不能服安眠药、饮酒、喝茶,同时记录血压、脑电图、心电图、胸腹式呼吸频率、眼动、腿动、口鼻气流、血氧饱和度、鼾声记录及体位等变化,记录结果经电脑自动分析后,再经人工校正。治疗:询问患者入组前8周癫的发作频率作为基线,做好癫发作频率记录,所有患者均给予基础治疗,包括减肥、侧卧位睡眠、戒烟酒、勿服镇静安眠药物、保持鼻腔通畅等。CPAP组在专业呼吸机中心医生的指导下进行,应用飞利浦伟康持续正压呼吸机,将呼吸机调定到适当的压力,以解决他们的呼吸暂停和低通气,患者均整夜戴呼吸机睡眠。药物组仅给予抗癫药物治疗,每周对患者进行电话随访或门诊随访,询问患者是否遵医嘱进行药物治疗或呼吸机治疗的依从性和不良反应,共观察24周。考察2组治疗后4周、24周癫发作频率、PSG、AHI及血药浓度。
1.4 统计学方法 采用SPSS 16.0进行统计分析。对正态分布的计量资料采用±s表示,2组间计量资料比较采用t检验。计数资料采用例(%)表示,组间比较用χ2。等级资料、非正态分布计量资料用Wilcoxon符号秩和检验及Mann-Whitney U检验,以P<0.05为差异有统计学意义。
2 结果

Tab.2 Comparison the seizure frequency of two groups before and after therapy表2 2组治疗前后癫 发作频率的比较[次/月,M(P25,P75)]
2.2 2组治疗前后AHI和发作频率比较 见表3。CPAP组治疗后AHI较治疗前降低(P<0.01),而药物组治疗前后AHI无变化(P>0.05)。CPAP组治疗后发作频率较治疗前减少(P<0.01),而药物组治疗前后无明显变化(P>0.05)。
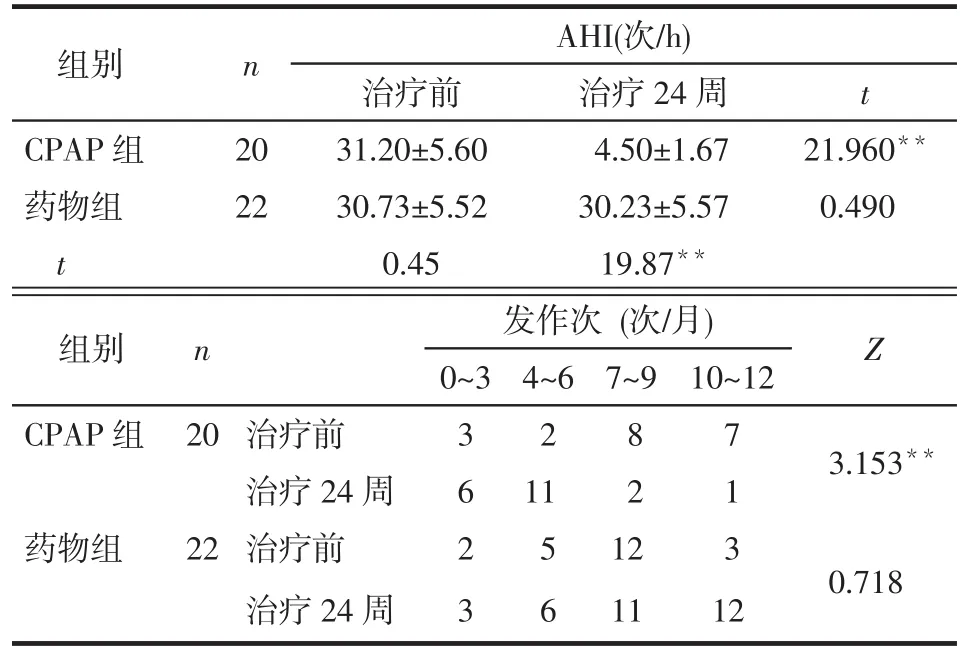
Tab.3 Comparison AHI and seizure frequency of two groups before and after therapy表3 2组治疗前后AHI和癫 发作频率的比较
3 讨论
本研究结果显示,CPAP组治疗后AHI较治疗前降低,而药物组治疗前后AHI无变化,表明CPAP能有效地降低AHI,改善OSA。癫的发生和恶化与AHI升高有关,OSA可升高AHI,可能是癫发生和加重的促进因素[12]。OSA相关的缺氧可直接导致神经元兴奋性过高,神经网络破坏,在易感个体中可导致癫的发生[6]。性发作本身就会导致缺氧,且抗癫药可降低唤醒的阈值和上呼吸道肌张力,而这些都可加重OSA[12]。尤其是在那些原发性癫的患者,一些癫类型,如原发性全面性癫对睡眠剥夺比较敏感,所以治疗睡眠疾病能有效改善癫发作[3]。
[1]Li P,Ghadersohi S,Jafari B,et al.Characteristics of refractory vs. medically controlled epilepsy patients with obstructive sleep apnea and their response to CPAP treatment[J].Seizure,2012,21(9):717-721.
[2]Badawy RA,Curatolo JM,Newton M,et al.Sleep deprivation increases cortical excitability in epilepsy:syndrome-specific effects [J].Neurology,2006,67(6):1018-1022.
[3]Malow BA,Foldvary-Schaefer N,Vaughn BV,et al.Treating obstructive sleep apnea in adults with epilepsy:a randomized pilot trial[J].Neurology,2008,71(8):572-577.
[4]中华医学会呼吸病学分会睡眠呼吸疾病学组.阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)[J].中华结核和呼吸杂志,2012,35(1):9-12.
[5]Hollinger P,Khatami R,Gugger M,et al.Epilepsy and obstructive sleep apnea[J].Eur Neurol,2006,5(2):74-79.
[6]Chihorek AM,Abou-Khalil B,Malow BA.Obstructive sleep apnea is associated with seizure occurrence in older adults with epilepsy [J].Neurology,2007,69(19):1823-1827.
[7]Phillips MC,Costello CA,White EJ,et al.Routine polysomnography in an epilepsy monitoring unit[J].Epilepsy Res,2013,105(3): 401-404.
[8]Van Golde EG,Gutter T,De Weerd AW.Sleep disturbances in people with epilepsy;prevalence,impact and treatment[J].Sleep Med Rev,2011,15(6):357-368.
[9]Hitomi T,Oga T,Tsuboi T,et al.Transient increase in epileptiform discharges after the introduction of nasal continuous positive airway pressure in a patient with obstructive sleep apnea and epilepsy[J]. Intern Med,2012,51(17):2453-2456.
[10]Oliveira AJ,Zamagni M,Dolso P,et al.Respiratory disorders during sleep in patients with epilepsy:effect of ventilatory therapy on EEG interictal epileptiform discharges[J].Clin Neurophysiol,2000, 111(Suppl 2):S141-145.
[11]Vendrame M,Auerbach S,Loddenkemper T,et al.Effect of continuous positive airway pressure treatment on seizure control in patients with obstructive sleep apnea and epilepsy[J].Epilepsia,2011,52(11): e168-171.
[12]Derry CP,Duncan S.Sleep and epilepsy[J].Epilepsy Behav,2013,26 (3):394-404.
(2013-12-10收稿 2014-05-29修回)
(本文编辑 陆荣展)
Continuous Positive Airway Pressure Treatment for Epilepsy Complicated with Obstructive Sleep Apnea Syndrome
ZHAO Yong,SHI Baolin△,WU Chunli,ZHANG Xiaoxia,ZHANG Yanzhen Neurology Department,Weifang People’s Hospital,Weifang 261041,China
△
E-mail:shibaolin1975@sina.com
ObjectiveTo investigate the effect of continuous positive airway pressure(CPAP)on seizure frequency in epilepsy patients complicated with obstructive sleep apnea(OSA).MethodsSubjects were divided into CPAP group(20 subjects)and medication group(22 subjects)according to whether they can tolerate CPAP.CPAP group were treated with CPAP combined with antiepileptic drugs.Medication group were treated with antiepileptic drugs alone.Seizure frequency and apnea-hypopnea index(AHI)were compared between groups before and after 4 weeks and 24 weeks of treatment.ResultsBaseline seizure frequency and apnea-hypopnea index(AHI)were compared between groups(P>0.05).A significant reduction of seizure frequency was observed in CPAP group after 4 weeks and 24 weeks of treatment compared to that before treatment(P<0.01).In medication group,no significant difference in seizure frequency was noted betweem 4 weeks and 24 weeks after treatment compared to that before treatment(P>0.05).A significant reduction of AHI was observed in the CPAP group after 24 weeks of treatment compared to that before treatment(P<0.01),but no change of AHI by treatment was observed in medication group(P>0.05).ConclusionTreatment of OSA in patients complicated with epilepsy may improve seizure control in short and long term,but longer observation time and more samples are needed for further research.
obstructive sleep apnea;epilepsy;continuous positive airway pressure;drug therapy
R742.1
A
10.3969/j.issn.0253-9896.2014.12.023
潍坊市科学技术发展计划项目(201104086)
山东潍坊,潍坊市人民医院神经内科(邮编261041)△
E-mail:shibaolin1975@sina.com

