个案报道:三维适形消融治疗肝左叶胆管细胞癌1例
扈彩霞 郑加生 孙斌
·病例报告·
个案报道:三维适形消融治疗肝左叶胆管细胞癌1例
扈彩霞 郑加生 孙斌
肝细胞癌和胆管细胞癌是常见的两种肝脏肿瘤。不能切除的未经治疗的胆管细胞癌患者预后差,尤其是发生门静脉受侵的患者。目前胆管细胞癌尚无有效的治疗手段。射频消融(radiofrequency ablation, RFA)在不能进行手术切除的肝恶性肿瘤治疗中发挥重要作用,在此,我们报道成功运用射频消融治疗伴有门静脉癌栓的肝内胆管细胞癌一例,该患者共计存活26个月。
肝内胆管细胞癌,肿瘤栓子,射频消融
病例介绍
肝细胞癌和胆管细胞癌是常见的两种肝脏肿瘤。不能切除的未经治疗的胆管细胞癌患者预后差,尤其是发生门静脉受侵的患者,中位生存时间约为3个月[1]。主要死亡原因为疾病进展所致肝功能恶化、胆管炎和败血症,以及反复发作的胆道梗阻[2]。这些病人中大部分患者因为慢性肝病基础所致肝储备能力差或者肝内有多发病灶,故仅有少数患者能够进行手术切除。射频消融(radiofrequency ablation,RFA)在不能进行手术切除的肝恶性肿瘤治疗中发挥重要作用,在此,我们报道成功运用射频消融治疗伴有门静脉癌栓的肝内胆管细胞癌一例。
患者,女性,56岁,主因上腹不适伴有乏力15天入院。体格检查未见明显腹痛,既往有高血压病史,口服降压药,血压控制可。无肿瘤家族史。化验检查:谷丙转氨酶(ALT) 45.8U/L,谷草转氨酶(AST) 34.5U/L,总胆红素12.9umol/L,碱性磷酸酶(ALP)106.2U/L,CA19-9明显升高,到392.59U/mL (正常值<37 U/mL),其余抽血化验均正常。乙肝五项表面抗原、核心抗体阴性,丙型肝炎抗体阴性。腹部CT提示肝左叶病变,伴有门静脉受侵(图1)。肝占位穿刺活检病理结果为肝内胆管细胞癌,CK19,CD34,P53和CK8/18阳性表达(图2,3)。对其施行局部麻醉CT引导下射频消融治疗。
使用Celon三针对其进行消融。条件分别是:140千焦,34分钟;123千焦38分钟;120千焦30分钟;130千焦35分钟;131千焦35分钟,92千焦28分钟(图4)。射频消融结束后,行即时CT检查,了解有无出血、腹水等并发症发生。术后7天行腹部CT检查评价治疗效果。如果在消融区域发现残余病灶,进行再次消融治疗。该患者3个月内进行4次消融。最后患者获得完全消融,病灶周边有0.5-1cm消融边缘。最后患者整个左叶完全消融(图5)。
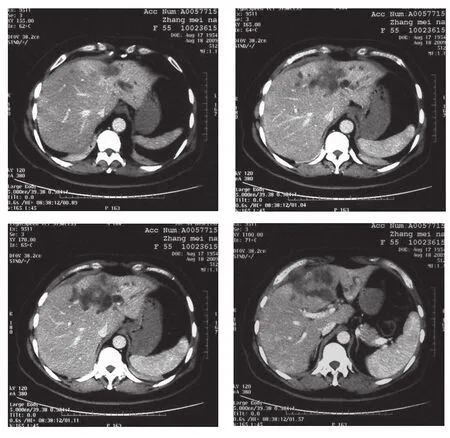
Figure 1.Contrast-enhanced CT images of 56-year-old woman with intrahepatic cholangiocarcinoma. It revealed left lobe of liver's lesions and left branch of portal vein was invasive.
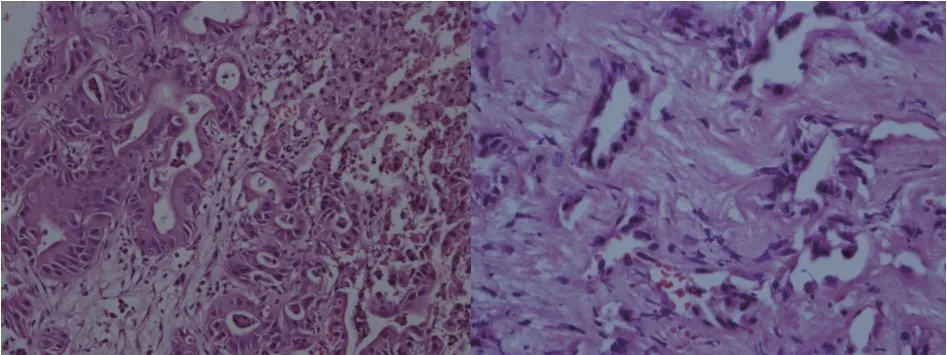
Figure 2.Original magnif i cations, ×200 and ×400,A,B. Hematoxylin and eosin staining showed morphologic evaluation of intrahepatic cholangiocarcinoma obtained from the patient.

Figure 3.Immunohistochemistry for Hepatocyte(C) and CK-19 (D)in the patient.Hepatocyte staining showed that cancer cells were generally negative. A diffusely positive staining was observed in the tumoral cells for CK-19.

Figure 4.CT guided percutaneous RFA. RFA of the tumor thrombus in the left portal vein and the whole left lobe of liver.
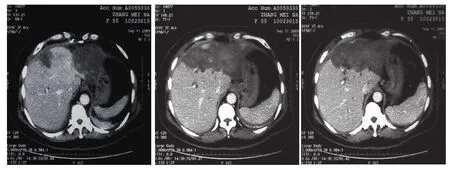
Figure 5.Follow up contrast-enhanced CT images after 6 months from the last time of RFA.The patient's left lobe of liver was ablated completely
讨论
胆管癌是原发性肝肿瘤中第二常见肿瘤,发生率高[3-5]。其恶性程度高,各种治疗效果差。胆管癌发生于胆管上皮细胞,沿着胆管可发生于任何部位。可分为肝内胆管细胞癌和肝外胆管细胞癌[6]。肝内胆管癌(ICC)的全球发病率在最近几十年来增加了2–6%。肝内胆管细胞癌因缺乏特异性症状,在诊断时多已发展至晚期,总体预后比肝外胆管细胞癌差[7-9]。ICC的诊断仍然是特别具有挑战性。目前唯一有效的治疗方法是手术。不幸的是,大多数患者在诊断时,疾病已经发展至晚期,失去手术切除机会[10-12]。大部分患者因为慢性肝病基础所致肝储备能力差或者肝内有多发病灶,故仅有少数患者能够进行手术切除[13]。并且,其对化疗也不敏感,大多数为乏血供肿瘤。肝动脉导管化疗栓塞(Transarterial chemoembolization,TACE)是通过增加病灶局部化疗药浓度来杀灭肿瘤细胞,从而减少化疗的全身副作用,故其对ICC的疗效很差。不管肿瘤血管分布怎样,经皮射频消融(RFA)对于不能手术切除的肿瘤患者是安全和有效的[14-17]。
在本病例中,患者门静脉左支受侵。CT引导下RFA治疗门静脉癌栓未见报道。在这例病例报告,我们成功完成了ICC合并门静脉癌栓的肝左叶完全消融。众所周知,肝癌患者合并有门静脉癌栓这预后极差,因为肿瘤生长迅速,常常伴有病灶肝内转移、肝功能恶化以及门脉高压所致上消化道出血等严重并发症。Fujii等[18]报道,合并门静脉癌栓患者,不管癌栓是在门脉左支、右支或主干,1年生存率为20.9%,2年生存率为6.2%。在本病例中,患者通过RFA联合TACE治疗,防止门静脉癌栓蔓延至主干,延长患者患者的生存期为26个月。其主要并发症为消融术后6个月发生肝内胆汁瘤,经过经皮胆汁瘤引流缓解症状。总之,RFA在一些不能手术切除的病例中可以成功控制局部肿瘤发展,在肝肿瘤的治疗中发挥重要作用。
1 Park J, Kim MH, Kim KP, et al. Natural history and prognostic factors of advanced cholangiocarcinoma without surgery, chemotherapy, or radiotherapy: a large-scale observational study. Gut Liver 2009;3 :298-305
2 Burger I, Hong K, Schulick R, et al. Transcatheter arterial chemoembolization in unresectable cholangiocarcinoma: initial experience in a single institution. J Vasc Interv Radiol2005 ;16 :353-361
3 Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33:1353-1357.
4 Taylor-Robinson SD, Toledano MB, Arora S, et al. Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales, 1968-1998. Gut. 2001;48:816-820.
5 Davila JA, El-Serag HB. Cholangiocarcinoma: the “other“ liver cancer on the rise. Am J Gastroenterol. 2002;97:3199-3200.
6 de Groen PC, Gores GJ, LaRusso NF, et al. Biliary tract cancers. N Engl J Med. 1999;341:1368-1378.
7 Park J, Kim MH, Kim KP, et al. Natural history and prognostic factors of advanced cholangiocarcinoma without surgery, chemotherapy, or radiotherapy: a large-scale observational study. Gut Liver 2009;3 :298-305
8 Burger I, Hong K, Schulick R, et al. Transcatheter arterial chemoembolization in unresectable cholangiocarcinoma: initial experience in a single institution. J Vasc Interv Radiol2005 ;16 :353-361
9 Nakeeb A, Tran KQ, Black MJ, et al. Improved survival in resected biliary malignancies. Surgery 2002;132 :555-563
10 Ben-Menachem T. Risk factors for cholangiocarcinoma. Eur. J. Gastroenterol. Hepatol.2007, 19, 615–617
11 Blechacz B. R., Gores G. J.Cholangiocarcinoma. Clin. Liver Dis. 2008,12, 131–150,
12 El-Serag H. B., Engels E. A., Landgren O., Chiao E., Henderson L., Amaratunge H. C., Giordano T. P.Risk of hepatobiliary and pancreatic cancers after hepatitis C virus infection: a population-based study of U.S. veterans. Hepatology,2009, 49, 116–123
13 Aljiffry M, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990–2009. World J Gastroenterol 2009;15 :4240-4262
14 De Baere T, Deschamps F, Briggs P, et al. Hepatic malignancies: percutaneous radiofrequency ablation during percutaneous portal or hepatic vein occlusion. Radiology 2008;248 :1056-1066
15 Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology 2009;49 :453-459
16 Stang A, Fischbach R, Teichmann W, Bokemeyer C, Braumann D. A systematic review on the clinical benef i t and role of radiofrequency ablation as treatment of colorectal liver metastases. Eur J Cancer 2009;45 :1748-1756
17 Meloni MF, Andreano A, Laeseke PF, Livraghi T, Sironi S, Lee FT Jr. Breast cancer liver metastases: US-guided percutaneous radiofrequency ablation—intermediate and long-term survival rates. Radiology 2009;253 :861-869
18 Fujii T, Takayasu K, Muramatsu Y, Moriyama N, Wakao F, Kosuge T, et al. Hepatocellular carcinoma with portal tumor thrombus: analysis of factors determining prognosis. Jpn J Clin Oncol 1993;23:105–9.
3-Dimension Conformal Technology Guided Radiofrequency Ablation of liver's left lobe for Intrahepatic Cholangiocarcinoma: A Case Report
Jiasheng Zheng,Caixia Hu, Bin Sun
Center of Minimally Invasive Intervention, Beijing You-an Hospital, Capital Medical University, Beijing 100069, P.R.China
Dr Jiasheng Zheng, Center of Minimally Invasive Intervention, Beijing You-an Hospital, Capital Medical University, Beijing 100069, P.R.China ;
Hepatocellular carcinoma and cholangiocarcinoma are the two most common malignant liver tumors.The prognosis for patients with untreated unresectable cholangiocarcinoma is depressed,especially to the patient with invasion in the portal vein. It has no effective treatment presently. Radiofrequency ablation (RFA) plays an importmant role in the treatment of unresectable liver tumors.It is considered a viable alternative to surgery for inoperable patients. Here,we report the successful use of CT- guided RFA in a patient with intrahepatic Cholangiocarcinoma with invasion in the portal vein.The patient survived for 26 months.
intrahepatic cholangiocarcinoma, tumor thrombus, radiofrequency ablation
2013-06-05)
(本文编辑:黄强)
10.3877/cma.j.issn.2095-5782.2014.03.018
100069 首都医科大学附属北京佑安医院介入中心
郑加生,Email: jiashengzheng@yahoo.com;

