Effect of sevoflurane on tissue permeability of lung ischemia-reperfusion injury in rats
Xiao-Hui Li, Zhong-Hua Liu, Hong-Bing Ma, Yong Li, Hui Zhao, Jian-Bo Che, Wei-Chao Liu, Gong-Ning Shi*
1Huaihe River Hospital, Henan University, Kaifeng 475000, Henan, China
2Medical School, Henan University, Kaifeng 475000, Henan, China
Effect of sevoflurane on tissue permeability of lung ischemia-reperfusion injury in rats
Xiao-Hui Li1, Zhong-Hua Liu2, Hong-Bing Ma, Yong Li1, Hui Zhao1, Jian-Bo Che1, Wei-Chao Liu1, Gong-Ning Shi1*
1Huaihe River Hospital, Henan University, Kaifeng 475000, Henan, China
2Medical School, Henan University, Kaifeng 475000, Henan, China
Objective: To investigate the effect of sevoflurane on tissue permeability of lung ischemiareperfusion injury (LIRI) in rats. Methods: A total of 45 wistar rats were randomly divided into 3 groups Ⅰ, Ⅱ, Ⅲ. Modified Eppinger method was adopted to establish the rat lung ischemiareperfusion injury model. GroupⅠ served as the control group, group Ⅱ as ischemia reperfusion group, group Ⅲ as sevoflurane ischemia-reperfusion group. Blood gas index, lung permeability index (LPI) change, lung tissue pathology change and lung water content were observed and compared between groups of rats at different time points. Results: During ischemia reperfusion, all rats kept balance of the MAP during different time points, SPO2of group Ⅱ and Ⅲ decreased significantly than Ⅰ group (P<0.05); after reperfusion lung permeability index in Group Ⅱ andⅢ was higher than the control group significantly (P<0.05), 120 min after reperfusion LPI change and injury of group Ⅲ was significantly lower than Ⅱ group (P<0.05); interstitial and alveolar cavity effusion in of group Ⅲ were lower than that of group Ⅱ. Conclusions: Sevoflurane pretreatment can reduce the lung tissue permeability, and LIRI plays a protective role in LIRI.
ARTICLE INFO
Article history:
Received 10 September 2013
Received in revised form 15 October 2013
Accepted 15 December 2013
Available online 20 April 2014
Sevoflurane
1. Introduction
Lung ischemia-reperfusion injury (LIRI) is clinical common in lung transplantation and extracorporeal circulation operation[1-3]. LIRI can lead to lung dysfunction, and is the leading cause of death after lung transplantation[4]. Studyhas showed that[5], enflurane and sevoflurane drugs play an important protective role in viscera reperfusion. Other studies have suggested[6] that sevoflurane pretreatment can significantly reduce the lung edema and inflammation induced by tissue endotoxin, and sevoflurane can protect on LIRI. This study aimed to observe the influence of sevoflurane on LIRI rat lung tissue permeability and the mechanism. We established the rat lung LIRI model, used sevoflurane pretreatment, observe its tissue permeability and the pathological changes, to provide the theory basis for clinical prevention and treatment of LIRI medication.
2. Materials and methods
2.1. Experimental animals
A total of 45 male, clean level, Wistar rats were selected, aged 8 to 10 weeks, weighting (251.3±42.5) g. They were provided by the laboratory animal center, class Ⅱ, and had free food and water. The experimental process strictly followed “regulations on the administration of experimental animals”.
2.2. Instrument and reagent
SLIRIecust730 pressure monitor (Siemens Germany); Detax gas monitor (Finland); NOVAbiomedical blood gas analyzer (United States); Optical microscope (BH-2) (Japan). 20% urethane (our center reagent); Sevoflurane (Baxter company, USA).
2.3. Model establishing
Eppinger method was used to establish LIRI model in ratsin vivo[7]. All rats had anesthesia with intraperitoneal injection of 20% urethane in supine position. The right lower limb groin skin had incision under local anesthesia, and right femoral vein was exposed. Sodium chloride was injected by infusion pump. After neck midline incision, trachea and left carotid artery was separated. Tracheotomy was performed for intubation, and animal breathing machine was used for mechanical ventilation. The parameters were adjusted according to the data. PaCO2was maintained at 35 to 45 mmHg. Left carotid artery blood pressure was monitored continuously and blood samples were collected at each time point. Vecuronium bromide amine was infused continuously to maintain anesthesia, and sevoflurane inhalation concentration was adjusted within 1 MAC (2.2%) in intraoperative sevoflurane preconditioning group. Thirty minutes after mechanical ventilation, the bottom left pulmonary ligament was cut off from the fifth rib in left side. Pulmonary hilar was exposed, and 50 U heparin was injected intravenously. Left pulmonary hilar was closed, and lung surface was rinsed with saline. Thoracic cavity was closed by suture, after 45 min blood flow was open.
2.4. Animal groups
A total of 45 Wistar rats were randomly divided into groupⅠ, Ⅱ, Ⅲ, with 15 in each. group Ⅰ served as the control group, without block after left pulmonary hilar opening; group Ⅱ as ischemia-reperfusion group, with perfusion 45 min after left pulmonary hilar blocking; group Ⅲ as sevoflurane ischemia-reperfusion group, with sevoflurane inhalation for 30 min and with perfusion 45 min after left pulmonary hilar blocking. There were three time points in each group, ischemia blocking for 45 min, 1 h and 2 h reperfusion. Five rats were sacrificed at each time point.
2.5. Indexes observation
0.5 mL of blood was collected for blood gas analysis at three time points, respectively. Lung wet dry weight ratio was detected[8]. Lung tissue was weighted as wet weight (W), then they were placed in the oven drying to record dry weight (D), to calculate the wet dry /weight ratio (W/D). Lung permeability index (LPI) value was obtained by using the Bradford method[9]. After perfusion, rats were sacrificed. 1 mm left lung tissue was selected, fixed, HE stained to observe changes in lung tissue;
2.6. Statistical analysis
SPSS12.0 statistics software was used to analyze data, measurement data were expressed as mean±SD, P<0.05 was considered as significant difference.
3. Results
3.1. PaCO2change
There was no statistical difference in PaCO2basic value between three groups (P>0.05); PaCO2decreased significantly in Ⅱ, Ⅲ group 60, 120 min after reperfusion (P<0.05), and compared with group Ⅰ the differences was statistically significant (P<0.05); decrease in Group Ⅱ at each time point was more significant than that of group Ⅲ, but there was no statistically significant difference (P>0.05) (Table 1).
3.2. Lung W/D detection
There was no statistical difference of rats W/D between three groups (P>0.05). 60, 120 min after reperfusion lung W/D in groupⅠhad no significant change compared with that at ischemia time (P>0.05); 60, 120 min after reperfusion W/D of Group Ⅱ and Ⅲ was significantly increased compared withthat of group Ⅰ (P<0.05). 60, 120 min after reperfusion W/D of Group Ⅱ was significantly increased compared with that of group Ⅲ (P<0.05) (Table 2).
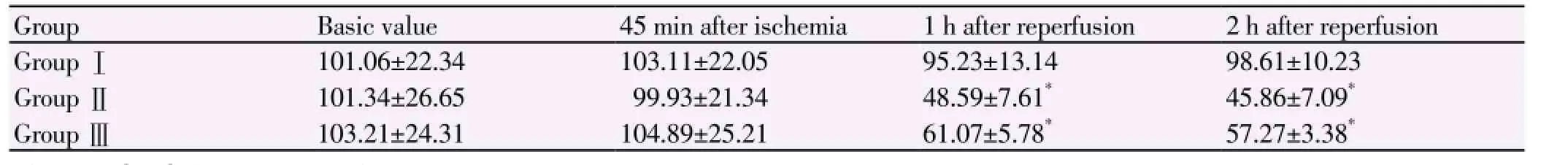
Table 1 PaCO2change of three groups at each time point (mmHg).

Table 2 Lung W/D.
3.3. LPI
120 min after reperfusionLPI of group Ⅱ[(2.73±0.09)%] andⅢ[(1.56±0.18)%] were significantly higher than group Ⅰ[(0.73 ±0.13)%] (P<0.05), and the difference was significant different between group Ⅲ and group Ⅱ (P<0.05).
3.4. Pathological observation
GroupⅠshowed normal lung tissue structure, a small amount of accidental effusion in alveolar space, capillary without congestion; group Ⅱshowed lung capillary expansion congestion, edema of broadening alveolar interval, infiltrated interstitial inflammatory cell, exudated red blood cells and inflammatory cells from alveolar lumen. Lung tissue structural damage was serious reperfusion after 120 min; group Ⅲ showed that lung tissue injury was reduced significantly than group Ⅱ, interstitial and alveolar cavity effusion reduced as shown in Figure 1.
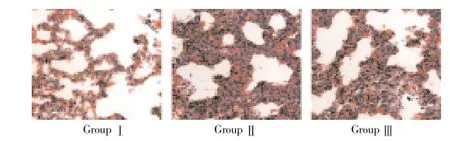
Figure 1. Pathological observation (HE×400).
4. Discussion
LIRI tends to occur in cardiopulmonary resuscitation, extracorporeal circulation, lung transplantation, and other circumstances. The pathogenesis is not yet clear. Some scholars reported that it is related with many factors, and acute LIRI is important factors affecting postoperative recovery[10-13]. After rebuilding blood supply, lung tissue damage is aggravating[14]. Therefore, the effective prevention and control measure is hot spot of clinical research. Studies have shown that[15-17], pretreatment with drugs can significantly reduce the degree of lung injury. This study Eppinger method is adopted to establish the LIRI rats model in vivo. Pathological changes of lung tissue were obvious, and lung capillary hyperemia and expansion were obvious after reperfusion. Alveolar cavities erythrocyte effused in great quantities, followed with interstitial edema and inflammatory cells infiltration, showing LIRI model was successfully established.
Sevoflurane inhalation anesthesia is common. Studies have shown that[18-20], it can improve the lung injury caused by endotoxin, alleviate endotoxin induced lung edema and inflammatory cell infiltration, without influence on regular inhalation of lung tissue. In this study, PaCO2of group Ⅱdecreased significantly after infusion. It may be related to increasing capillary permeability after lung ischemia reperfusion, which lead to pulmonary interstitial edema, blood flow to the ventilation/dysfunction ratio[21-23]; In GroupⅢafter sevoflurane pretreatment, PaCO2was increased slightly, showing that LIRI has certain protective effect. LPI is the main indicators for lung tissue protein permeability. In this study, LPI of group Ⅱ after reperfusion was increased most significantly. LPI in group Ⅲ decreased significantly pretreatment than Ⅱ group after sevoflurane inhalation. It also shows that sevoflurane pretreatment can decrease the LPI rising degree. The lung D/W ratio in group Ⅲ was lower than that in group Ⅱ, the result changes were positively related to the level of the LPI changes, showing sevoflurane pretreatment can reduce pulmonary vascular permeability after reperfusion. The lung tissue can play a protective role. HE staining showed that, tissue damage degree in the groupⅢwas significantly lighter than group Ⅱ, which confirmed protection effect of sevoflurane pretreatment on LIRI.
According to the results of this study, pretreatment with sevoflurane can improve tissue permeability of lung ischemia-reperfusion injury in rats, to protective LIRI lung tissue.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Mukherjee S, Kim S, Gibbons LE, Nho K, Risacher SL, Glymour MM, et al. Genetic architecture of resilience of executive functioning. Brain Imaging Behav 2012; 6(4): 621-633.
[2] Melotte V, Qu X, Ongenaert M, van Criekinge W, de Bruïne AP, Baldwin HS, et al. The N-myc downstream regulated gene (NDRG) family: diverse functions, multiple applications. FASEB J 2010; 24(11): 4153-4166.
[3] Sun Z, Shen L, Sun X, Han T, Yang G, Zhang J, et al. VaLIRIation of NDRG2 and c-Myc expression in rat heart duLIRIng the acute stage of ischemia/reperfusion injury. Histochem Cell Biol 2011; 135(1): 27-35.
[4] Chen J, Shen BY, Deng XX, Zhan Q, Peng CH. SKP1-CULLIN1-F-box (SCF)-mediated DRG2 degradation facilitated chemotherapeutic drugs induced apoptosis in hepatocellular carcinoma cells. Biochem Biophys Res Commun 2012; 420(3): 651-655.
[5] Sun JF, Zhao ZY, Huo DS. Protection of mulsified isoflurane preconditioning on rat lung ischemia-reperfusion injury. J Chin Med Sci 2013; 3(l): 40-41.
[6] Yang B, Chen GK, Li WH, Wang WC, Ge P, Kang Y, et al. NDRG2 expression in rat lung ischemia-reperfusion injury. Modern Biomed Progr 2013; 13(5): 828-829.
[7] Hengst WA, Gielis JF, Lin JY, Van Schil PE, De Windt LJ, Moens AL. Lung ischemia-reperfusion injury:a molecular and clinical view on a complex pathophysiological process. Am J Physiol-Heart Ciricul Physiol 2010; 299(5): H1283-H1299.
[8] Linfert D, Chowdhry T, Rabb H. Lymphocytes and ischemiareperfusion injury. Transplantation Rev 2009; 23(1): 1-10.
[9] Xia ZY, Gao J, Ameer KA. Protective effect of ischemic postconditioning on lung ischemia-reperfusion injury in rats and the role of heme oxygenase-1. Chin J Traum 2009; 12(3): 162-166.
[10] Fan K, Wang JJ, Zhai W, Tang J, Wan L. Improved three casing method to establish the left lung orthotopic transplantation model in rats. J Tissue Eng Res Clin Reh Chin 2010; 14(44): 8183-8185.
[11] Zheng ZK, Li JS, Wang JJ, Jiang K, Zhang J, Qiao XW. Establishing and evaluation of lung ischemia-reperfusion injury in mice model. J Huazhong Univ Sci Technol (Med Sci) 2011; (6): 727-729.
[12] Yang M, Xu L, Ren BH, Chen J, Jiang F, Ding ZH, et al. Characteristics of nilateral pulmonary circulation block to the lung ischemia/reperfusion injury. J Med Graduate Students 2009; 22: 592-595.
[13] Yang SJ, Wang GN, Ping W, Jiang WY, Xu CC, Chen WS, et al. Establishing and evaluation of lung ischemia-reperfusion acute injury model in mice. Chin Med Tribune 2013; 15(5): 858-860.
[14] Duan MK, Wang JW, Lan JB, Xu SS, Xiong W, Wu YG, et al. The effect and the mechanism study of ischemic postconditioning reduction after lung ischemia-reperfusion injury. J Shandong Med 2013; 53(14): 15-16.
[15] Bogoyevitch MA, Ngoei KR, Zhao TT. c- Jun N- ter-minal kinase ( JNK) signaling: recent advances and chal-lenges. Biochim Biophys Acta 2010; 1804(3): 463-475.
[16] Sun XD, Liu XG.. Curcumin induces apoptosis of pancreatic cancer by inhibiting Ras-ERK and Shh-GLI1 signal. Chinese J Pathophysiol 2012; 28(6): 996- 1000.
[17] Kuang YP, Chen K, He BH, Wang LJ, Zhu AZ, Liu CC, et al. Photosensitization of curcumin induced gastric cancer MGC - 803 cells apoptosis. Chin J Pathophysiol 2012; 28(7): 1247- 1252.
[18] Yucel AF, Kanter M, Pergel A. The role of curcu-min on intestinal oxidative stress,cell proliferation and apoptosis after ischemia / reperfusion injury in rats. J Mol Histol 2011; 42(6): 579- 587.
[19] Zanotti G, Casiraghi M, Abano JB, Tatreau JR, Sevala M, Berlin H, et al.Novel cLIRItical role of Toll- like receptor 4 in lung ischemia-reperfusion in-jury and edema. Am J Physiol Lung Cell Mol Physiol 2009; 297(1): L52- L63.
[20] Qiu XX, Song ZJ, Dai YY, Fang ZX, Wang WT. Influence of notoginseng total saponin on apoptosis and c-Jun the amino terminal kinase in lung ischemia/reperfusion injury. J Physiol 2012; 64(2): 135-141.
[21] Li H, Liu KX, Feng JL. Influence of Tanshinone Ⅱ A against cerebral ischemia on NO content and NOS in serum, the iNOS activity after reperfusion injury in rats. Chin J Chin Med Inform 2009; 16(1): 40-42.
[22] Chen XL, Wang LL, Qiao Yi, Xi MM, Wu Y, Wang JW. Influence of Shuangsen vein bolus on of ischemia-reperfusion injury in rat infarction area and the nerve cell apoptosis. J Med Fight Infection 2010; 7(3): 182-184.
[23] Wang HJ, Jia RD, Zhao R. Protection of Tanshinone Ⅱ A in intestinal ischemia reperfusion lung injury in rats. Anti-infection Pharm 2013; 10(1): 36-39.
ment heading
10.1016/S1995-7645(14)60037-7
*Corresponding author: Gong-Ning Shi, Chief Physician, Professor, Master Tutor, Huaihe River Hospital, Henan University, Kaifeng 475000, Henan, China.
Tel: 13503788880
E-mail: shignin@163.com
Foundation project: It is supported by New Medical Technology Import Project in Henan Province (No 2011020113).
Rats
Lung ischemia-reperfusion
Protection
 Asian Pacific Journal of Tropical Medicine2014年4期
Asian Pacific Journal of Tropical Medicine2014年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Establishment and identification of induced pluripotent stem cells in liver cancer patients
- Correlations of β-catenin, Ki67 and Her-2/neu with gastric cancer
- Experimental treatment of radiation pneumonitis with human umbilical cord mesenchymal stem cells
- Protection effect of Xuanfudaizhetang on reflux esophagitis in rats
- Effect of peroxisome proliferator-activated receptor gamma agonist on heart of rabbits with acute myocardial ischemia/reperfusion injury
- Effect and mechanism of salvianolic acid B on the myocardial ischemiareperfusion injury in rats
