Correlations of β-catenin, Ki67 and Her-2/neu with gastric cancer
Hong-Wen Wu, Cheng-Yong Qin, Ji-Lai Huang, Xian-Yi Kong, Wen-Ji Wang, Wen-Kun Bai
1School of Medicine, Shandong University, Jinan 250012, China
2Digestive Internal Medicine, The First Hospital of Zibo City, Zibo 255200, China
3Digestive Internal Medicine, Shandong Provincial Hospital, Jinan 250021, China
4Digestive Internal Medicine, Shandong Qianfoshan Hospital, Jinan 255200, China
Correlations of β-catenin, Ki67 and Her-2/neu with gastric cancer
Hong-Wen Wu1, Cheng-Yong Qin2*, Ji-Lai Huang3, Xian-Yi Kong3, Wen-Ji Wang4, Wen-Kun Bai4
1School of Medicine, Shandong University, Jinan 250012, China
2Digestive Internal Medicine, The First Hospital of Zibo City, Zibo 255200, China
3Digestive Internal Medicine, Shandong Provincial Hospital, Jinan 250021, China
4Digestive Internal Medicine, Shandong Qianfoshan Hospital, Jinan 255200, China
Objective: To study the clinical pathologic characteristics of β-catenin, Ki67 and Her-2/neu in gastric cancer and the correlation of β-catenin and Ki67 to the protein expression and gene conditions of Her-2/Neu. Methods: The protein expression of β-catenin, Ki67 and Her-2/Neu was detected by immunohistochemistry in 101 cases of gastric cancer and the gene conditions of Her-2/Neu by fluorescence in situ hybridization (FISH). Results: The protein expression of β-catenin, Ki67 and Her-2/Neu had close relationship with the clinical pathologic characteristics of gastric cancer. The β-catenin and Ki67 had obvious correlation to the differentiation, infiltration and lymphatic metastasis of the gastric cancer (P<0.05). The Ki67 had close relationship with the tumor-node-metastasis staging staging of gastric cancer (P<0.05). Her-2/Neu had close relationship with the differentiation and tumor-node-metastasis staging of gastric cancer (P<0.05) but had no relationship with the infiltration and lymphatic metastasis of the gastric cancer (P<0.05). The protein expression of Ki67 had significantly positive correlation to the protein expression and gene amplification conditions of Her-2/Neu (r=0.567, P<0.05 for protein; r=0.304, P<0.05 for gene). Conclusions: Combined detection of β-catenin, Ki67 and Her-2/Neu can be used as a reliable method to help the observation of biological behavior, diagnosis and prognosis of gastric cancer, and Ki67 can be used to serve the preliminary screening of Her-2/Neu gene state.
ARTICLE INFO
Article history:
Received January 2014
Received in revised form 15 February 2014
Accepted 15 March 2014
Available online 20 April 2014
Gastric cancer
β-catenin
Ki67
Her-2/neu
Immunohistochemistry
Fluorescence in situ hybridization
Tumor marker
1. Introduction
Gastric cancer, known as a malignant tumor[1], is characterized by tumor cell invasion and metastasis and is also a main cause of death[2]. Ki67 is widely used as a marker of cell proliferation and its function is closely associated with chromatin. β-catenin exhibits the roles of signal transduction and cellular adhesion in Wnt signaling pathway. Amplification ofHer-2/neugene is the key to the efficacy of molecular targeted drugs. We investigated the correlations of β-catenin, Ki67 and Her-2/neu with the clinical characteristics of gastric cancer and analyzed the relationship between the expression of β-catenin, Ki67 and Her-2/neu proteins. Reliable reference indices were also searched to screenHer-2/neugene state.
2. Materials and methods
2.1. General data
Cancerous gastric tissue samples were surgically resected from 101 gastric cancer patients who received treatment at Shandong Provincial Hospital, China between March 2012 and May 2013. Simultaneously, fresh stomach mucous membrane tissues, which was confirmed pathologically free of carcinomatous change, were harvested from thecutting edge of diseased foci of 76 gastric cancer patients and used as control. The included patients did not receive any anti-tumor treatment before surgery and provided complete clinical record document. Following hematoxylineosin staining, all tissue sections were diagnosed as adenocarcinoma by two experienced physicians in consensus. The gastric cancer patients, 52 males and 49 females, were at the age of 57 (range from 34 to 80) years. The size of tumor was ≥5 cm in 70 patients and <5 cm in 31 patients. According to the WHO criteria, tumor cells were well- and medium-differentiated in 51 patients and poorly-differentiated in 50 patients. As per the pathological tumor-node-metastasis staging (pTNM) system issued by the American Joint Commission for Cancer Staging (2011), tumors were staged as I/II in 58 patients and as III-IV in 43 patients. According to the depth of invasion, tumors invaded the serosa in 57 patients and had invaded but not penetrated the serosa in 44 patients. Lymph node metastasis was present in 68 patients but not in 33 patients.
2.2. Main instruments and reagents
The experimental instruments used in this study were provided by Department of Pathology, Shandong Provincial Hospital, China. Other instruments included paraffin embedding apparatus (Germany), microtomes (LEICA BM2135; AO, USA), optical microscope (BX-50; Olympus, Japan), constant temperature baker (Shanghai Yuejin Medical Instrument Factory, China), and in situ hybridizer (ThermoBriteTM, StatSpin, USA). Immunohistochemical reagents were purchased from Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd., China.Her-2/neugene fluorescence in situ hybridization (FISH) detection kits and reagents were purchased from Beijing Jinpujia Medical Science and Technology Co., Ltd., China.
2.3. Immunohistochemical staining assay
Immunohistochemical staining was performed using streptavidin-peroxidase kit according to the manufacturer’s instructions. PBS, rather than primary antibody, was taken as a negative control. Through an optical microscopy, β-catenin- and Ki67-positive cells were counted in five fields of view randomly selected from each section. The percentage of β-catenin- or Ki67-positive cells ≤10% was considered as 0 point, 11%-50% as 1 point, 51%-75% as 2 points, and >75% as 3 points. No staining was scored 0, light brown 1 point, brown 2 points, and dark brown 3 points. The final score was obtained by sum of the above two scores: 1-2 points were considered as “1+”, 3-4 points as “2+” and“5-6” points as “3+”. Finally, sample with a total score of 0 was considered as negative, while sample with a total score of 1+ to 3+ as positive. Her-2/neu immunoreactivity was scored according to HercepTest guidelines. Her-2/neupositive cells exhibited brown yellow staining.
2.4. FISH detection
FISH detection was performed in strict accordance with kit instruction. Thirty cells were counted for calculation of ratio value according to the formula:
Ratio = Number of red signals in 30 nuclei/Number of green signals in 30 nuclei.
Ratio <1.8 was considered negative, indicating absence ofHer-2/neugene amplification in the tested sample; Ratio >2.2 was considered positive, indicating presence ofHer-2/neugene amplification in the tested sample; 1.8≤Ratio≤2.2, count 100 cells or repeat FISH test.
2.5. Statistical analysis
Statistical analysis was performed using SPSS 17.0 software. Difference comparison was carried out using Chi-square test and Fisher’s exact test. Correlation analysis was conducted using Spearman’s rank correlation. A level ofP<0.05 was considered statistically significant.
3. Results
3.1. Expression ofβ-catenin, Ki67 and Her-2/neu proteins in cancerous gastric tissue
As shown by the immunohistochemical staining, the positive expression of β-catenin and Ki67 was located in the nuclei (Figure 1A and 1B), and that of Her/neu was found in the cellular membrane (Figure 1C). The positive cells were stained light or dark brown. The expression ofHer-2/neugene was also detected by FISH. The red signals ofHer-2/neugene amplification (positive) were distributed in clusters or diffusion spots (ratio >2.2; Figure 2A), while the signals were distributed in diffusion spots (ratio <1.8; Figure 2B) withoutHer-2/neugene amplification.
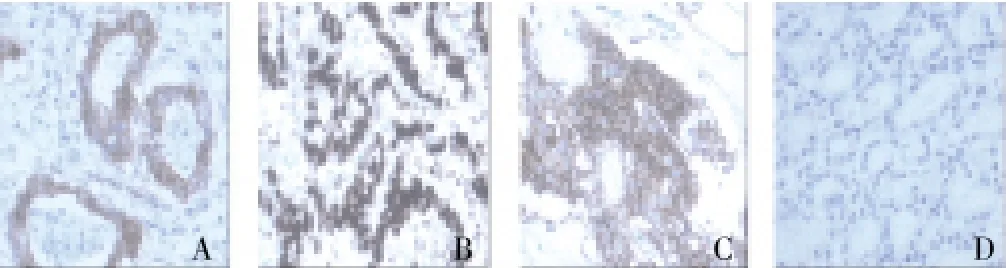
Figure 1. Expression of β-catenin, ki67 and Her-2/neu in the tested samples detected by immunohistochemistry (×200).(A) β-catenin-positive expression (3+); (B) Ki67-positive expression (3+); (C) Her-2/neu-positive expression (3+); (D) Her-2/neu-negative expression.
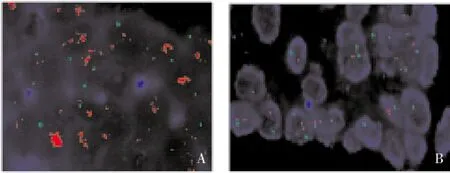
Figure 2. Amplification of Her-2/neu gene in the tested sample detected by in situ hybridization (×200).(A) With Her-2/neu gene amplification (ratio >2.2); (B) Without Her-2/neu gene amplification (ratio <1.8). Her-2/neu gene is shown by red signals and centromere 17 by green signals
Among the 101 patients with gastric cancer, the number of β-catenin-positive patients scored 0, 1+, 2+ and 3+ was 26(25.7%), 4(4%), 29(28.7%) and 42(41.6%), respectively, while the number of Ki67-positive patients was 20(19.8%), 24(23.8%), 15(14.8%) and 42(41.6%), respectively. The number of Her-2/neu-positive patients scored 2+ and 3+ was 6(6.0%) and 10(10.0%), respectively. The percentage of β-catenin-, Ki67-, and Her-2/neu-positive patients among the 101 gastric cancer patients was 74.3%(75/101), 80.2%(81/101) and 15.8%(16/101), respectively, which was significantly higher than that of the control group [36.8%(28/76), 25.0%(19/76) and 1.3%(1/76),P<0.05].
3.2. Correlations ofβ-catenin, Ki67 and Her-2/neu expression with the clinical pathological characteristics of gastric cancer
The expression of β-catenin, Ki67 and Her-2/neu was not correlated with the gender, age, and tumor size of patients with gastric cancer. The expression of β-catenin and Ki67 were significantly correlated with degree of tumor cell differentiation, depth of tumor cell invasion and lymph node metastasis (P<0.05). The β-catenin expression was not correlated with pTNM stage. The Her-2/neu expression was significantly correlated with pTNM stage (P<0.05), but it was not correlated with the depth of tumor cell invasion and lymph node metastasis (Table 1).
3.3. Correlations of Ki67 protein expression with Her-2/neu protein expression and gene stage
The Ki67 protein expression was positively correlated with Her-2/neu protein expression (r=0.567,P<0.05) and positively correlated withHer-2/neugene state (r=0.304,P<0.05). The immunohistochemistry results showed that the positive rate of Her-2/neu expression (21.4%) was significantly higher in the 9 gastric cancer patients presenting with the positive expression of Ki67 (3+) and Her-2/neu (3+) than in other types (Table 2).
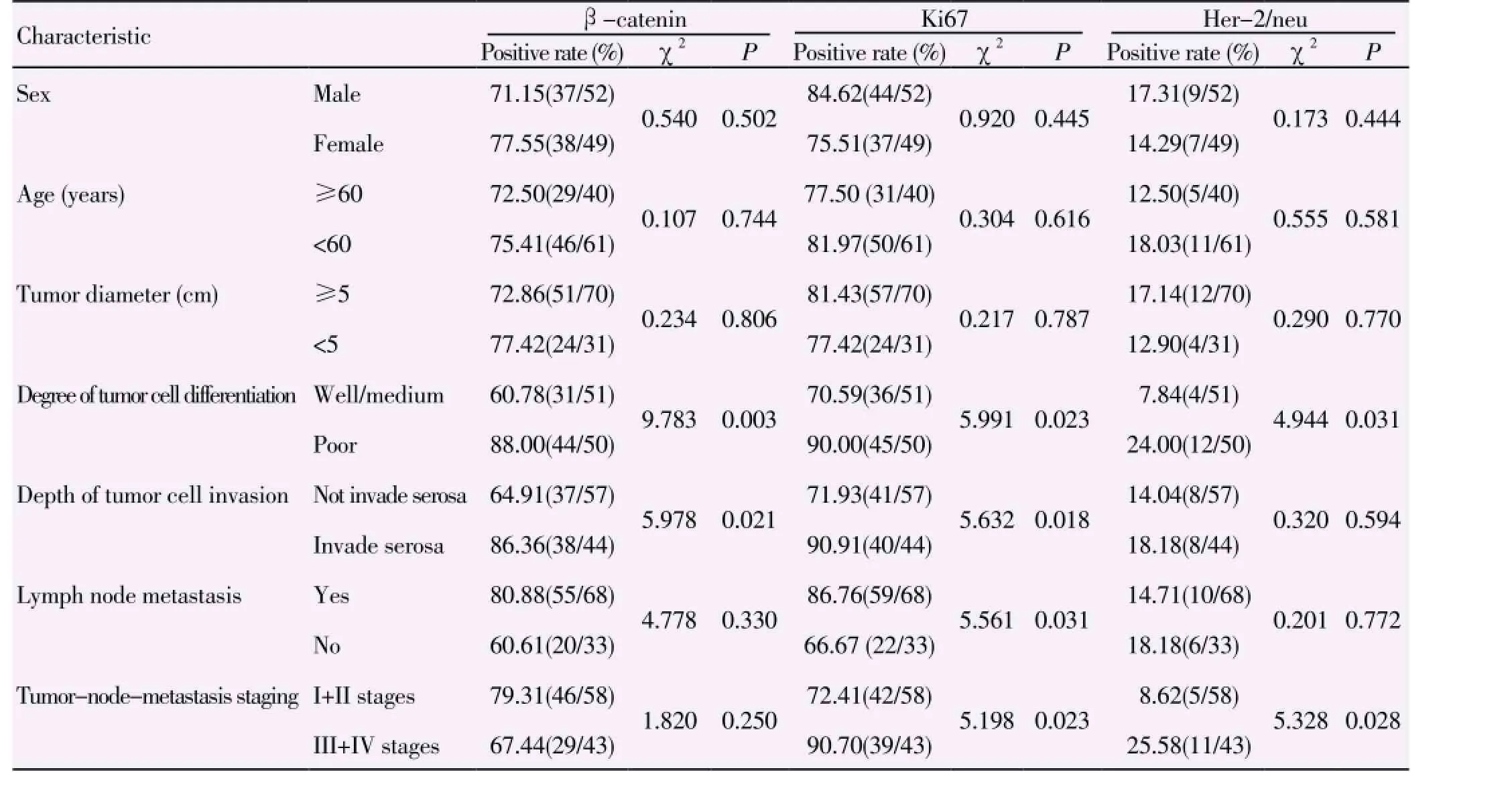
Table 1 Correlations of β-catenin, Ki67 and Her-2/neu with the clinical pathological characteristics of gastric cancer.
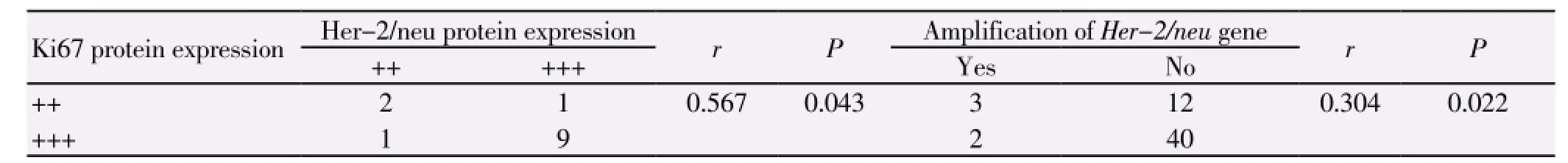
Table 2 Correlations of Ki67 protein expression with Her-2/neu protein expression and gene stage.
3.4. Analysis on Her-2/neu protein expression and Her-2/neu gene state
Through FISH, the amplification ofHer-2/neugene was detected in 14 patients, with a gene amplification rate of 13.9%(14/101). According to the Her-2/neu protein expression, the patients were divided into two groups: Her-2/neu (2+/3+) and Her-2/neu (-/+). The amplification rates ofHer-2/neugene in the sanples with Her-2/neu (3+) and Her-2/neu (2+) were 90.0%(9/10) and 83.3%(5/6), respectively. In the tested samples with Her-2/neu (-/1+), no amplification of theHer-2/neugene was detected (0/33 and 0/52, respectively). The detection results of patients with Her-2/neu (2+/3+) by immunohistochemistry was 87.5% consistent with the amplification resluts ofHer-2/neugene by FISH.
4. Discussion
Abnormal or up-regulated expression of β-catenin leads to the occurrence of diseases[3]. It has been evidenced that β-catenin influences the biological behaviors of tumor stem cells[4] and its down-regulation improves cell ultrastructure, promotes apoptosis and inhibits cell proliferation[5]. We found β-catenin was significantly correlated with degree of tumor cell differentiation, depth of tumor cell invasion and lymph node metastasis (P<0.05), suggesting that abnormal β-catenin expression in the gastric cancer tissue helps gastric cancer cells to obtain stronger invasive and metastatic abilities and thus indicates poor prognosis.
At present, Ki67 has been considered as a reliable index for evaluating cell proliferation and malignant potentials and predicting cancer recurrence[6-7], and its expression level is of important clinical significance for tumor treatment and metastasis[8]. It also shows a predictive value in adjuvant chemotherapy. In our study, the Ki67 expression rate was 70.6% in the well- and medium-differentiated gastric cancer, 90% in the poorly differentiated gastric cancer, 68.6% in the serous layer-infiltrated tissues and 90.9% in the non-infiltrated tissues. The results suggest that changes in proliferative activity of tumor cells are related to the progression of gastric cancer.
Her-2/neu, also called C-erbB-2, shows similar functions as Ki67 and both can promote mitosis. In this study, the positive expression rate of Her-2/neu was 15.8%, which is in accordance with a previous report[9]. The positive expression rate of Her-2/neu was 3.4% and 8.8% in the welland medium-differentiated tissue and poorly differentiated tissue respectively, suggesting that high expression level of Her-2/neu is a marker of malignant tumor. Moreover, the amplification rate ofHer-2/neugene increased with the increasing grades, indicating the state ofHer-2/neugene becomes more instable with increasing malignance of gastric cancer.
The application of Her-ceptin, the monoclonal antibody against Her-2/neu, in the treatment of gastric cancer attracts more attention and disputes. Trastuzumab (trade name: herceptin), a molecular targeted drug, is only effective in tumor patients presenting withHer-2/neugene amplification. Her-2/neu (2+) was previously used as the reference for FISH detection ofHer-2/Neugene, but negative FISH detection results also exist in subjects with Her-2/neu (3+). To predict theHer-2/neugene state of tumor patients more simply and accurately, we statistically analyzed the present results and found that the expression of Ki67 protein was positively correlated with the protein expression and gene amplification of Her-2/neu (r=0.567,P<0.05 for protein;r=0.304,P<0.05 for gene). TheHer-2/neugene amplification analyzed by FISH was consistent with the protein expression detected by immunohistochemistry, with a K value of 0.879, demonstrating that the protein expression and gene state had good consistency. This is in line with previous reports. However, contrary results have also been reported, which may be caused by differences in experimental methods, interpretation criteria and sample size. Further investigation is needed to eliminate this conflict.
Our results demonstrated that the protein expression and gene amplification of Her-2/neu were closely related to the expression of Ki67 protein. Previous researches show that Her-2/neu protein does not act independently but exhibits synergic and inhibitory effects together with other factors. Further studies are required to investigate whether the proliferative activity of gastric cancer cells promotes theHer-2/neugene amplification and whether there is aregulatory relationship between Ki67 and Her-2/neu. We can speculated that the Ki67 protein expression, in addition to Her-2/neu (2+) protein expression, may be selected as another assistant reference in screeningHer-2/neugene state by FISH.
Taken together, the expression of β-catenin, Ki67 and Her-2/neu is closely related to the clinical pathological characteristics of gastric cancer. Combined detection methods can provide an overall reference evidence for understanding the nature, clinical diagnosis and prognosis of tumors. Her-2/neu combined with Ki67 can be used as a predicator for screeningHer-2/neugene state by FISH, which will increase detection efficiency ofHer-2/neugene amplification.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgments
This work was funded by the Shandong Province Natural Fund Project (Y2008C114).
[1] Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59: 225-249.
[2] Hu SL, Kong XY, Cheng ZD, Sun YB, Shen G, Xu WP, et al. Promoter methylation of p16, Runx3, DAPK and CHFR genes is frequent in gastric carcinoma. Tumori 2010; 96: 726-733.
[3] Xu L, Jiang Y, Zheng J, Xie G, Li J, Shi L, et al. Aberrant expression of β-catenin and E-cadherin is correlated with poor prognosis of nasopharyngeal cancer. Hum Pathol 2013; 44: 1357-1364.
[4] Luo W, Fang W, Li S, Yao K. Aberrant expression of nuclear vimentin and related epithelial-mesenchymal transition markers in nasopharyngeal carcinoma. Int J Cancer 2012; 131: 1863-1873.
[5] Ma L, Zhang G, Miao XB, Deng XB, Wu Y, Liu Y, Jin ZR, et al. Cancer stem-like cell properties are regulated by EGFR/AKT/ β-catenin signaling and preferentially inhibited by gefitinib in nasopharyngeal carcinoma. FEBS J 2013; 280: 2027-2041.
[6] Singh S, Trevino J, Bora-Singhal N, Coppola D, Haura E, Altiok S, et al. EGFR/Src/Akt signaling modulates Sox2 expression and self-renewal of stem-like side-population cells in non-small cell lung cancer. Mol Cancer 2012; 11: 73.
[7] Ma BB, Lui VW, Poon FF, Wong SC, To KF, Wong E, et al. Preclinical activity of gefitinib in non-keratinizing nasopharyngeal carcinoma cell lines and biomarkers of response. Invest New Drugs 2010; 28: 326-333.
[8] Gaujoux S, Hantel C, Launay P, Bonnet S, Perlemoine K, Lefèvre L, et al. Silencing mutated β-catenin inhibits cell proliferation and stimulates apoptosis in the adrenocortical cancer cell line H295R. PLoS One 2013; 8: e55743.
[9] Tissier F, Cavard C, Groussin L, Perlemoine K, Fumey G, Hagneré AM, et al. Mutations of beta-catenin in adrenocortical tumors: activation of the Wnt signaling pathway is a frequent event in both benign and malignant adrenocortical tumors. Cancer Res 2005; 65: 7622-7627.
[10] Chapman A, Durand J, Ouadi L, Bourdeau I. Identification of genetic alterations of AXIN2 gene in adrenocortical tumors. J Clin Endocrinol Metab 2011; 96: E1477-1481.
[11] Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 2008; 372: 392-397.
[12] Tadjine M, Lampron A, Ouadi L, Bourdeau I. Frequent mutations of beta-catenin gene in sporadic secreting adrenocortical adenomas. Clin Endocrinol (Oxf) 2008; 68: 264-270.
[13] Wang JX, Zhang YY, Yu XM, Jin T, Pan XL. Role of centromere protein H and Ki67 in relapse-free survival of patients after primary surgery for hypopharyngeal cancer. Asian Pac J Cancer Prev 2012; 13: 821-825.
[14] He WL, Li YH, Yang DJ, Song W, Chen XL, Liu FK, et al. Combined evaluation of centromere protein H and Ki-67 as prognostic biomarker for patients with gastric carcinoma. Eur J Surg Oncol 2013; 39: 141-149.
[15] Delpech Y, Wu Y, Hess KR, Hsu L, Ayers M, Natowicz R, et al. Ki67 expression in the primary tumor predicts for clinical benefit and time to progression on first-line endocrine therapy in estrogen receptor-positive metastatic breast cancer. Breast Cancer Res Treat 2012; 135: 619-627.
[17] He WL, Li YH, Yang DJ, Song W, Chen XL, Liu FK, et al. Combined evaluation of centromere protein H and Ki-67 as prognostic biomarker for patients with gastric carcinoma. Eur J Surg Oncol 2013; 39: 141-149.
[18] Meza-Junco J, Sawyer MB. Metastatic gastric cancer - focus on targeted therapies. Biologics 2012; 6: 137-146.
[19] Meza-Junco J, Au HJ, Sawyer MB. Trastuzumab for gastric cancer. Expert Opin Biol Ther 2009; 9: 1543-1551.
ment heading
10.1016/S1995-7645(14)60033-X
*Corresponding author: Dr. Cheng-Yong Qin, professor, Digestive Internal Medicine, Shandong Provincial Hospital, Jinan 250021, China.
Tel: +86-531-87068126
E-mail: hongwenwu70@126.com
Foundation project: This work was funded by the Shandong Province Natural Fund Project (Y2008C114).
 Asian Pacific Journal of Tropical Medicine2014年4期
Asian Pacific Journal of Tropical Medicine2014年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Establishment and identification of induced pluripotent stem cells in liver cancer patients
- Experimental treatment of radiation pneumonitis with human umbilical cord mesenchymal stem cells
- Protection effect of Xuanfudaizhetang on reflux esophagitis in rats
- Effect of peroxisome proliferator-activated receptor gamma agonist on heart of rabbits with acute myocardial ischemia/reperfusion injury
- Effect of sevoflurane on tissue permeability of lung ischemia-reperfusion injury in rats
- Effect and mechanism of salvianolic acid B on the myocardial ischemiareperfusion injury in rats
