Protection effect of Xuanfudaizhetang on reflux esophagitis in rats
Bing Liang, Zhong-Hua Liu, Hai-Tao Wei, Zhi Zhang, Gong-Ning Shi*
1Department of Cardiothoracic Surgery, Huahe Hospital, Henan University, Kaifeng 475000, Henan, China
2Medical College, Henan University, Kaifeng 475000, Henan, China
Protection effect of Xuanfudaizhetang on reflux esophagitis in rats
Bing Liang1, Zhong-Hua Liu2, Hai-Tao Wei1, Zhi Zhang1, Gong-Ning Shi1*
1Department of Cardiothoracic Surgery, Huahe Hospital, Henan University, Kaifeng 475000, Henan, China
2Medical College, Henan University, Kaifeng 475000, Henan, China
Objective: To study protection effect of Xuanfudaizhetang on reflux esophagitis in rats.
Methods: A total of 50 Wistar rats were randomly divided into groups A, B, C, D and E with 10 in each. Reflux esophagitis model in rats was established by incomplete helicobacter seam+lower esophagus sphincterotomy. All rats were divided into 5 groups: group A as control group, group B as model group, group C with saline lavage treatment, group D with motilium treatment, group E with Xuanfudaizhetang lavage treatment. Recovery of esophageal, gastric mucosa and pH changes of rats were compared between groups. Results: Weight gain in group D and E was significantly higher in than group C; the esophageal mucosa grades and esophagus tissue pathological morphology grades of group D and E were higher than that of group B and C with significant difference between groups (P<0.05); pH of lower esophageal mucosa in group D and E increased significantly than that in the group B and C (P<0.05), and the distal mucosal pH dropped significantly in the group B and C (P<0.05). Conclusions: Xuanfudaizhetang can obviously improve the pH of lower esophageal mucosa in rats with reflux esophagitis, decrease pH value of gastric mucosal, thus improve esophageal mucosa pathological conditions to achieve therapeutic effect on reflux esophagitis.
ARTICLE INFO
Article history:
Received 10 September 2013
Received in revised form 15 October 2013
Accepted 15 December 2013
Available online 20 April 2014
Xuanfudaizhetang
Reflux esophagitis
Esophageal mucosa
PH value
Treatment
1. Introduction
Reflux esophagitis is a clinical common disease, with the rising trend of incidence year by year, along with the life and diet structure change[1-5]. The reason for this chronic intractable disease is that lower esophageal sphincter dysfunction results in reflux of gastric or duodenal contents into the esophagus, causing inflammatory lesions of esophageal mucosa, may induce serious complications such as esophageal stenosis and bleeding[6,7]. Experiments showed that, damage and symptoms of esophageal mucosa are closely related to the frequency and contact time of acid exposure, with pH dependence[8]. The author aimed to observe the protective effect of Xuanfudaizhetang on reflux esophagitis, esophageal mucosal and the effect on pH value, by selecting Wistar rats to establish reflux esophagitis model with Xuanfudaizhetang treatment. Then the curative effect on esophageal and gastric mucosa and pH value change were observed and reported as follows.
2. Materials and methods
2.1. Experimental animal
A total of 50 male, clean Wistar rats were selected, and they were provided by the Laboratory Animal Center, Class Ⅱ, weighting (251.3±42.5) g. They were free to forage and drinking. Experimental process of rats was strictly in accordance with ”Regulations on Administration of Experimental Animals”.
2.2. Instruments and reagents
DigitrapperTMMk Ⅲ pH Value Recorder (Synectics); Ray magnetic PHS-3 c precision pH meter (Shanghai precision scientific instrument co., LTD). motilium (yeung sum pharmaceutical co., LTD., production); Saline solution (pH = 7.01); ChanJing blue mixed suspension (tianjin toyo ink co.; Xuanfudaizhetang formula: inula spend 9 g, ginger 10 g, 12 g, jujube, ginseng 6 g, red ochre 30 g, pinellia 9 g, licorice root 6 g, pan-fried for crude drug concentration of 1 g/mL water decoction.
2.3. Model establishment
Reflux esophagitis model in rats was established by incomplete helicobacter seam+lower esophagus sphincterotomy after starvation for 24 h[9]. After intraperitoneal injection of urethane anesthesia and abdominal midline incision, the stomach was pierced with metal needle through the gastric body, from the pylorus to the duodenum. Pylorus seam was kept, then metal stitches was taken out. Stomach puncture point was stitched. It was incised longitudinally in 0.5 cm under the esophageal sphincter to the mucosa for strengthening the gastric reflux. All experimental animals were provided with food 24 h after surgery.
2.4. Methods
A total of 50 Wistar rats were randomly divided into A, B, C, D, E groups with 10 in each. After modelling, the rats in sham-operated Group A were only given laparotomy; Group B is the model group without special treatment; Group C was treated with saline lavage; Group D was treated with motilium (2 mL/d) for a week; Group E was treated with Xuanfudaizhetang lavage 2 mL once a day for a week after 48 h.
2.5. Indexes observation
The growth situation and weight changes during treatment were observed. One week later, recovery of esophageal, gastric mucosa and pH changes of rats were compared between groups. After anesthesia and caesarean section, a pH recorder electrode was inserted into the stomach big bend about 1 cm above the stomach esophagus-junction to record the pH; then pH electrode was rinsed with distilled water and it was inserted through the distal big bend perforation to record the pH. After sacrificing, the lower segment of esophagus was collected after saline flushing for macroscopic inspection of RE classification, according to the Chinese Medical Association Digestive Endoscopy Diagnostic Criteria about RE[10]. 1 cm of esophagus at 0.5 cm above the stomach-esophagus border was collected to prepare HE dyeing for pathological RE grading.
2.6. Statistical analysis
SPSS12.0 statistics software was used for processing data in this study; data were expressed as (mean±sd), and analyzed byttest. P<0.05 was considered as statistically significant difference.
3. Results
3.1. General condition
Group A revealed luster hair, good appetite and granule stool; Group B revealed lacklustre, less appetite abdominal distension. General situation of D, E groups of rats was close to group A after treatment, body weight was increased with the increase of appetite, with weight growth rate of as (22.14±3.89) g in group E, (11.91±3.13) g in group D, (13.97± 1.87) g in group C, the difference between three groups was statistically significant (P<0.05).
3.2. Pathological morphology changes
Group A showed complete, smooth and white. The esophageal mucosa grades and esophagus tissue pathological morphology grades of group D and E were higher than that of group B and C with significant difference between groups (P<0.05); grades of group D and E shows no significant difference between each other. Esophageal mucosa of rats in group A had no obvious abnormality of HE staining (Table 1).
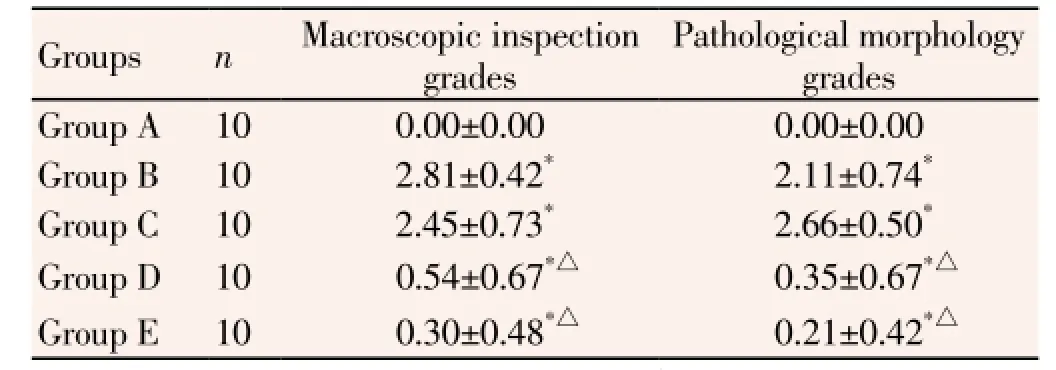
Table 1 Esophageal mucosa grades and pathological morphology grades of esophagus tissue in the RE rats.
3.3. pH comparision of lower esophageal mucosa and the distal mucosa
There was no significant difference in pH between group D and E (P>0.05); pH of lower esophageal mucosa in groupD and E was increased significantly than that in the group B and C (P<0.05), and the distal mucosal pH dropped significantly in the group B and C (P<0.05) (Table 2).
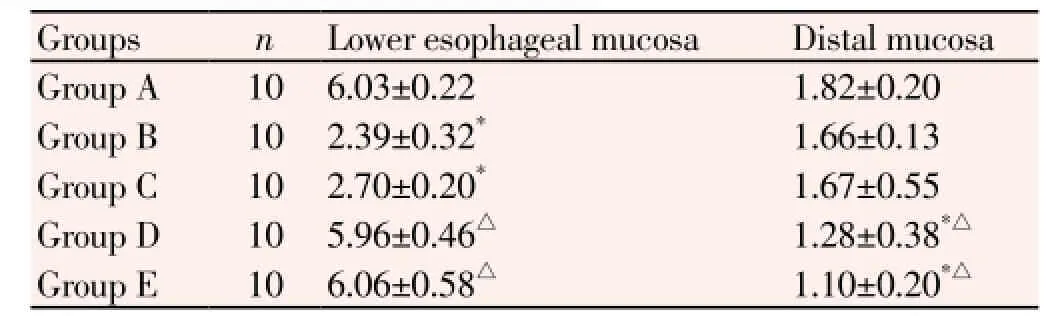
Table 2 pH comparision of lower esophageal mucosa and the distal mucosa.
3.4. Pathological observations of esophageal mucosa
Esophageal mucosa of group A, D, E was normal; hyperplasia of squamous esophageal mucosa was significant in Group B and C. Propria nipples was observed in mucosa lamina, inflammatory cells infiltrating, predominantly neutrophils and lymphocytes, was observed (Figure 1).
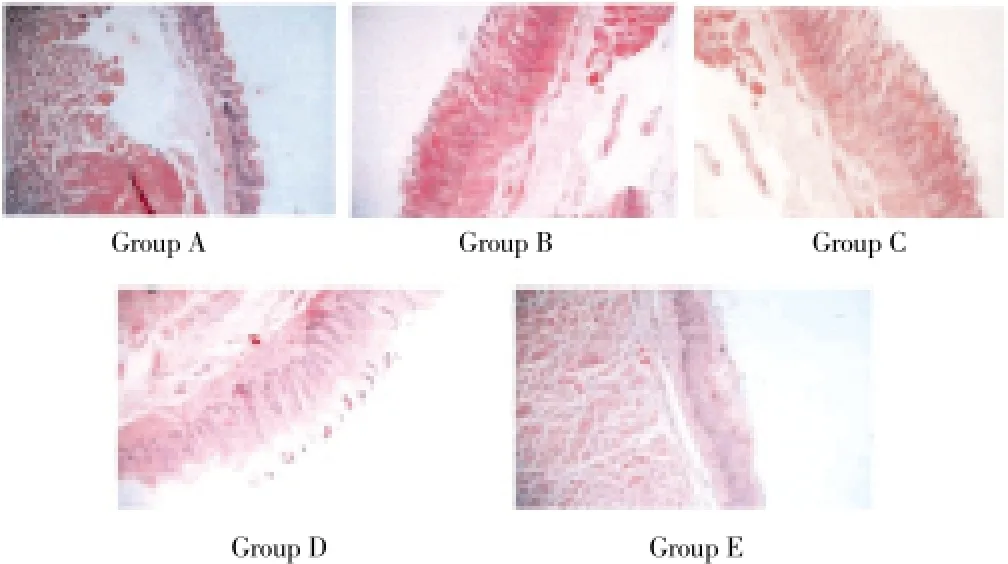
Figure 1. Pathological observations of esophageal mucosa (HE×100).
4. Discussion
The reflux esophagitis belongs to “noisy, spit acid, choking diaphragmatic” category in Chinese traditional medicine, related to many factors such as diet and mood. The pathogenesis is that the gastric estrangement and liver-qi stasis, resulting in liver-qi depression, dampness and heat cements in the liver[11-15]. Acid reflux can cause burning pain of diaphragm, which would progress into choke symptoms[16,17]. In view of the fact that this disease is mainly caused by spleen deficient, weak stomach, obstructed phlegm, etc. So based on the theory of Chinese medicine that digestive organs should have harmonious relationship[18], we chose Xuanfudaizhetang to treat rats with reflux esophagitis, and obtained good effect.
Inula flower can cause gas saliva inversion and sputum elimination. The official medicine red ocher can treat hiccups and belching, the adjuvant medicine ginger can warm the stomach phlegm, pinellia can inverse the stomach. Combination use of these ingredients can decrease the acid damage[19-24]. Modern pharmacology showed that Xuanfudaizhetang can obviously enhance the gastrointestinal peristalsis, and increase a variety of amino acids and strong tonic, provide the body with sufficient nutritions to promote recovery of vital spirit[25-29]. In this study, after treatment, the weight gain of group E was significantly higher than that of group C, which was provided with saline (P<0.05), and its mechanism of action and the theory is the same. Research has shown that esophageal mucosa injury and symptoms in reflux esophagitis are pH dependent, frequency and contact time with acid exposure is also closely related to reflux esophagitis. Acid reflux can cause the direct damage in reflux esophagitis when esophageal pH is less than 4, play an important role in the pathogenesis of reflux esophagitis[30-32]. In this experiment, lower esophageal pH in group E rats is significantly higher than group C (model group) and group B (placebo), suggesting that Xuanfudaizhetang can obviously improve the pH of lower esophageal mucosa in rats with reflux esophagitis, decrease pH value of gastric mucosal, thus improve reflux esophagitis pathological state. Xuanfudaizhetang and motilium can improve pH value of lower esophageal mucosal, which may be related to promoting anterograde peristalsis of oesophagus and stomach, as well as inhibition of gastric acid secretion and so on[33,34].
The experimental results showed that compared with group B and C, pH of lower esophageal mucosa of rats of group D increased significantly after treatment for a week. It suggests that Xuanfudaizhetang can increase the pH value of the lower esophageal mucosa and reduce inflammation stimulation, so as to protect the esophageal mucosa, it can also significantly stimulate the secretion of gastrin and gastric acid, reduce gastric pH value to improve pathological condition of esophageal mucosa in reflux esophagitis treatment.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Wang SF, Shun SD. The curative effect observation and mechanism of Esomeprazole in treatment of reflux esophagitis. Modern Digestion & Intervention 2010; 15(2): 113-115.
[2] Wang TL. Review: classification and pathogenesis ofgastroesophageal reflux disease. Trad Chin Med Res 2009; 22(4): 45-46.
[3] Zheng HG, Shi YP, Li XL. 60 cases were down-regulated in the treatment of functional dyspepsia. Global Chin Med 2012; 5(8): 621-622
[4] Xing J, Feng QQ, Li CN, Fan T. Combination of traditional Chinese and western medicine in treatment of reflux esophagitisclinical observation. Chin Med Herald 2013; 10(1): 120-121
[5] He M. Nanyang clinical epidemiological studies of reflux esophagitis. Appl J General Prac 2012; 14(1): 7-8.
[6] Qing Z, Zhang BJ, Wang SJ. Clinical epidemiological studies of reflux esophagitis . The Chin Comm Physicians (Med) 2011; 19(30): 125-126.
[7] Du Y, Bai RX, Fang L, Yao SK. Small doses of Esomeprazole in preventing reflux esophagitis, the role of cured after recurrence. Chin J New Drugs 2010; 19(19): 1785-1787.
[8] Yuan GX, Ma Y, Han SP, Wei AQ, Pan M, Xu JJ, et al. effect of xuanfudaizhetang on CyclinD1 expression in mixed rats model with reflux esophagitis. Tianjin Trad Chin Med 2010; 27(1): 50-52.
[9] Kang LW, Xiong NY, Li SY, Xiao HZ. Fe-(2+), Fe-(3+) content of different fried liquid from ochre. Experimental Technol Manag 2011; (3): 36-38, 44.
[10] Ning YC, Wang ZG, Wu JM, Liu JJ, Ji F, Liu DK, et al. Gastroesophageal reflux disease diagnosis and treatment of 1014 cases of hospitalized patients. Chin General Proc Mag (E) 2010; 4(3): 264-270.
[11] Ye B, Ye W. Rise and fall of traditional Chinese medicine theory in the application of the reflux esophagitis and its complications. Chin Basic Med J Trad Chin Med 2012; 18(3): 292-293.
[12] Guo Y. Syndrome differentiation in treatment of reflux esophagitis, 100 cases of clinical curative effect observation. Bei Fang Yao Xue 2012; 9(7): 57-58.
[13] Shen YL. Banxia decoction soup in treatment of reflux esophagitis curative effect observation. J Liaoning Univ Trad Chin Med 2012; 14(8): 180-181.
[14] Zhu ZZ, Hao JJ, Lv J. Banxiaxiexin decoction and Xuanfudaizhe decoction in treatment of reflux esophagitis, 120 cases of clinical observation. Res Integr Trad Chin Western Med 2012; 4(4): 184-185, 187.
[15] Chen J, Dan Z. Xiaoyao powder in treatment of reflux esophagitis, random parallel control study. J Pract Trad Chin Int Med 2012; 26(2): 41-42.
[16] Duan SS, Zhao Y, Yan XG. From the carbuncle treatment of reflux esophagitis, theoretical basis and clinical practice. Chin Comm Physicians (Med) 2011; 12(34): 169-170.
[17] Wang XH, Wang D, Wei PK. Rev diaphragmatic adjustment of the treatment of 32 cases of erosive reflux disease. Chin J Chin Med Inform 2010; 17(2): 63-64.
[18] Hu YL, Shen SW. Stomach Yin qing tonga subtraction in treatment of reflux esophagitis, 45 cases. Mod Trad Chin Med 2011; 31(2): 17-18.
[19] Chen CH. Curative effect observation of Zinitongrun Embellish drop soup in treatment of reflux esophagitis. Guangming J Chin Med 2012; 27(3): 478-480.
[20] Zhu LJ, Hong X. Syndrome differentiation in treatment of reflux esophagitis, 106 cases of clinical curative effect observation. Jiangxi Trad Chin Med 2010; (6): 32-33.
[21] Cui XF. Stomach pixu (spleen deficient) weak type reflux esophagitis, 62 cases traditional Chinese medicine treatment. Clinical J Chin Med 2012; 43(9): 81-83.
[22] Zhang YM. Syndrome differentiation in treatment of reflux esophagitis, 66 cases of clinical curative effect observation. Chin Med Herald 2012; 9(14): 114-115.
[23] Shang YF. Syndrome differentiation in treatment of reflux esophagitis, 34 cases. Heilongjiang Chin Med 2009; 38(2): 32.
[24] Hu KM. relationship between reflux esophagitis and internal organs. Zhejiang J Integrated Trad Chin Western Med 2009; 19(6): 350-351.
[25] Huang MH, Chen XR. Liver spleen and stomach drop decoction combined with Esomeprazole and Mosapride in treatment of reflux esophagitis, 48 cases. Chin J Integrated Trad Chin Western Med Dig 2009; 17(04): 268-269.
[26] He G, Luo RX. Combination of traditional Chinese and western medicine in treatment of reflux esophagitis, 60 cases of clinical observation. Pract J Ttrad Chin Med 2012; 28(3): 192.
[27] He QQ, Fu XG, He Q. Combination of traditional Chinese and western medicine in treatment of reflux esophagitis, 60 cases of clinical observation. J Sichuan Trad Chin Med 2010; 28(8): 68-69.
[28] Gong SQ. Combination of traditional Chinese and western medicine in treatment of reflux esophagitis, 60 cases of clinical observation. Pract Clin J Integrated Trad Chin Western Med 2010; 10(5): 51-52.
[29] Zhang Y, Qu R, Zhu JL, Yang K. Artemisia Qin qing bile tonga subtraction and rabeprazole azole in treatment of reflux esophagitis, 89 cases of clinical observation. J Shanxi Coll Trad Chin Med 2012; 10(03): 73-74.
[30] He WM, Hu XL. Curative effect observation of 30 cases-Herba schizonepetae forsythia tonga subtraction treatment of reflux esophagitis. Chin Comm Physicians (Med) 2012; 13(15): 255-256.
[31] Du X, Shi YQ, Qiu JR, Yuan HX. Yuan Gongxia’s experience in treatment of reflux esophagitis-86 cases. Liaoning J Trad Chin Med 2011; 38(1): 111-112.
[32] Li XH, Li HW, Li M. Professor Xie Jingri’s experience in treatment of reflux esophagitis. J Emergency Trad Chin Med 2010; 19(8): 1345.
[33] Zhu HY, Jin XJ. Wentonghewei method in treatment of reflux esophagitis. J Changchun Univ Trad Chin Med 2011; 27(2): 208-209.
[34] Li X, Xie LS. Experience of Professor Yuan Changjin in treating reflux esophagitis by lifting liver and clearing stomach. Guiding J Trad Chin Med Pharmaco 2010; 7(5): 20-21.
ment heading
10.1016/S1995-7645(14)60035-3
*Corresponding author: Gong-Ning Shi, Chief Physician, Master Tutor, Department of Cardiothoracic Surgery, Huahe Hospital, Henan University, Kaifeng 475000, Henan, China.
Tel: 13503788880
E-Mail: liangbintg@163.com
Foundation project: It is supported by Project of Education Department in Henan Province, No: 12A320004.
 Asian Pacific Journal of Tropical Medicine2014年4期
Asian Pacific Journal of Tropical Medicine2014年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Establishment and identification of induced pluripotent stem cells in liver cancer patients
- Correlations of β-catenin, Ki67 and Her-2/neu with gastric cancer
- Experimental treatment of radiation pneumonitis with human umbilical cord mesenchymal stem cells
- Effect of peroxisome proliferator-activated receptor gamma agonist on heart of rabbits with acute myocardial ischemia/reperfusion injury
- Effect of sevoflurane on tissue permeability of lung ischemia-reperfusion injury in rats
- Effect and mechanism of salvianolic acid B on the myocardial ischemiareperfusion injury in rats
