MH-STRALP: A scoring system for prognostication in patients with upper gastrointestinal bleeding
Jun-Nan Hu,Fei Xu,Ya-Rong Hao,Chun-Yan Sun,Kai-Ming Wu,Yong Lin,Lan Zhong,Xin Zeng
Abstract BACKGROUND Upper gastrointestinal bleeding (UGIB) is a common medical emergency and early assessment of its outcomes is vital for treatment decisions.AIM To develop a new scoring system to predict its prognosis.METHODS In this retrospective study,692 patients with UGIB were enrolled from two centers and divided into a training (n=591) and a validation cohort (n=101).The clinical data were collected to develop new prognostic prediction models.The endpoint was compound outcome defined as (1) demand for emergency surgery or vascular intervention,(2) being transferred to the intensive care unit,or (3) death during hos-pitalization.The models’ predictive ability was compared with previously esta-blished scores by receiver operating characteristic (ROC) curves.RESULTS Totally 22.2% (131/591) patients in the training cohort and 22.8% (23/101) in the validation cohort presented poor outcomes.Based on the stepwise-forward Logistic regression analysis,eight predictors were integrated to determine a new post-endoscopic prognostic scoring system (MH-STRALP);a nomogram was determined to present the model.Compared with the previous scores (GBS,Rockall,ABC,AIMS65,and PNED score),MH-STRALP showed the best prognostic prediction ability with area under the ROC curves (AUROCs) of 0.899 and 0.826 in the training and validation cohorts,respectively.According to the calibration curve,decision curve analysis,and internal cross-validation,the nomogram showed good calibration ability and net clinical benefit in both cohorts.After removing the endoscopic indicators,the pre-endoscopic model (pre-MH-STRALP score) was conducted.Similarly,the pre-MHSTRALP score showed better predictive value (AUROCs of 0.868 and 0.767 in the training and validation cohorts,respectively) than the other pre-endoscopic scores.CONCLUSION The MH-STRALP score and pre-MH-STRALP score are simple,convenient,and accurate tools for prognosis prediction of UGIB,and may be applied for early decision on its management strategies.
Key Words: Upper gastrointestinal bleeding;Prognosis prediction;Retrospective study;Nomogram;Post-endoscopic model;Pre-endoscopic model
lNTRODUCTlON
Upper gastrointestinal bleeding (UGIB) is a type of bleeding that originates above the Treitz ligament and always results from an esophageal,gastroduodenal,and biliary or pancreatic disease involving the duodenum[1].According to the cause of bleeding,it is divided into two categories: Nonvariceal UGIB (NVUGIB) and variceal UGIB (VUGIB).The common causes of NVUGIB include peptic ulcer,acute and chronic inflammation of the upper gastrointestinal mucosa,and malignancy;bleeding induced by peptic ulcer still ranks first.Due to the aging population and the increased use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and other anti-platelet drugs,the incidence of NVUGIB derived from upper gastrointestinal carcinomas (UGIC) and acute gastric mucosa lesions presents an increasing trend[2,3].Moreover,as the chief etiology of VUGIB,esophageal-gastric variceal bleeding (EGVB) is a serious and common complication of portal hypertension in patients with liver cirrhosis,associated with a 20% risk for mortality at 6 wk after onset[4].
As we all know,the greatest risk of UGIB is to lead to life-threatening peripheral circulatory failure.Although the global mortality associated with UGIB seemed on a downward trend with the development of endoscopic techniques,the extensive use of PPIs,and the improvement of specialty care,the morbidity and mortality during hospitalization showed no significant change in 2012-2013 compared to 10 years ago in China;the 30-day mortality still reaches up to 11%[3,5-8].Thus,UGIB remains as a medical emergency in clinical practice,leading to significant morbidity and mortality,hospitalization rates,and healthcare costs[5].
It has been well documented that a precise risk assessment is crucial to aid clinical decision-making and guide subsequent treatment,such as determining the timing of endoscopy,time to discharge,and level of care in patients with UGIB[9-12].Therefore,multinational guidelines and consensus consistently recommended the application of clinically validated prognostic scoring systems in evaluating the severity of UGIB and the need for clinical intervention.To date,several scoring systems were developed for prognosticating UGIB and have proven to be advantageous in different studies (i.e.,GBS,Rockall,ABC,AIMS65,and PNED scores);these were divided into scores for NVUGIB and VUGIB patients based on the etiology.Considering the fact that endoscopic performances are of great significance in predicting the outcomes of bleeding,yet not totally eligible for all patients,the scoring systems for UGIB are categorized into scores with or without endoscopic variables[13-17].However,these scores have been erratically applied in clinical practice;their use in clinical decisions remains limited[18-21].Additionally,the primary outcome variables were inconsistent for the construction of scoring systems,including the risk of complications,rebleeding,the need for clinical intervention,or death.Despite the advantages previously reported,most prognostic scoring systems of UGIB were not validated in trials;thus,previous scoring systems for UGIB prognostication remain unclear in China.Therefore,it is necessary to establish an appropriate risk stratification system based on the composite outcomes for Chinese UGIB patients.
With this study,we aimed to investigate the main factors influencing the poor outcomes of UGIB (e.g.,the demand for emergency surgery or vascular intervention,being transferred to the intensive care unit (ICU),and dying during hospitalization) and attem-pted to identify a simplified and practical prognostic scoring system for UGIB risk stratification and for guiding its treat-ment decisions.
MATERlALS AND METHODS
Study population
This is a multicenter,retrospective,cohort study.All procedures were performed in accordance with the ethical standards of the Responsible Committee on Human Experimentation (institutional and national) and the 1975 Helsinki Declaration,as revised in 2008.The study protocol was reviewed and approved by the Institutional Ethics Committee of Shanghai Changzheng Hospital (2016SL018).
To determine the impact factors of the outcomes of UGIB and to develop the prognostic scoring system,UGIB patients admitted in East Hospital from March 1,2020 to August 31,2021 were enrolled into a training cohort;patients admitted in Changzheng hospital from December 1,2021 to October 31,2022 were enrolled into a validation cohort.The eligibility criteria were as follows: (1) Diagnosis of UGIB by gastrointestinal endoscopy,capsule endoscopy,or enteroscopy;(2) with a clear etiology of UGIB at discharge;and (3) with sufficient clinical information,including medical history,clinical manifestations,physical signs,endoscopic findings,and laboratory examination results.The exclusion criteria were as follows: (1) Unexplained bleeding (e.g.,the location or cause could not be identified even if endoscopy and various examinations were performed);(2) those who were discharged automatically due to uncooperative treatment;(3) those who did not receive endoscopy examination during hospitalization;and (4) with insufficient clinical data.A flow chart of the screening process was shown in Figure 1.

Figure 1 Cohorts for the study. UGIB: Upper gastrointestinal bleeding;ICU: Intensive care unit.
Study design and process
In this retrospective study,the data of the individuals in the training cohort were used to select the major predictors for poor outcomes and to construct a new post-endoscopic prognostic scoring model involving endoscopic signs.Sequentially,a nomogram was determined to present the model and was compared with the previous prognostic scoring systems (i.e.,GBS,Rockall,ABC,AIMS65,and PNED scores).The value of the nomogram for UGIB prognostication was verified in the validation cohort.After removing the endoscopic predictors,the pre-endoscopic model (pre-MH-STRALP score) was conducted and compared with other pre-endoscopic scores in both training and validation cohorts.
Data collection
The clinical data were collected using a database conducted by Epidata 3.1,including medical history,symptoms,vital and other physical signs,initial laboratory findings after admission,endoscopic characteristics [e.g.,dark spots,active bleeding,adherent thrombosis,visible vessels,lesions with diameter ≥ 2 cm,stigmata of recent hemorrhage (SRH)],main treatment strategies (e.g.,the use of proton pump inhibitor,somatostatin and its analogs,blood transfusion,endoscopic management,vascular intervention,and emergency surgery) and the outcomes.
Endpoints
The primary endpoint was the compound outcomes,defined as (1) the demand for emergency surgery or vascular intervention;(2) being transferred to the ICU;or (3) death during hospitalization.According to the Guidelines of the Chinese Society of Critical Care Medicine and the standardized operating procedures of the two hospitals,the indications for transferring to ICU were the occurrence of acute,reversible,life-threatening organ dysfunction,or acute exacerbation and life-threatening manifestations based on chronic organ dysfunction.Death events were defined as all-cause mortality events.
Statistical analysis
Categorical variables were expressed as numbers and percentages or frequencies.Continuous parameters were described using medians with interquartile ranges.Theχ2test or Fisher’s exact test was used to compare the categorical variables.The comparison of continuous variables was determined by thet-test or Mann-WhitneyU-test,depending on whether these variables were from a normally distributed aggregate and were consistent with the homogeneity of variance.Univariate Logistic regression analysis was used to select variables which were associated with poor outcomes.The variables with aPvalue < 0.05 were included in the subsequent multivariate analysis.Then,a stepwise-forward Logistic regression analysis was performed to determine the major predictors and to conduct the final UGIB prognostic prediction model.According to the degree of influence of predictors (i.e.,the magnitude of the regression coefficients),a nomogram was drawn by assigning the corresponding scores to these predictive factors.The models’ predictive ability was compared with previously established scores by receiver operating characteristic (ROC) curves[22].Concordance index and decision curve analysis (DCA) were used to evaluate the clinical benefits and utility of the nomogram.Calibration plots were used to evaluate calibrating ability.All statistical analyses were performed using STATA 16 statistical software (Stata Corporation;College Station,TX,United States) and R software version 4.2.1 (R Foundation for Statistical Computing,Vienna,Austria).APvalue < 0.05 was considered statistically significant.The statistical methods of this study were reviewed by Yi-bin Guo from Department of Health Statistics,Naval Medical University,Shanghai,China.
Role of the funding source
All authors had access to the study data and reviewed and approved the final manuscript.The corresponding authors made the final decision to submit the manuscript for publication.
RESULTS
Patient characteristics
Patients with UGIB admitted in two centers were enrolled in this study.All patients had a clear UGIB etiology at discharge and underwent gastroscopy during hospitalization.Ultimately,591 patients were eventually included into the training cohort,while 101 patients were enrolled into the external validation cohort (Figure 1).Of the 591 individuals (453 males and 138 females) in the training cohort,501 (82.9%) suffered from NVUGIB,whereas 101 (17.1%) suffered from VUGIB.The main etiology of NVUGIB were peptic ulcer (379/591,64.1%) and UGIC (52/591,8.8%);the cause of VUGIB included EGVB (90/591,15.2%),Dieulafoy’s disease (8/591,1.4%),and endoscopic operations (3/591,0.5%).Among these patients,131 (22.2%) had poor prognosis (PP),including 22 deaths.Among the 109 cases transferred to the ICU,16 underwent emergency surgery and 19 received vascular intervention.In the validation cohort (78 males and 23 females),86 (85.1%) cases were diagnosed as NVUGIB,while 15 (14.9%) were diagnosed as VUGIB.The first two causes of bleeding were peptic ulcer (67/101,66.3%) and acute erosive hemorrhagic gastritis (13/101,12.9%).The proportion of the patients with PP was 22.8% (23/101);the mortality was 1.0% (1/101) in the validation cohort.The detailed characteristics of the patients in both cohorts are listed in Table 1 and Supplementary Table 1.

Table 1 Characteristics of the patients in the training cohort
Comparison of the characteristics of patients with various prognoses
According to the previously identified compound outcomes,the patients were divided into a PP and a good prognosis (GP) group.In the training cohort,compared with those in the GP group,the PP patients were older (P=0.020) and hadlower body weight (P=0.006) and body mass index (BMI,P=0.008).Totally,36.6% of patients in the PP group had previous episodes of UGIB,which was significantly higher than that in the GP group (27.2%,P=0.036).The patients in the PP group had more comorbidities and more serious complications,manifested as higher prevalence of chronic liver disease (32.8%vs15.4%,P< 0.001),liver cirrhosis (33.6%vs10.4%,P< 0.001),cerebral infarction (19.1%vs10.0%,P=0.005),stroke (19.8%vs10.9%,P=0.007),UGIC (32.1%vs10.7%,P< 0.001),liver failure (35.9%vs10.0%,P< 0.001),respiratory failure (1.5%vs0.0%,P=0.049),and multi-organ failure (7.6%vs1.7%,P< 0.001).There was no obvious difference in the administration of antiplatelet drugs (21.4%vs23.3%,P=0.641),anticoagulants (2.3%vs1.1%,P=0.533),glucocorticoids (0%vs0.9%,P=1.000),and NSAIDS (3.1%vs1.1%,P=0.224) before bleeding or previous surgery (0%vs0.9%,P=0.581) and endoscopic operation history (11.5%vs6.5%,P=0.061) between the two groups.Those patients who spent a longer time from symptom onset to admission were more likely to have poorer outcomes (P=0.033).As expected,the patients with PP had a higher probability of hematemesis (68.7%vs40.0%,P< 0.001),palpitations (67.9%vs41.7%,P< 0.001),amaurosis (15.3%vs8.7%,P=0.028),hidrosis (33.6%vs20.4%,P=0.002),and anemia (75.6%vs43.7%,P< 0.001) than those with GP,Moreover,there were significantly lower levels of systolic blood pressure (SBP,P=0.011),diastolic blood pressure (DBP,P< 0.001) red blood cell (RBC) count (P< 0.001),hemoglobin (P< 0.001),platelet (PLT) count (P< 0.001),mean corpuscular volume (MCV,P=0.012),hematocrit (HCT,P< 0.001),albumin (P< 0.001),creatinine (P=0.040),and serum iron (P=0.030),and longer prothrombin time (PT) and international normalized ratio among the patients in the PP group as compared to those in the GP group.These findings,including symptoms,body signs,and laboratory indicators,all suggested obvious clinical manifestations and severe hypoperfusion in the PP group.Moreover,the patients with poorer outcomes had a higher prevalence of rebleeding (19.8%vs3.3%,P< 0.001) and a more pressing demand for proactive intervention,manifesting as earlier timing for endoscopic examination (P< 0.001),a higher proportion of patients receiving administration of somatostatin and its analogs (92.4%vs71.3%,P< 0.001),blood transfusion (70.1%vs16.1%,P< 0.001),and endoscopic treatment (57.3%vs23.9%,P< 0.001).In the validation cohort,the PP patients had a higher proportion of patients with hematemesis (69.6%vs39.7%,P=0.012),lower serum albumin level (P=0.011),higher urea level (P=0.041),and more probability with the endoscopic appearance of adherent thrombosis (39.1%vs14.1%,P=0.008),visible vessels (47.8%vs20.5%,P=0.009) and SRH (78.3%vs35.9%,P< 0.001).The patients with poorer prognosis in the validation cohort had more frequent episodes of rebleeding (30.4%vs0%,P< 0.001),stronger demands for blood transfusion (69.6%vs24.4%,P< 0.001),and a higher proportion of individuals with hospitalization time exceeding 14 d (65.2%vs9.0%,P< 0.001) than those with good outcomes.
Establishment of a new post-endoscopic scoring system for predicting the prognosis of UGIB
The data of the cases in the training cohort were used to determine the impact factors of the prognosis and to establish a new scoring system for UGIB prognostication.The prognostic factors of UGIB were determined by univariate and multivariate logistic regression analysis (Table 2).The univariate analysis showed that age,weight,BMI,previous UGIB history,comorbidities (i.e.,liver disease,cirrhosis,gallstone,autoimmune diseases,cerebral infarction,stroke,peptic ulceration,UGIC,EGVB,and liver failure),signs and symptoms (e.g.,hematemesis,black stool,palpitation,amaurosis,sweat,altered mental status,pulse,SBP,DBP,anemia appearance,lymphocyte count,RBC count,MCV,HCT,hemoglobin,PLT count,C-reactive protein,PT,fibrinogen,D-dimer,albumin,ferritin),treatment history (e.g.,blood transfusion,administration of somatostatin and its analogs),endoscopic manifestations (i.e.,dark spots,bleeding,adherent clots,visible vessels,lesion diameter ≥ 2 cm),SRH,and rebleeding were associated with endpoint events (allP< 0.05).According to the logistic stepwise forward analysis,seven factors were determined as the impact factors for poor UGIB prognosis,including five factors at admission [OR 1.039,95%CI: 1.023-1.055,P< 0.001),albumin (OR 0.912,95%CI: 0.864-0.962,P=0.001),history of liver failure (OR 2.370,95%CI: 1.254-4.480,P=0.008) or stroke (OR 1.710,95%CI: 0.826-3.540,P=0.148),and demand for blood transfusion (OR 4.387,95%CI: 2.458-7.831,P< 0.001)],and two indicators of endoscopy [SRH (OR 4.089,95%CI: 2.192-7.626,P< 0.001) and UGIC (OR 3.795,95%CI: 1.727-8.337,P=0.001)].Rebleeding is extremely important in clinical practice and has been involved in most models for UGIB prognostication.Therefore,we incorporated rebleeding (OR 2.071,95%CI: 0.892-4.809,P=0.090)into the final model.Thus,eight predictors were integrated to conduct a new post-endoscopic prognostic scoring system (MH-STRALP).
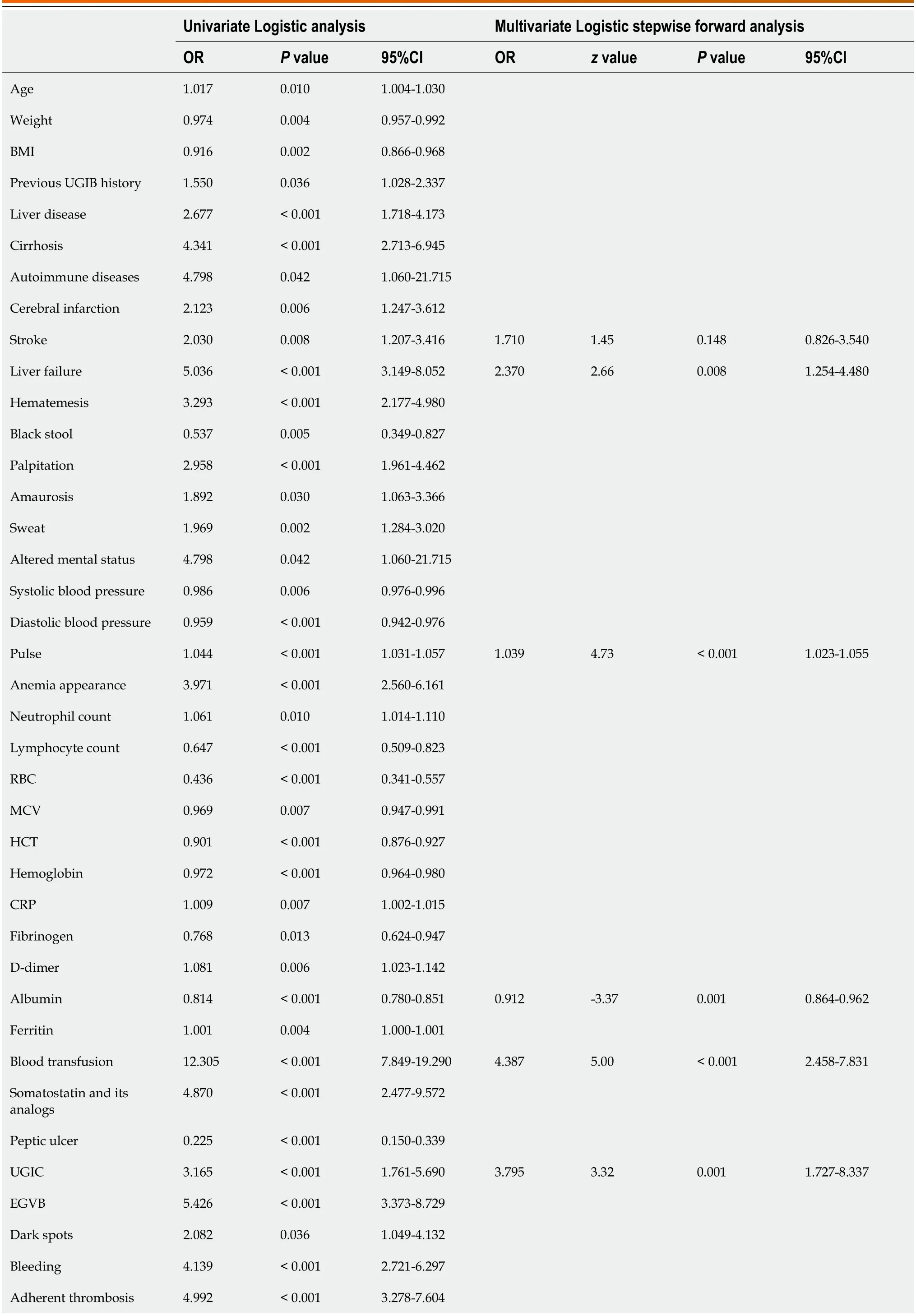
Table 2 Logistic regression analysis for the prognostic factors of upper gastrointestinal bleeding
Performance and validation of MH-STRALP nomogram
A nomogram was determined to present the post-endoscopic prognostic model,MH-STRALP (Figure 2).In the nomogram,each value taken for different predictors was assigned a corresponding score.These scores were then summed to obtain a total score,which in turn corresponds to a probability,representing the predictive value of poor UGIB prognosis.As shown in Table 3 and Figure 3A,based on the ROC curve analysis,the nomogram showed a robust discrimination for UGIB prognosis,with an area under the ROC curve (AUROC) of 0.899 (95%CI: 0.870 to 0.928) in the training cohort,which was higher than the AUROC of other previous scores (i.e.,GBS,Rockall,ABC,AIMS65,and PNED scores).The calibration curve showed that the probabilities for poor outcomes predicted by the nomogram agreed well with the actual probabilities (Figure 3B).Moreover,an internal cross-validation analysis (Figure 3C) in the training cohort showed an AUROC of 0.888 and revealed the potent discrimination of the new nomogram.DCA determination found that the accuracy of MH-STRALP for predicting UGIB outcomes was superior to the GBS,Rockall,ABC,AIMS65,and PNED scores (Figure 3D).In addition,MH-STRALP showed an AUROC of 0.826 (95%CI: 0.734-0.919) in the validation cohort,which was higher than the other score systems,thereby verifying the significance of this new nomogram for UGIB prognostication (Figure 3E,Supplementary Table 2).
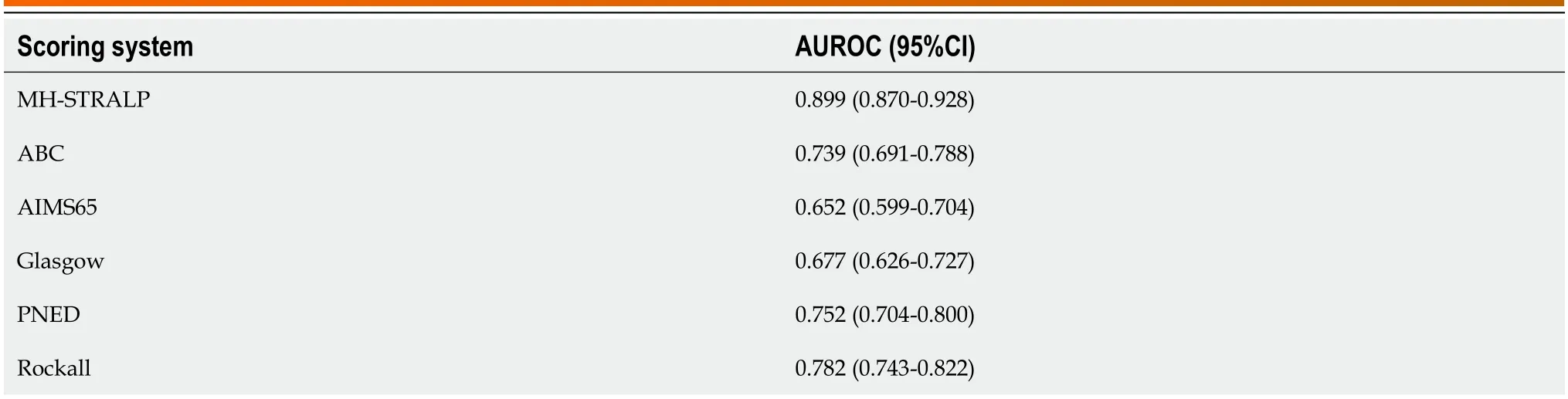
Table 3 Comparison of prognostic predictive ability between MH-STRALP and other scoring systems in the training cohort

Figure 2 Nomogram for the prognostic model of upper gastrointestinal bleeding (MH-STRALP). To calculate the probability of the compound outcomes,points for each parameter are assigned by corresponding values from the “points” axis,and sum of the points is plotted on “total points” axis.UGIC: Upper gastrointestinal carcinoma;SRH: Stigmata of recent hemorrhage.

Figure 3 Performance and validation of the MH-STRALP nomogram. A: The area under the curve (AUC) of the MH-STRALP nomogram for prognostic prediction of upper gastrointestinal bleeding (UGIB) in the training cohort;B: The calibration curve for the prognostic nomogram.The x-axis represents the nomogram-predicted probability and y-axis represents the actual probability of the compound outcomes.A perfect prediction would correspond to the 45° grey line.The brown line represents the entire cohort bias-corrected by bootstrapping (B=1000 repetitions),indicating observed nomogram performance;C: The AUC of the MH-STRALP nomogram in the internal cross-validation analysis in the training cohort;D: The decision curve analysis compared the accuracy for prognostic prediction between MH-STRALP nomogram and other scoring systems;E: The AUC of the MH-STRALP nomogram for prognostic prediction of UGIB in the validation cohort.ROC: Receiver operating characteristic.
Establishment and validation of a pre-endoscopic scoring system for predicting the prognosis of UGIB
Some patients were unable to undergo endoscopy during hospitalization due to various contraindications;therefore,we conducted a new pre-endoscopic model (pre-MH-STRALP score) by removing the endoscopic indicators.Six factors (i.e.,pulse,albumin,history of liver failure or stroke,demand for blood transfusion,and rebleeding) were included in the pre-MH-STRALP score.The AUROCs of the new pre-endoscopic model for discriminating the UGIB prognosis were 0.868 (95%CI: 0.832-0.904) in the training cohort and 0.767 (95%CI: 0.832 to 0.904) in the validation cohort,thereby representing better predictive performance than other pre-endoscopic scoring systems (Figure 4,Table 4,Supplementary Table 3).
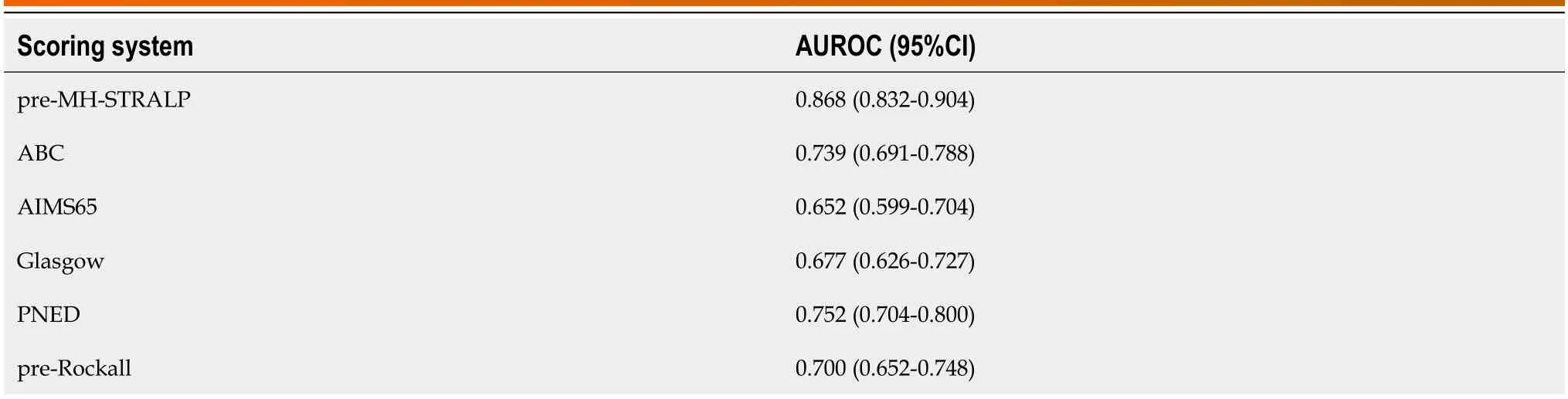
Table 4 Comparison of prognostic predictive ability between pre-MH-STRALP and other pre-endoscopic scoring systems in the training cohort
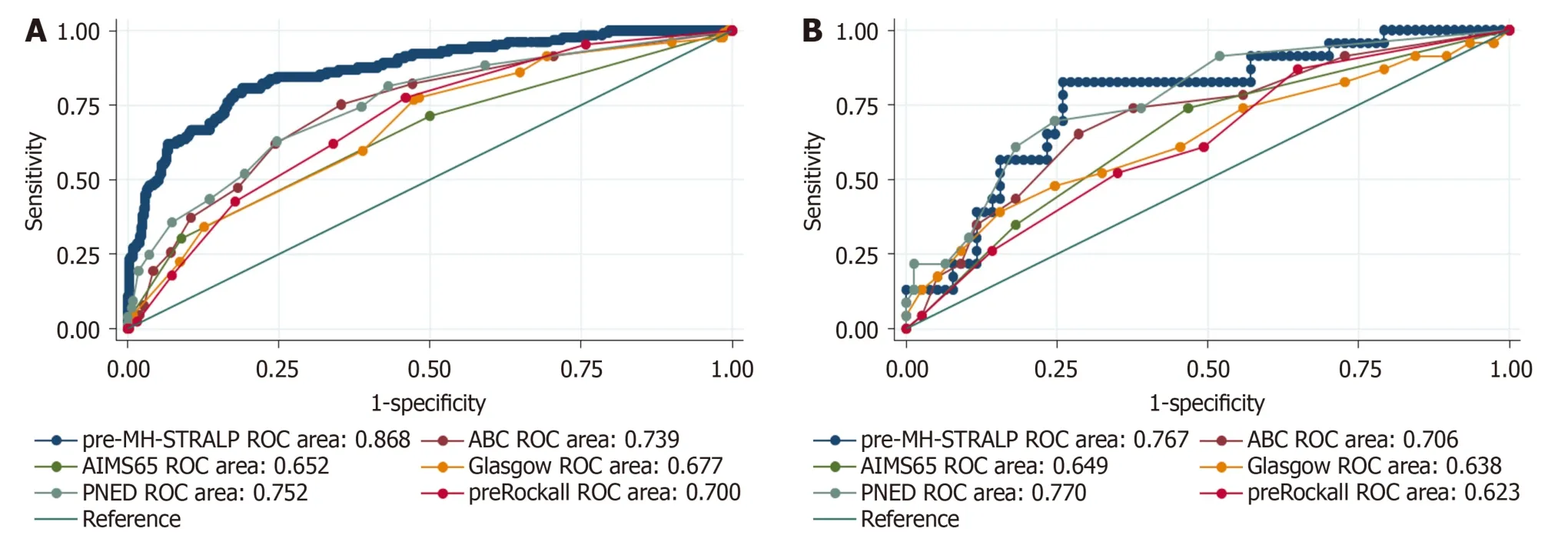
Figure 4 The area under the curve of the pre-endoscopic scoring system (pre-MH-STRALP) for prognostic prediction of upper gastrointestinal bleeding. A: The area under the curve (AUC) of the pre-endoscopic scoring system (pre-MH-STRALP) for prognostic prediction of upper gastrointestinal bleeding (UGIB) in the training cohort;B: The AUC of the pre-endoscopic scoring system (pre-MH-STRALP) for prognostic prediction of UGIB in the validation cohort.ROC: Receiver operating characteristic.
DlSCUSSlON
UGIB is a common emergency and remains challenging to treat and manage.Multiple factors can contribute to the deterioration of the patients' condition and ultimately lead to a PP.To date,drug administrations and emergency endoscopy remain as the standard treatment regimens for UGIB management,as recommended by a series of guidelines[9-12,23,24].However,despite administration of high-dose proton pump inhibitors and other drugs as well as repeated intervention of endoscopic hemostasis,there were still some patients who needed transcatheter embolization or surgical treatment.Several models have already been suggested for UGIB prognostication.Nevertheless,only few studies focused on the compound outcomes,which not only led to poorer survival but also prolonged the length of hospital stay and enhanced medical burden.With this study,we constructed a new scoring system,MH-STRALP,to predict the prognosis of patients with UGIB,with compound endpoint events of undergoing emergency surgery or vascular intervention,being transferred to the ICU,or dying during hospitalization;we formulated a nomogram to present the scoring system.We also conducted a pre-endoscopic model (pre-MH-STRALP score) by removing the endoscopic indicators.With our observation,the two novel scoring systems,MH-STRALP and pre-MH-STRALP score,were both superior to other models (i.e.,GBS,Rockall,ABC,AIMS65,and PNED scores) in predicting the compound outcomes.
Among all the etiologies,UGIC and liver cirrhosis have been regarded as relevant to poor UGIB prognosis.UGIC is the third leading cause of UGIB in addition to ulcers and varices,accounting for 3.7%-5% of UGIB patients[25-27].For 79% of patients with UGIC,UGIB is the initial manifestation of cancer[26].Previous studies shown that the prognosis for UGIC isextremely poor,with a median survival of 1.3-3.0 months after bleeding due to advanced gastric cancer[25,27,28].Because of the severity of the protopathy diseases as well as the difficulty of endoscopic and vascular intervention,it is generally agreed that VUGIB resulting from liver cirrhosis-related hypertension is more rapid and serious as compared with NVUGIB,thereby leading to poorer outcomes.In addition,liver disease-related hypoalbuminemia,malnutrition,coagulation disorders,and immune dysfunction could augment hemorrhage and result in hemostatic difficulty[29-33].In our study,the patients in the PP group had a higher prevalence of UGIC,chronic liver disease,liver cirrhosis;albumin,UGIC,and history of liver failure were the independent risk factors for poor UGIB outcomes.Albumin is the key indicator for liver cirrhosis and liver failure;thus,all these observations demonstrate the impact of UGIC and liver disease on UGIB prognosis.
Some underlying diseases,such as stroke,have been implicated in UGIB prognosis.Stroke,including hemorrhagic and ischemic stroke,is one of the important predispositions of stress ulcer-induced UGIB[34-36].According to an investigation including 331 individuals,the prevalence of UGIB was 20.5% in acute stroke patients aged > 65 years[37].Multiple factors participate in gastric mucosal damage and bleeding induced by stroke,including excessive secretion of gastric acid triggered by overactivity of the vagus nerve,strong and sustained vasoconstriction of the gastric mucosa caused by overexcitation of sympathetic-adrenomedullary system,increased catecholamines secretion in the cerebrospinal fluid and serum,and disruption of the axis between the central nervous system.Furthermore,due to the disturbances in the coagulation and fibrinolytic systems as well as tissue ischemia and hypoxia,patients with UGIB are more prone to stroke.The interaction between the two diseases aggravates the illness and contributes to poorer prognosis.In this study,more patients in the PP group were combined with stroke;stroke was an independent risk factor for poor UGIB outcomes.These findings were consistent with the results of previous studies.
Circulatory failure is the most important manifestation and serious complication of UGIB.UGIB can result in different clinical features of circulatory impairment,including abnormal hypertension or hypotension,decline or rise of heart and pulse rate,hypovolemic shock,and sudden cardiac arrest.According to a previous study,there are two distinct phases of the neurohumoral and hemodynamic responses in acute hemorrhage[38]: The initial arterial baroreceptor-mediated phase and the abruptly progressive phase characterized by withdrawal of sympathetic vasoconstrictor drive.In the initial phase,the medulla oblongata accepts the signals from carotid and aortic pressure receptors as well as from arterial chemoreceptors,and activates sympathetic signals,thus leading to a considerable enhancement of muscle sympathetic activity and sustained elevation of norepinephrine in the muscle and plasma.This causes,the capacitance vessels to constrict,accelerates the intrinsic pacing frequency of the sinus node,and reflexively increases heart rate[39-41].Because the fall in cardiac output is nearly matched by a sympathetically mediated increase in peripheral resistance,the alteration of arterial pressure is not obvious.When blood volume has fallen by a critical amount (approximately 30%),the hemodynamic responses enter the second phase.Due to the debilitation of sympathetic-drived vasoconstrictor,central opioidergic,and serotonergic mechanisms,the patients show a relative or absolute bradycardia as well as a profound fall in blood pressure.Therefore,blood transfusion is a key strategy to correct hypovolemia and circulatory failure induced by UGIB[9,10].Growing evidence have demonstrated the relationship between blood transfusion and further bleeding rates or mortality of UGIB[42-44];these revealed that blood transfusion is an independent prognostic factors for UGIB[43].Based on the current data,pulse and demand for blood transfusion were predictor of PP in patients with UGIB,further confirming the central role of circulatory failure on the outcomes of UGIB.
Rebleeding has been indicated as a predictor for high mortality risk in patients with UGIB[45,46].Based on the Forrest classification,endoscopic manifestations (i.e.,active arterial bleeding,visible vessels,and adherent thrombosis) signify high rebleeding risk,with a rebleeding rate of 90%,50%,and 33% in the absence of endoscopic hemostasis,respectively;these were much higher than those with flat pigmented spots and clean ulcer bases[47,48].In our observation,the overall rebleeding rate of UGIB was 6.9%,with a significant elevation in the PP than in the GP group (3.2%: 20.9%;P< 0.001).Additionally,rebleeding was associated with the compound outcomes by Logistic univariate analysis.Rebleeding has been involved in most of the scoring systems;thus,we ultimately integrated rebleeding into our model for UGIB prognostication.
In recent years,the widespread use of endoscopy facilitates the microscopic diagnosis and hemostatic treatment of UGIB.A microscopic feature,SRH,remains of great importance and is recognized as an independent predictor for UGIB mortality.Moreover,it provides useful and important prognostic information for risk stratification and clinical decision making (e.g.,receiving endoscopic hemostasis or surgical intervention or intervention)[14,49,50].As expected,SRH was one of the most powerful predictors of poor UGIB prognosis in our model.Therefore,this finding encouraged early endoscopic examination and intervention.
There are existing models for UGIB prognostication,including GBS,ABC,PNED,AIMS65,Rockall scores,and so on.Among these,the GBS score was initially established to predict the need for blood transfusion or intervention and to help outpatient emergency physicians to identifying those who need hospitalization.The ABC,PNED,AIMS65,and Rockall scores were established with death as the predictive endpoint event.A previous study showed that the predictive power of the AIMS65 and PNED scores were similar for 30-day mortality,which were better than the Rockall and GBS scores[18].In our study,we formulated newer post-endoscopic (MH-STRALP) and pre-endoscopic (pre-MH-STRALP) scoring systems to predict the prognosis of UGIB by using compound endpoint events (i.e.,undergoing emergency surgery or vascular intervention,being transferred to the ICU,or dying during hospitalization);we presented the scoring system as a nomogram.The AUC of the novel models were significantly higher than the other scores in both the training and validation cohorts,thereby suggesting better prediction efficiency for the compound outcomes of UGIB,whether before or after endoscopy.
There are some limitations in our study.Firstly,this is a retrospective study,which might lead to selection bias.Secondly,we included patients who had undergone endoscopy during hospitalization;the prognostic prediction of UGIB patients who did not undergo endoscopy may be biased.
CONCLUSlON
Taken together,we successfully developed novel post-endoscopic (MH-STRALP) and pre-endoscopic (pre-MH-STRALP) scoring systems to conveniently and accurately predict the prognosis of UGIB.Further large-scale prospective studies are necessary to verify the value of the scor-ing systems.
ARTlCLE HlGHLlGHTS
Research background
Upper gastrointestinal bleeding (UGIB) is divided into nonvariceal UGIB (NVUGIB) and variceal UGIB (VUGIB),with rising NVUGIB cases due to an aging population and more non-steroidal anti-inflammatory drugs use,and VUGIB typically resulting from liver cirrhosis with substantial mortality.Despite medical and endoscopic progress,UGIB maintains a high morbidity and mortality rate,with persistent high hospitalization challenges and a 30-day mortality rate of 11% in China,highlighting its critical status as a healthcare emergency.
Research motivation
UGIB prognostic scoring systems are inconsistently applied in clinical practice,with limited impact on decision-making due to variances in primary outcomes and lack of validation.The absence of trial-based evidence for these scores contributes to their uncertain utility in Chinese clinical settings.
Research objectives
The goal of this study is to identify key factors that influence poor UGIB outcomes (e.g.,the demand for emergency surgery or vascular intervention,being transferred to the intensive care unit,and dying during hospitalization) and develop a simpli-fied,effective scoring system to guide risk stratification and treatment decisions in Chinese UGIB patients.
Research methods
A retrospective study used UGIB patient data from East Hospital as a training cohort and from Changzheng Hospital as a validation cohort to construct and test a new scoring model based on major predictors of UGIB outcomes,including endoscopic findings.A nomogram derived from this model was developed,validated,and compared to existing UGIB scores,with an alternative pre-endoscopic model also assessed.The study employed extensive clinical data and statistical analyses,like multivariate analysis and receiver operating characteristic (ROC) curves,to evaluate the models' effectiveness,focusing on the composite endpoint of emergency surgery,vascular intervention,ICU transfer,or in-hospital mortality.
Research results
Univariate analysis determined factors related to negative outcomes in UGIB,leading to the creation of the MH-STRALP scoring system,which incorporates seven prognostically significant factors plus the risk of rebleeding.The MH-STRALP system showed better prognostic accuracy compared to other established scoring systems (GBS,Rockall,ABC,AIMS65,and PNED),with areas under ROC curves (AUROC) of 0.899 and 0.826 in the training and validation cohorts,whilst the pre-MH-STRALP score also showed better predictive value (AUROCs of 0.868 and 0.767 in the training and validation cohorts,respectively).These two scoring systems are helpful in prognosticating Chinese UGIB patients,providing personalized appropriate treatment and management,and facilitating early clinical decision-making.
Research conclusions
With this study,we constructed new scoring systems,MH-STRALP and pre-MH-STRALP,to predict the prognosis of patients with UGIB,with compound endpoint events of undergoing emergency surgery or vascular intervention,being transferred to the ICU,or dying during hospitalization;we formulated a nomogram to present the scoring system.
Research perspectives
Since this is a retrospective study and we did not make prognostic predictions for patients with UGIB who did not undergo endoscopy,there may be bias.Further large-scale prospective studies are necessary to verify the value of the scoring systems.
ACKNOWLEDGEMENTS
The authors would like to thank the patients and their families for their contribution to this study.
FOOTNOTES
Co-first authors:Jun-Nan Hu and Fei Xu.
Co-corresponding authors:Lan Zhong and Xin Zeng.
Author contributions:Hu JN,Xu F were involved in investigation,acquisition,data collection,and drafting of the manuscript;Sun CY,Wu KM were involved in analysis of data;Hao YR was involved in investigation,acquisition,data collection;Lin Y was involved in concept and design,gathering conflict-of-interest forms and statements,are properly completed;Zhong L,Zeng X were involved in providing details of authorship,acquisition and interpretation of funding,ethics committee approval documentation,review and edit the manuscript.All authors were involved in the critical review of the results and have contributed to,read,and approved the final manuscript.Hu JN and Xu F contributed equally to this work as co-first authors.The reasons for designating Hu JN and Xu F as co-first authors are as follows.They have equally contributed to the project by leading and executing a critical component of the research,namely developing the computational model,solving pivotal theoretical problems.They also shared equal responsibility in the process of writing,editing,and refining the manuscript,as well as preparing the visualizations that greatly enhance the clarity and impact of the work.Zhong L and Zeng X contributed equally to this work as co-corresponding authors.The reasons for designating Zhong L and Zeng X as co-corresponding authors are as follows.Zhong L and Zeng X played a crucial role in providing author details,acquiring and interpreting funding,obtaining ethics committee approval documents,and revising and editing the manuscript.The contributions of both authors were essential for the smooth progress of the research and the writing of the final paper,reflecting their significant leadership and coordination role throughout the research process.Their expertise and contributions were indispensable in ensuring the quality and integrity of the study.By involving themselves in every key stage of the project and bearing the responsibility of ensuring the research adhered to ethical and funding body standards,the designation of co-corresponding authors serves as recognition of their significant work.Moreover,they ensured that the paper had proper technical and administrative support during the submission process and after publication,guaranteeing high standards and transparency for the research and manuscript.Therefore,appointing Zhong L and Zeng X as co-corresponding authors is a fair and appropriate reflection of their substantial contributions and corresponding responsibilities to this research.This research was completed as a result of collaborative teamwork,and designating co-first authors and co-corresponding authors accurately reflects the distribution of responsibility and the burden of time and effort required to complete the study and the manuscript.It also embodies our team’s spirit of collaboration,the equitable contributions,and the diversity present within our group.
Supported byKey Disciplines Group Construction Project of Shanghai Pudong New Area Health Commission,No.PWZxq2022-06;Medical discipline Construction Project of Pudong Health Committee of Shanghai,No.PWYgf2021-02;Joint Tackling Project of Pudong Health Committee of Shanghai,No.PW2022D08;and the Medical Innovation Research Project of the Shanghai Science and Technology Commission,No.22Y11908400.
lnstitutional review board statement:The study protocol was reviewed and approved by the Institutional Ethics Committee of Shanghai East Hospital (Approval No.2020SL018).
lnformed consent statement:Given this article is a retrospective study,an informed consent form is not included.
Conflict-of-interest statement:Dr.Zeng has nothing to disclose.
Data sharing statement:The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yong Lin 0000-0002-2653-7143;Lan Zhong 0000-0002-6947-3266;Xin Zeng 0000-0002-7562-9909.
S-Editor:Lin C
L-Editor:A
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2024年3期
World Journal of Gastrointestinal Surgery2024年3期
- World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
