Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
Shamir O Cawich,Elijah Dixon,Parul J Shukla,Shailesh V Shrikhande,Rahul R Deshpande,Fawwaz Mohammed,Neil W Pearce,Wesley Francis,Shaneeta Johnson,Johann Bujhawan
Abstract BACKGROUND Pancreaticoduodenectomy (PD) is a technically complex operation,with a relatively high risk for complications.The ability to rescue patients from post-PD complications is as a recognized quality measure.Tailored protocols were instituted at our low volume facility in the year 2013.AIM To document the rate of rescue from post-PD complications with tailored protocols in place as a measure of quality.METHODS A retrospective audit was performed to collect data from patients who experienced major post-PD complications at a low volume pancreatic surgery unit in Trinidad and Tobago between January 1,2013 and June 30,2023.Standardized definitions from the International Study Group of Pancreatic Surgery were used to define post-PD complications,and the modified Clavien-Dindo classification was used to classify post-PD complications.RESULTS Over the study period,113 patients at a mean age of 57.5 years (standard deviation [SD] ± 9.23;range: 30-90;median: 56) underwent PDs at this facility.Major complications were recorded in 33 (29.2%) patients at a mean age of 53.8 years (SD: ± 7.9).Twenty-nine (87.9%) patients who experienced major morbidity were salvaged after aggressive treatment of their complication.Four (3.5%) died from bleeding pseudoaneurysm (1),septic shock secondary to a bile leak (1),anastomotic leak (1),and myocardial infarction (1).There was a significantly greater salvage rate in patients with American Society of Anesthesiologists scores ≤ 2 (93.3% vs 25%;P=0.0024).CONCLUSION This paper adds to the growing body of evidence that volume alone should not be used as a marker of quality for patients requiring PD.Despite low volumes at our facility,we demonstrated that 87.9% of patients were rescued from major complications.We attributed this to several factors including development of rescue protocols,the competence of the pancreatic surgery teams and continuous,and adaptive learning by the entire institution,culminating in the development of tailored peri-pancreatectomy protocols.
Key Words: Pancreas;Complication;Rescue;Failure;Morbidity;Mortality;Pancreaticoduodenectomy
lNTRODUCTlON
Pancreaticoduodenectomy (PD) remains the best therapeutic option for peri-ampullary malignancies[1,2].As it is a technically complex operation,PDs should be performed by experienced teams who are facile with the operative steps and management of complications when they occur.The ability to rescue patients from succumbing to post-PD complications is recognized as a quality measure in modern practice[3-7].
Our facility in the Caribbean is a tertiary referral center where experienced pancreatic surgeons perform PD at low volumes.The primary aim of this study was to evaluate rescue rates after PD and to document short-term outcomes using tailored peri-pancreatic protocols.
MATERlALS AND METHODS
We secured ethics approval to collect data for this study from a pancreatic surgery unit in the Eastern Caribbean.A dedicated unit was established on January 1,2013,staffed by pancreatic surgeons,anesthetists,and support staff.
In this study,we carried out an audit to identify all consecutive patients who underwent PD at this facility over one decade,from January 1,2013 to June 30,2023.Patients were identified from operating room registers.Then hospital records were retrieved to identify patients who experienced a major complication after PD.The following data were collected from these records: patient demographics,operative details,postoperative complications,and 30-d mortality.
The criteria to be eligible for inclusion were: Age > 18 years,PD during the specified study period,availability of hospital records,and documentation of a major complication.Patients were excluded if they underwent left-sided or total pancreatic resections,had missing or incomplete records,were transferred to other facilities for any reason,and experienced minor or no complications.
We used standardized definitions from the International Study Group of Pancreatic Surgery[8,9] to define post-PD complications and the definition of pancreatic fistula proposed by the International Study Group on Pancreatic Fistula criteria[10,11].The modified Clavien-Dindo classification[12] was used to classify post PD complications.Complications were further divided into medical and procedure-related complications using standardized classifications[13,14].Procedure-related complications include pancreatic fistula,delayed gastric emptying,surgical site infection,organ space collection,post-pancreatectomy hemorrhage,anastomotic leaks,and bile leaks[13,14].
Rescue was defined as the proportion of patients who were salvaged after a major (Claviden-Dindo ≥ 3a) post-PD complication was treated[3].Descriptive statistics were generated using SPSS version 16.0.The χ2andt-tests were used to compare rescue rates based on patient sex,patient age (≤ 55 yearsvs> 55 years),type of complication (medicalvsprocedure-related),Eastern Cooperative Oncology Group performance scores (ECOG 0-1vs2-4),and physical status using the American Society of Anesthesiologists’ risk score (ASA 1-2vs3-5).P< 0.05 was considered statistically significant.
RESULTS
Over the study period,113 patients underwent PDs at this facility.There were 71 males and 62 females at a mean age of 57.5 years (standard deviation [SD] ± 9.23;range: 30-90;median: 56).Major complications were recorded in 33 (29.2%) patients after PD.In the subgroup with major complications,there were 23 males and 10 females at a mean age of 53.8 years (SD: ± 7.9;range: 30-70;median: 53).Table 1 outlines the individual complications.
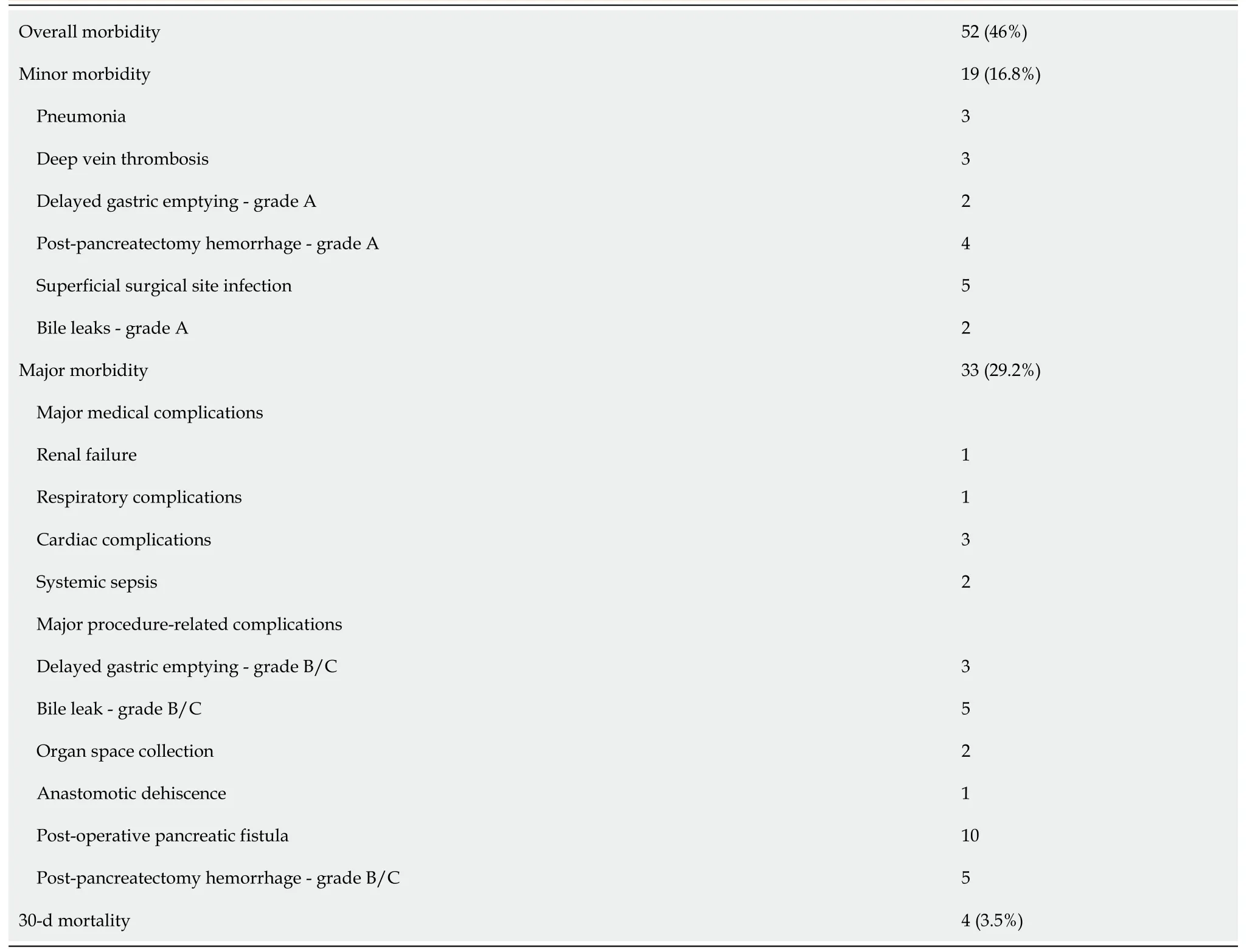
Table 1 Complications after 113 pancreaticoduodenectomies
Twenty-nine patients who experienced major morbidity were salvaged after aggressive treatment of their complication.Therefore,the salvage rate at this facility was 87.9%.
Four (3.5%) patients died as a direct consequence of their complications,resulting in an FTR rate of 12.1%.The complications from which patients could not be rescued included: Post-pancreatectomy hemorrhage from a bleeding pseudoaneurysm,septic shock secondary to a bile leak,intra-abdominal collections from an anastomotic leak,and a cardiac insufficiency due to myocardial infarction.
There were seven major medical complications and six (85.6%) were rescued after treatment of the complication.There were 26 patients with procedure-related complications and 23 (88.5%) of these patients were rescued.There was no statistically significant difference in salvage rates for medicalvsprocedure-related complications (P=0.0391).
We found that salvage rates were slightly higher in patients with age ≤ 55 years (89.5%vs83.3%;P=0.743) and ECOG scores ≤ 1 (91.3%vs80%;P=0.361),female sex (90%vs87%;P=0.951),although neither achieved statistical significance.Due to the retrospective nature of data collection,we could not evaluate the relationship between salvage rates and body mass index (BMI).However,there was a significantly greater salvage rate in patients with ASA scores ≤ 2 (93.3%vs25%;P=0.0024).
DlSCUSSlON
Rescue from salvageable complications requires early recognition and treatment of complications.Since PD is recognized to be a technically challenging procedure with high inherent complication rates[1-4],isolated analyses of morbidity and mortality are not the best quality measures[3,6,7].Instead,interhospital variations in mortality bear a closer relationship to the rates of rescue or failure thereof[3-7].
At our center,PD was accompanied by 29.2% major morbidity and 3.5% mortality,which is on par with reports in the surgical literature[3,13-18].More importantly,we were able to rescue 89% of patients from major complications.The failure rate (12.1%) was at the upper limit of that reported from high-volume centers,ranging from 5.4%[8] to 12.5%[19].This means there may still be room for improvement in complication management at our center.
Prior data suggest that rescue rates are directly proportional to hospital case volume[3,6,7,20,21].Although there is no consensus on what constitutes a high-volume center,most authors consider high-volume hospitals as those performing > 18 PDs annually[22-26].van Rijssenet al[3] suggested that hospital volume > 40 per year was an an independent predictor of rescue.Therefore,with an annual volume of 11.3 PDs per year,our hospital does not qualify as high volume.
We found that the only factor that predicted rescue was the patients’ physical status using the ASA risk score,in agreement with published data[3,27,28].The surgical literature suggests that other factors predicting failure to rescue include patient-related factors,such as male sex[3],increasing age[3,27],high BMI[3],and co-morbidities[6,28,29].Hospital-specific factors include understaffing[6,28,30],intensive care unit support[6,28,29],hospital technology status[3],nurse-to-patient ratio[6,28,29],and availability of interventional radiology[27].
Our results suggest that rescue is not necessarily related to case volumes alone.It is a much more complex issue that requires a multidisciplinary team approach,appropriate hospital equipment,and diligence on the part of the care team.In our setting where a new pancreatic service was being formed,we appreciated that a surgeon-led drive was necessary to ensure that the facility focused on recognized factors contributing to good outcomes,such as quaternary training for hepato-pancreato-biliary teams[31],trained nursing teams[32],development of care pathways[32],multidisciplinary approach to care[1,2],tailored centralization pathways[33],and continuous hospital learning[32].We took a holistic approach,by creating peri-pancreatic protocols that are tailored to our resource-poor system,as summarized in Table 2.
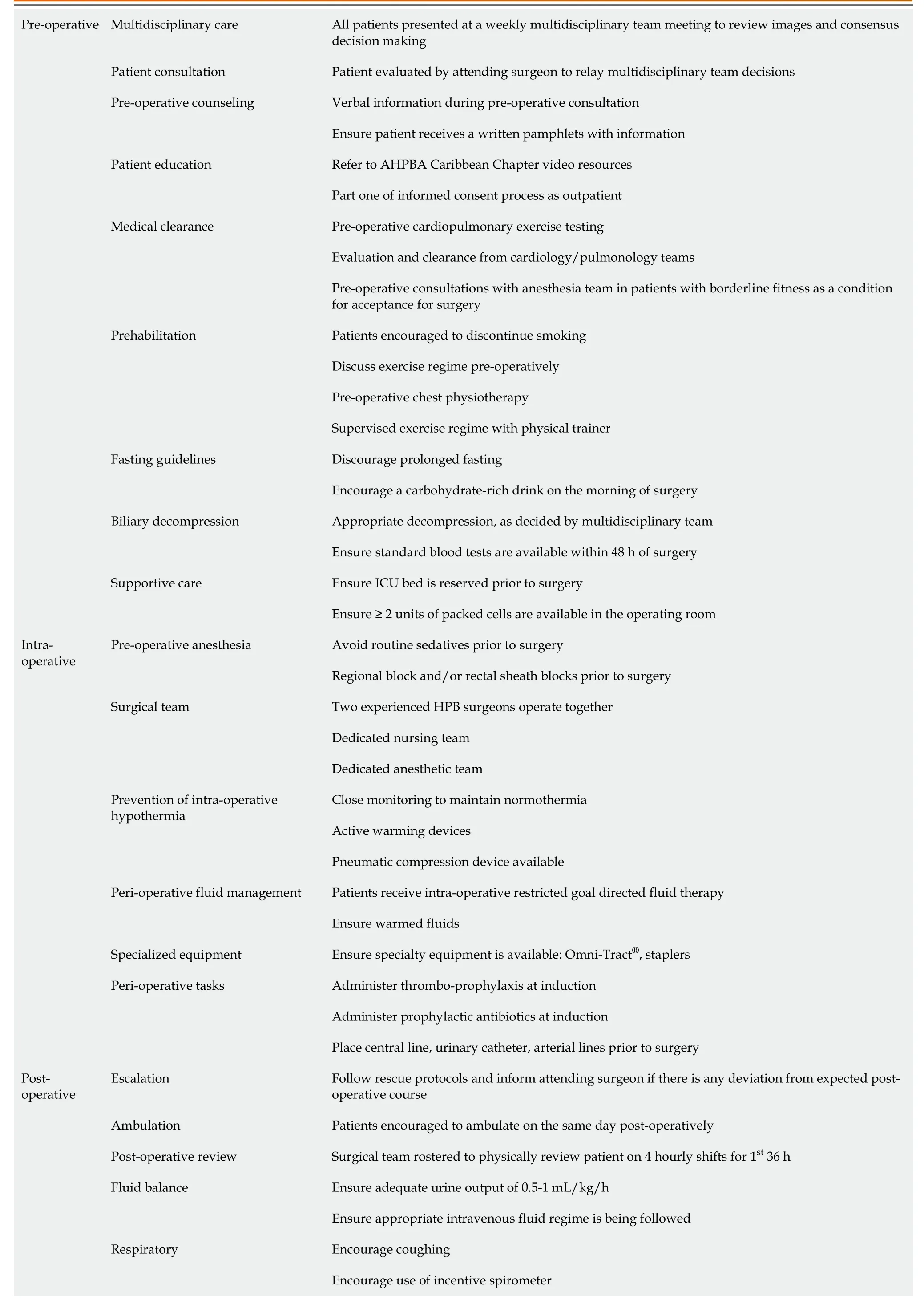
Table 2 Caribbean peri-pancreatic surgery protocols
It is important to recognize that the attending surgeon has less control in the post-operative period.It is the diligence of the nursing and support staff that allows complications to be recognized early,the experience of junior medical staff that allows appropriate steps to be taken and seniors to be notified,and the quality of care from the entire care team that will determine whether a patient is rescued.Team leaders/attending surgeons must recognize that they need cooperation from all categories of hospital staff and,many times,this is an exercise in diplomacy.To do this,attending surgeons must rely on charisma power (the ability to influence behavior through force of character) instead of coercive power (influencing others through fear or the ability to punish subordinates)[37].
It is also important for the surgeon to be able to adapt to their working environment.For example,we understood early that our facility battled with unavailability of intensive care unit space,paucity of blood products,shortage of consumables,and inconsistent supply of drugs,among others.Recognizing that these would have a negative impact on patient recovery,we emphasized good interdisciplinary relationships and the surgical team took the responsibility to ensure that everything needed was available prior to surgery.This was an example of continuous,adaptive learning by the entire institution[1,12,32],culminating in the development of the tailored peri-pancreatectomy protocols[32].We firmly believe that this holistic approach has contributed to the good outcomes in this resource-poor,low-volume facility.
CONCLUSlON
This paper adds to the growing body of evidence that volume alone should not be used as a marker of quality for patients requiring PD.Despite low volumes at our facility,we demonstrated that 87.9% of patients were rescued from major complications.We attributed this to several factors including development of rescue protocols,the competence of the pancreatic surgery teams and continuous,adaptive learning by the entire institution,culminating in the development of tailored peri-pancreatectomy protocols.
ARTlCLE HlGHLlGHTS
Research background
Peri-operative outcomes differ between institutions due to a variety of factors.This can affect the way individual hospitals manage complications,and also their mortality rates after pancreaticoduodenectomies (PDs).
Research motivation
Our facility in the Caribbean is a low-volume center with numerous challenges.Tailored peri-pancreatic protocols were devised specifically to compensate for challenges at our facility.These have not been evaluated prior to this study.
Research objectives
The ability to rescue patients from post-PD complications is as a recognized quality measure.This study sought to document the rate of rescue from post-PD complications with tailored protocols in place as a measure of quality.
Research methods
A 10-year retrospective audit was performed to evaluate rescue rates in patients who experienced major post-PD complications.Standardized definitions from the International Study Group of Pancreatic Surgery were used to define post-PD com-plications and the modified Clavien-Dindo classification was used to classify post-PD complications.All data were examined with SPSS version 18.0.
Research results
There were 113 patients who underwent PDs and 33 experienced major morbidity.Twenty-nine (87.9%) patients were salvaged after aggressive treatment of their complication.There was a significantly greater salvage rate in patients with American Society of Anesthesiologists scores ≤ 2 (93.3%vs25%;P=0.0024).
34. A regular blow-out: Blow-out is a colloquialism97 from the UK meaning An excessive spree of drinking, eating, spending or sex (Duckworth 2003). Andrew Lang considers phrase this to be an example of Hansel s vulgarity in a footnote to the story in The Blue Fairy Book.
Research conclusions
Despite low volumes and multiple hospital challenges,we were able to achieve acceptable rescue rates after post-PD complications.We attributed this to several factors including development tailored peri-pancreatectomy protocols.
Research perspectives
This adds to existing data that volume alone should not be used as a quality measure.It encourages further research with larger numbers since this early research shows encouraging results.
FOOTNOTES
Author contributions:Cawich SO,Dixon E,Sukla PJ,and Shrikhande SV designed the research;Cawich SO,Mohammed F,Pearce NW,and Francis W performed the research;Deshpande R,Pearce NW,Johnson S,and Bujhawan J contributed data analytic tools;Cawich SO,Mohammed F,Deshpane R,Pearce NW,and Johnson S analyzed the data;Cawich SO,Dixon E,Sukla PJ,and Shrikhande SV wrote the paper;Cawich SO,Dixon E,Sukla PJ,Shrikhande SV,Deshpande R,Mohammed F,Pearce NW,Francis W,Johnson S,and Bujhawan J checked the manuscript for scientific accuracy.
lnstitutional review board statement:This study was approved by the Campus Research Ethics Committee,St.Augustine.
lnformed consent statement:This was a retrospective review of written hospital records,the requirement for informed consent was waived by the local institutional review board.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Data sharing statement:All data are stored by the corresponding author and will be released upon reasonable request.
STROBE statement:The authors have read the STROBE Statement—checklist of items,and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Trinidad and Tobago
ORClD number:Shamir O Cawich 0000-0003-3377-0303;Parul J Shukla 0000-0003-3599-4968;Shailesh V Shrikhande 0000-0002-8036-4212;Rahul R Deshpande 0000-0002-1368-4144;Fawwaz Mohammed 0000-0002-1346-8628;Neil W Pearce 0000-0002-3182-7268;Wesley Francis 0000-0003-3174-1015.
S-Editor:Gong ZM
L-Editor:Filipodia
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2024年3期
World Journal of Gastrointestinal Surgery2024年3期
- World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
- Analysis of the impact of immunotherapy efficacy and safety in patients with gastric cancer and liver metastasis
