Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
Konstantin Y Tchilikidi
Abstract This editorial contains comments on the article “Systematic sequential therapy for ex vivo liver resection and autotransplantation: A case report and review of literature” in the recent issue of World Journal of Gastrointestinal Surgery.It points out the actuality and importance of the article and focuses primarily on the role and place of ex vivo liver resection and autotransplantation (ELRAT) and systemic therapy,underlying molecular mechanisms for targeted therapy in perihilar cholangiocarcinoma (pCCA) management.pCCA is a tough malignancy with a high proportion of advanced disease at the time of diagnosis.The only curative option is radical surgery.Surgical excision and reconstruction become extremely complicated and not always could be performed even in localized disease.On the other hand,ELRAT takes its place among surgical options for carefully selected pCCA patients.In advanced disease,systemic therapy becomes a viable option to prolong survival.This editorial describes current possibilities in chemotherapy and reveals underlying mechanisms and projections in targeted therapy with kinase inhibitors and immunotherapy in both palliative and adjuvant settings.Fibroblast grow factor and fibroblast grow factor receptor,human epidermal growth factor receptor 2,isocitrate dehydrogenase,and protein kinase cAMP activated catalytic subunit alpha (PRKACA) and beta (PRKACB) pathways have been actively investigated in CCA in last years.Several agents were introduced and approved by the Food and Drug Administration.They all demonstrated meaningful activity in CCA patients with no global change in outcomes.That is why every successfully treated patient counts,especially those with advanced disease.In conclusion,pCCA is still hard to treat due to late diagnosis and extremely complicated surgical options.ELRAT also brings some hope,but it could be performed in very carefully selected patients.Advanced disease requires systemic anticancer treatment,which is supposed to be individualized according to the genetic and molecular features of cancer cells.Targeted therapy in combination with chemo-immunotherapy could be effective in susceptible patients.
Key Words: Perihilar cholangiocarcinoma;Klatskin’ tumor;Ex vivo liver resection and autotransplantation;Chemotherapy;Ⅰmmunotherapy;Targeted therapy
lNTRODUCTlON
Cholangiocarcinoma (CCA) is the main malignancy in the biliary tract.It is classified into three subtypes according to localization.Intrahepatic CCA is the second primary liver cancer after hepatocellular carcinoma (HCC).Perihilar CCA (pCCA) or Klatskin’ tumor originates from left,right,and common hepatic ducts distal to second order biliary branches and proximal to the cystic duct confluence.Distal CCA arises from the common bile duct proximal to the Vater’s ampula.In fact,CCA is a heterogeneous group of malignancies with different genetic and molecular features[1-4].Those genetic and molecular properties make this malignancy chemo-radio-resistant,shrinking the number of available therapeutic options.
The only curative option is radical surgery.However,the location of pCCA leads to late diagnosis of the disease frequently in advanced stage[1].In addition,surgical excision and reconstruction become extremely complicated and not always could be performed even in localized disease.
Results of allogeneic liver transplantation (LT) in CCA did not bring this procedure to routine use like in HCC.As stated by Sapisochínet al[5],as well as other authors,pCCA could be an accepted indication for orthotopic LT in some centers under a strict selection process and after neoadjuvant chemoradiation.Intrahepatic CCA is a formal contraindication for LT in most centers worldwide due to the poor reported results,despite that neoadjuvant chemoradiation makes them better[5-7].
On the other hand,ex vivoliver resection auto-transplantation (ELRAT),since first introduced by Pichlmayret al[8] in 1988,has taken its place among surgical options for non-malignant lesions and malignancies including carefully selected pCCA patients[8,9].
Systemic anticancer therapy in pCCA has common limitations as in other CCA locations.Just a few chemotherapy regimens showed certain efficacy.Due to recent advances in genetic and molecular mapping,targeted agents have started to become treatment options for selected CCA patients.They open new possibilities in advanced stage CCA.Despite everything,CCA is still a highly lethal disease that requires complicated surgical excision and is resistant to systemic therapy.That is why every successful treatment should be taken into account.One of them is the case report by Huet al[10] “Systematic sequential therapy forex vivoliver resection and autotransplantation: A case report and review of literature” published in the recent issue ofWorld Journal of Gastrointestinal Surgery[10].
ROLE OF EX VIVO LlVER RESECTlON AND AUTO-TRANSPLANTATlON lN PERlHlLAR CHOLANGlOCARClNOMA TREATMENT
Hardyet al[11,12] in 1963 first reported extracorporeal procedures with organs followed by kidney re-implantation after high ureteral injury.Newly introduced in the 1980s,reduced-size,split and auxiliary LT were techniques that precludedex situliver resections[13-15].Publications about ELRAT started with Pichlmayret al[8] in 1988[8].ELRAT allows avoiding scarce donor organs and lifelong immunosuppression.Development of this surgical procedure led to different technical subtypes.Now many authors recognizein vivototal hepatectomy followed by ELRAT andin vivopartial hepatectomy followed by ELRAT[9,16].Despite that ELRAT started to be used in patients with malignancies,patients with benign liver diseases far overweighed them now,mainly due to hepatic alveolar echinococcosis[16-18],where some authors reported low perioperative mortality and good survival[17-20].
Results in cancer patients are still controversial with higher morbidity and mortality that do not make ELRAT become a procedure widely used in these settings[2].According to Zawistowskiet al[20],among 244 patients involved in 53 studies,the 30-d mortality did not differ among patients with the nonmalignant and malignant diseases (11.3%vs6.3%,P=0.181).The 90-d mortality was higher for malignant tumors (21.6%vs8.2%,P=0.004),as well as in-hospital mortality (18.3%vs2.7%,P< 0.001).The postoperative 1-year survival was worse in the malignant group (65.0%vs89.7%,P< 0.001).Major postoperative complications took place less commonly in the nonmalignant group (21.0%vs50.0%,P< 0.001).Post-hepatectomy liver failure occurred more frequently among patients with malignant tumors (23.0%vs8.9%,P=0.006;Table 1)[20].
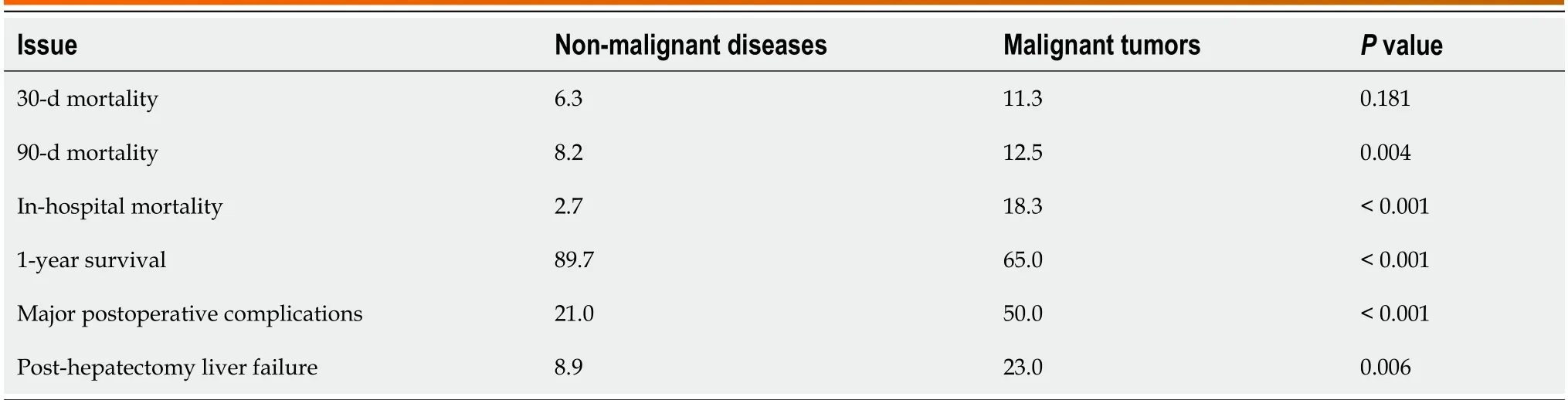
Table 1 Results of ex vivo liver resection and auto-transplantation in malignant and non-malignant settings (%)
Nevertheless,several publications on ELRAT in malignancies including pCCA appeared in last years.That allows Katoet al[21] in 2020 and Weineret al[22] in 2022 as well as other authors to make conclusion about this method as an alternative treatment in selective cancer patients[21,22]. Some researchers performed ELRAT for CCA with no additional anticancer therapy.Others combined them[16,23].pCCA patients are not a preferable population for ELRAT.Despite good early results of the treatment in the article reported by Huet al[16],it would be necessary to continue surveillance.
ROLE OF SYSTEMlC CHEMOTHERAPY lN CHOLANGlOCARClNOMA MANAGEMENT
Due to the lack of specific clinical presentations in early stages,most of biliary tract carcinomas are diagnosed as advanced disease[1,24],where patients have lost their chance for routine curative treatment.Thus,systemic anticancer therapy becomes the procedure of choice in neo-adjuvant and palliative settings.With curative resections,both adjuvant and neo-adjuvant chemotherapy prolonged overall survival and disease-free survival[25,26].However,both studies did not find survival advantage of neo-aduvant chemotherapyvsadjuvant chemotherapy in sensitivity analysis.Since first reported in 2010,results of the ABC-02 trial (NCT00262769) made the gemcitabine and cisplatin regimen most popular.This doublet chemotherapy confirmed its superiority over other cytostatics.Its efficacy has allowed gemcitabine/cisplatin to become first line chemotherapy in CCA[27].Nevertheless,this regimen could increase resectability only in few patients.In addition,most of patients required dose adaptions[28].That forced researchers to seek other systemic agents including targeted therapy to increase survival and as a bridge to curative surgery in advanced disease.
TARGETED THERAPY AS A TREATMENT OPTlON lN CHOLANGlOCARClNOMA PATlENTS
Rapid development of cancer genetic mapping and molecular mechanism discovery in the last decade has changed targeted therapy from experimental anticancer treatment to widely accepted.The fibroblast grow factor (FGF) and FGF receptor (FGFR) pathway is considered to be one of the most important pathways in CCA.Munugalaet al[29] further discovered that the isocitrate dehydrogenase mutations took a significant percentage in different subsets of CCA[29,30].Drugs include infigratinib,erdafitinib,TAS-120 (an irreversible pan-FGFR inhibitor),pemigatinib (a potent,selective oral inhibitor of FGFR isoforms 1,2,and 3).Pemigatinib becomes the first Food and Drug Administration (FDA) approved anti-FGFR2 agent.They all demonstrated meaningful activity in CCA patients with no global change in outcomes[29,30].Some other authors considered that extrahepatic CCA including pCCA is more related to human epidermal growth factor receptor 2 (HER2) and the protein kinase cAMP activated catalytic subunit alpha (PRKACA) and beta (PRKACB) pathways[31,32].The antibody-drug conjugate trastuzumab emtansine experimentally used by some researchers in CCA settings showed higher activity in CCA cell lines with higher HER2 expression[33,34],though HER2 agents act indirectly on the FGF/FGFR pathway too[29,30].
Immunotherapy becomes a game changer in some malignancies such as melanoma,but unfortunately not in CCA.Results of programmed death protein ligand 1 (PD-L1) inhibitors pembrolizumab and nivolumab were mixed[29,35-37].Programmed death protein 1 (PD-1)/PD-L1 inhibitors can be used in high microsatellite instable (MSI-H) tumors.MSI-H as a result of DNA mismatch repair defects (dMMR) could appear in different malignancies.MSI-H is rare in intrahepatic CCA,but more frequent in extrahepatic CCA[38].The phase III TOPAZ-1 trial presented promising results for the PD-L1 inhibitor durvalumab in combination with gemcitabine/cisplatin,mostly confirmed by Riminiet al[39] and Maciaset al[40].Maciaset al[40] in their recent editorial article called the above regimen “new first-line standard of care for patients with advanced biliary tract cancer after more than 10 years of chemotherapy alone”[40,41].The FDA recommended pembrolizumab as a second line therapy for MSI-H/dMMR cancers[42,43].Results of the phase III KEYNOTE-966 trial showed survival benefit by adding pembrolizumab to gemcitabine/cisplatin in advanced CCA[44].
Lenvatinib,as a multi-kinase inhibitor of VEGF receptors 1-3,FGF receptors 1-4,platelet derived growth factor receptor α,KIT,and RET,selectively inhibits tyrosine kinase receptors involved in tumor growth and angiogenesis[45].Tislelizumab is a PD-1 monoclonal IgG4 antibody of high affinity that is mainly used in hematological malignancies and advanced solid cancers,which was conditionally approved in China[45].Dinget al[45] reported successful neoadjuvant therapy with gemcitabine/cisplatin/lenvatinib/tislelizumab in patients with advanced intraheptic CCA followed by surgical resection with no recurrence at the 10-month follow-up[45].
Infigratinib is a reversible ATP-competitive FGFR 1-3 inhibitor.It is actively investigating now.Yuet al[46] concluded that tumor resistance to reversible FGFR inhibitors including infigratinib could be a barrier for the clinical benefits of infigratinib in CCA.They also proposed perspectives with its future administration in combination with immunotherapy[46].
Anticancer therapy in the article of Huet al[10] included conditionally approved agents.So again,further surveillance is necessary.
CONCLUSlON
pCCA is still hard to treat due to late diagnosis and extremely complicated surgical options.ELRAT also brings some hope,but it could be performed only in carefully selected patients.Advanced disease requires systemic anticancer treatment,which is supposed to be individualized according to the genetic and molecular features of cancer cells.Targeted therapy in combination with chemo-immunotherapy could be effective in susceptible patients.
FOOTNOTES
Author contributions:Tchilikidi KY is the sole author of this manuscript.
Conflict-of-interest statement:The author reports no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Russia
ORClD number:Konstantin Y Tchilikidi 0000-0002-8054-5777.
S-Editor:Li L
L-Editor:Wang TQ
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2024年3期
World Journal of Gastrointestinal Surgery2024年3期
- World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
- Analysis of the impact of immunotherapy efficacy and safety in patients with gastric cancer and liver metastasis
