Clinical observation of extraction-site incisional hernia after laparoscopic colorectal surgery
Bao-Hang Fan,Ke-Li Zhong,Li-Jin Zhu,Zhao Chen,Fang Li,Wen-Fei Wu
Abstract BACKGROUND Laparoscopic colorectal cancer surgery increases the risk of incisional hernia (IH) at the tumor extraction site.AIM To investigate the incidence of IH at extraction sites following laparoscopic colorectal cancer surgery and identify the risk factors for IH incidence.METHODS This study retrospectively analyzed the data of 1614 patients who underwent laparoscopic radical colorectal cancer surgery with tumor extraction through the abdominal wall at our center between January 2017 and December 2022.Differences in the incidence of postoperative IH at different extraction sites and the risk factors for IH incidence were investigated.RESULTS Among the 1614 patients who underwent laparoscopic radical colorectal cancer surgery,303 (18.8%),923 (57.2%),171 (10.6%),and 217 (13.4%) tumors were extracted through supraumbilical midline,infraumbilical midline,umbilical,and off-midline incisions.Of these,52 patients developed IH in the abdominal wall,with an incidence of 3.2%.The incidence of postoperative IH was significantly higher in the off-midline incision group (8.8%) than in the middle incision groups [the supraumbilical midline (2.6%),infraumbilical midline (2.2%),and umbilical incision (2.9%) groups] (χ2=24.985;P < 0.05).Univariate analysis showed that IH occurrence was associated with age,obesity,sex,chronic cough,incision infection,and combined diabetes,anemia,and hypoproteinemia (P < 0.05).Similarly,multivariate analysis showed that off-midline incision,age,sex (female),obesity,incision infection,combined chronic cough,and hypoproteinemia were independent risk factors for IH at the site of laparoscopic colorectal cancer surgery (P < 0.05).CONCLUSION The incidence of postoperative IH differs between extraction sites for laparoscopic colorectal cancer surgery.The infraumbilical midline incision is associated with a lower hernia rate and is thus a suitable tumor extraction site.
Key Words: Ⅰncisional hernia;Laparoscopy;Colorectal cancer;Ⅰncision infection
lNTRODUCTlON
Tumor specimens are typically extracted by enlarging the trocar during radical laparoscopic procedures for colorectal cancer.This is commonly achieved through supraumbilical midline,infraumbilical midline,umbilical,and off-midline incisions[1] of approximately 4-6 cm in length.Although these incisions are significantly substantially smaller than an open incision,they can lead to complications such as incisional hernia (IH).IH arises from inadequate healing of the tendinous layer of the abdominal wall.It is a common complication following abdominal surgery,with an incidence ranging from 2% to 11%[2].Both traditional open and laparoscopic surgeries carry a risk of IH,thereby impacting the postoperative recovery of patients[3].Previous research on IH has predominantly focused on traditional open surgery.However,the incidence and risk factors of IH following laparoscopic surgery remain largely understudied.Therefore,this retrospective analysis of clinical data from patients who underwent laparoscopic radical colorectal cancer surgery at our center over the past 5 years sought to explore the potential variance in postoperative IH incidence following intraoperative tumor extraction.This study further aimed to evaluate the risk factors influencing IH occurrence.
MATERlALS AND METHODS
Patient characteristics
This study is a retrospective analysis of medical records from 2679 patients who underwent radical colorectal cancer surgery at our center between January 2017 and December 2022.The inclusion criteria were as follows: (1) Patients with preoperative ancillary tests indicating colorectal cancer who underwent radical colorectal cancer surgery in our hospital;(2) the surgical procedure was either laparoscopic or da Vinci robot-assisted radical tumor resection;and (3) tumor specimens were extracted by enlarging the trocar.The exclusion criteria were: (1) Patients who underwent open surgery,hand-assisted laparoscopic surgery (HALS),or Miles’ surgery,or transitioned from laparoscopic to open surgery;(2) patients who underwent natural orifice specimen extraction surgery;and (3) patients who required multiorgan resection.In total,1614 eligible patients were included in the final study.
All patients in the cohort underwent tumor excisionviatrocar enlargement and incision protector placement.The extent of the incision was determined by the size of the tumor.All patients were subjected to a 'three-step suture' procedure that involved suturing the anterior sheath of the rectus abdominis and the peritoneum,the fat layer of the abdominal wall,and the skin layer.
Follow-up method
Patient data were gathered using a hospital information system,short message service,and telephone follow-up.The preoperative,perioperative,and postoperative details of all patients included in this study were meticulously recorded.The follow-up period was delineated from the day following surgery until the final outpatient follow-up visit to evaluate the onset of IH.This follow-up primarily encompassed laboratory examinations such as routine blood tests,liver and kidney function assessments,serum electrolyte measurements,and fasting blood glucose levels.Additionally,physical examinations and imaging evaluations were conducted.The imaging examinations predominantly involved abdominal computed tomography (CT) scans and ultrasound.An IH was characterized by either a palpable defect on physical examination or an abdominal wall defect as evidenced by imaging data.The follow-up duration for IH was consistent with the postoperative follow-up period following tumor surgery,which entailed biannual check-ups for the first 2 years.The frequency of follow-ups was adjusted to every 6 months from the third year onwards.Routine abdominal CT scans were performed during the postoperative surveillance of the tumor.Patients identified through imaging as having occult IH or abdominal wall defects,but without symptoms of IH,were subjected to a 1-3-months follow-up period.This monitoring process encompassed an abdominal physical examination,color Doppler ultrasound,and,if necessary,additional abdominal CT scans.
This study examined several prognostic factors influencing incision healing,including sex,age,obesity,diabetes,anemia,hypoproteinemia,chronic cough,radiotherapy,and chemotherapy,as well as postoperative incision infection.Older patients were defined as those aged 60 years or older;obesity was characterized by a body mass index exceeding 30 kg/m2;anemia was identified by hemoglobin levels below 90 g/L;hypoproteinemia was denoted by serum albumin concentrations below 35 g/L;chronic cough encompassed both preoperative and perioperative new chronic cough;the positioning of the incision referred to the location of the enlarged trocar used for tumor specimen collection,which could be categorized into median and paramedian incisions (including supraumbilical midline,infraumbilical midline,and umbilical incisions);and the chemoradiotherapy received by patients was defined as either preoperative or postoperative.
Statistical analysis
SPSS software (version 26.0;IBM Corp.,Armonk,NY,United States) was used for statistical analyses.Categorical and quantitative variables are reported as frequencies (%) and the mean ± SD,respectively,unless otherwise stated.Categorical variables were analyzed using theχ2or Fisher exact test,whereas quantitative variables were analyzed using attest.Univariate analysis was performed to define the risk factors for extraction-site IH for all patients.Moreover,multivariate analysis was performed using logistic regression to analyze independent risk factors for postoperative IH.P< 0.05 was considered statistically significant.
RESULTS
Clinical characteristics
In this study,2679 patients who underwent radical colorectal cancer surgery at our hospital from January 2017 to December 2022 were selected.In total,1614 patients were finally included in the study.Here,303 (18.8%),923 (57.2%),171 (10.6%),and 217 (13.4%) tumors were extracted through supraumbilical midline,infraumbilical midline,umbilical,and off-midline incisions,respectively.All patients were grouped according to the incision sites through which the tumor specimens were extracted.The basic clinical information and perioperative conditions of the patients are shown in Table 1.

Table 1 Comparison of patient demographics,characteristics,and comorbidities among groups,n (%)
Comparison of IH incidence
Table 2 shows the comparative results of IH incidence.In this study,52 of the 1614 included patients developed postoperative IH,with an incidence of IH of 3.2%.The incidence of postoperative IH was significantly higher in the offmidline incision (8.8%) group than in other groups [the supraumbilical midline (2.6%),infraumbilical midline (2.2%),and umbilical incision (2.9%) groups] (χ2=24.985;P< 0.05).
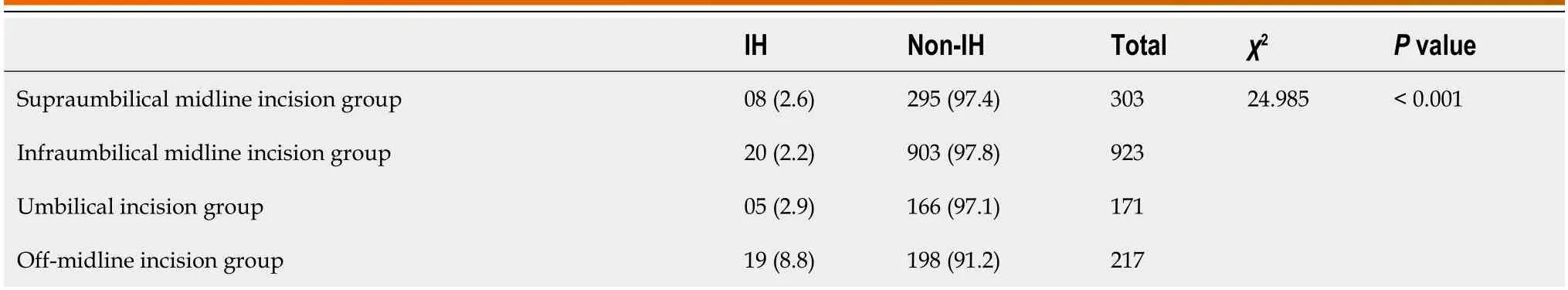
Table 2 Comparison of the rate of incisional hernia,n (%)
Univariate analysis of factors associated with IH at the extraction site
Univariate analysis was performed on the 1614 patients grouped according to IH incidence to investigate the risk factors for IH.The number of patients with obesity (17.3% in the IH groupvs4.4% in the non-IH group),comorbid diabetes (53.8% in the IH groupvs14.5% in the non-IH group),anemia (19.2% in the IH groupvs10.6% in the non-IH group),hypoproteinemia,chronic cough (75% in the IH groupvs35.5% in the non-IH group),and incision infection was significantly higher than that in the non-IH group (P< 0.05).In contrast,no significant difference in the number of patients who received radiotherapy was observed between the two groups (Table 3).
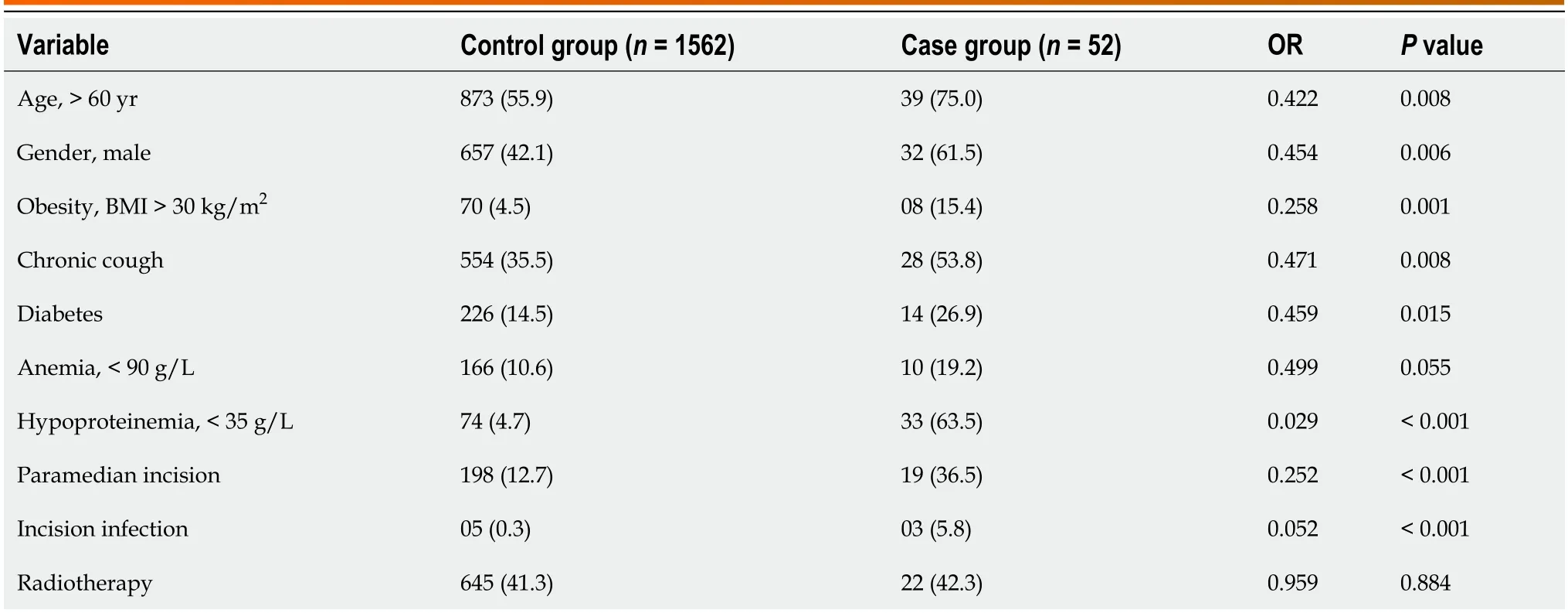
Table 3 Univariate analysis of factors associated with incisional hernia at the extraction site,n (%)
Multivariate analysis of risk factors for extraction-site IH
Further multifactorial logistic regression analysis identified off-midline incision [odds ratio (OR)=1.627],age (≥ 60 years;OR=2.231),sex (female;OR=2.273),and obesity (OR=3.299),combined chronic cough (OR=2.401),anemia (OR=6.634),and incision infection as major risk factors for extraction-site IH (P< 0.05) (Table 4).
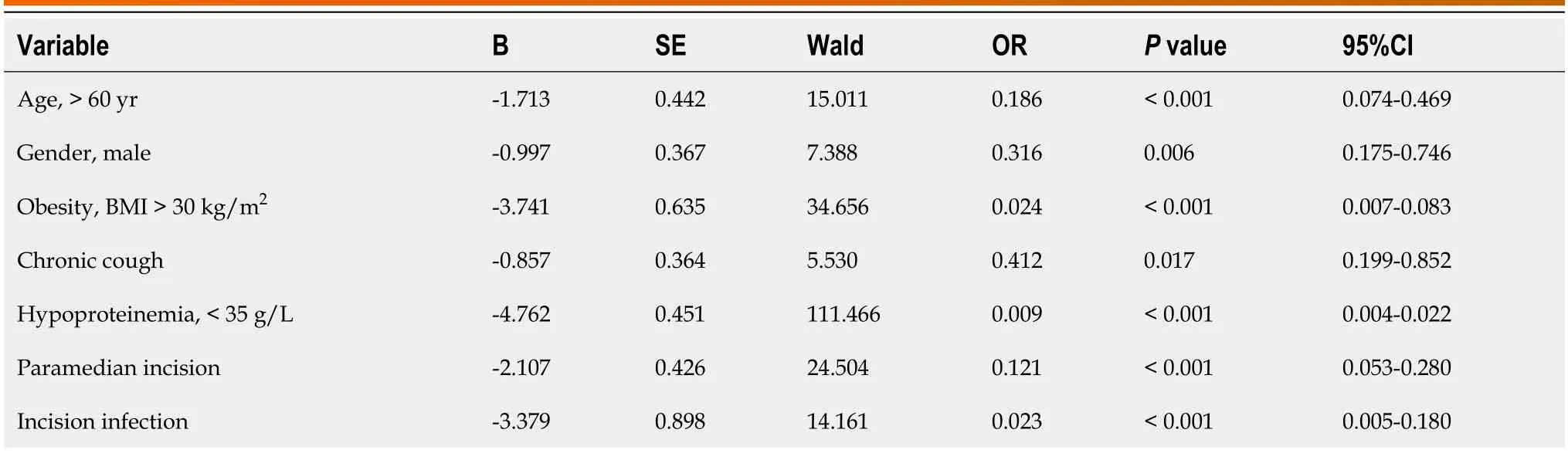
Table 4 Multivariate analysis of factors associated with risk of extraction-site incisional hernia
DlSCUSSlON
This study demonstrates that the rate of extraction-site IH varies across different abdominal wall sites,with a significantly higher incidence observed in off-midline incisions compared to median incisions (including supraumbilical midline,infraumbilical midline,and umbilical incisions).The authors posit that this is because the paramedian incision penetrates the abdominal cavityviathe rectus abdominis.This approach warrants the removal of more tissue layers than the midline incision,necessitating the severance of the rectus abdominis muscle bundle,which complicates suture placement.Excessive suture tension can induce bleeding and muscle tears upon closure of the abdominal cavity,thereby hindering wound healing and increasing the risk of IH.In addition,inadequate closure of the abdominal wall caused by insufficient tension following paramedian incision may directly contribute to high IH incidence.Furthermore,the anatomical layers of the median abdominal incision were accurately delineated.This facilitated the suture of the appropriate tissue layers without complications such as abdominal wall muscle tearing during suturing,thus promoting wound healing.A higher prevalence of anemia and hypoproteinemia was observed among patients in the sub-umbilical incision group[4].However,the incidence rate of IH was considerably lower in this group.This demonstrates the impact of incision position on the occurrence of IH.These findings contrast with those of previous studies[5-8] that tend to eschew the use of median incisions.However,this discrepancy does not negate the findings of this study.The variance in results among studies was attributed to factors such as the number of cases included and the grouping method employed.For instance,in studies examining extraction-site IH following laparoscopic surgery[9,10],the authors incorporated "conversion from laparoscopic colorectal surgery to open surgery" and “HALS” in the midline group,leading to the conclusion that IH incidence was higher after midline incisions.The authors contend that the incision size significantly exceeds that of laparoscopic surgery,whether transitioning from laparoscopic colorectal surgery to open surgery or HALS.The extended incision was identified as a risk factor for intra-operative hemorrhage,leading to an increased IH incidence in the midline group and potentially biasing the final results.
In addition to the incision location,numerous factors influence the incidence of extraction-site IH,encompassing both surgeon and patient characteristics.A multifactorial analysis identified factors such as age,obesity,sex,combined anemia,and concurrent respiratory disease as independent risk factors for IH.This finding aligns with prior research on IH following abdominal surgery[4,11,12].Patients presenting these conditions exhibit delayed wound healing and areprone to wound infection or suboptimal wound healing,thereby amplifying the risk of IH[13].Consequently,surgeons must exercise caution during suturing for patients with these predisposing conditions and closely monitor wound recovery to mitigate perioperative infections and minimize IH incidence.Operational variables,including the suturing proficiency of the surgeon and suture selection variances,can directly influence IH occurrence.Therefore,the authors posit that the incision location is not the sole determinant of extraction-site IH events.Beyond patient predispositions,it is imperative to acknowledge the significance of suture technique and material selection irrespective of incision sites[14].
In conclusion,the findings of this study tentatively indicate that the incidence of IH following laparoscopic radical colorectal cancer extraction is more likely when the tumor is removedviaoff-midline incision compared to other incisions.Therefore,it is recommended to avoid this approach,where possible.Furthermore,the significance of the suturing technique should not be overlooked.It is imperative to implement stringent perioperative management for patients at high risk of IH,including those of advanced age,obese patients,and women with diabetes,anemia,and chronic cough.This will help prevent incisional infection and poor healing,thereby reducing the occurrence of IH.
CONCLUSlON
The incidence of postoperative IH at the extraction site varies across different laparoscopic colorectal cancer surgery sites,with off-midline incision warranting avoidance whenever possible.In addition,factors such as age,sex,obesity,incision infection,and combined chronic cough and hypoproteinemia,were identified as independent risk factors for IH at the site of laparoscopic colorectal cancer surgical extraction.
ARTlCLE HlGHLlGHTS
Research background
After laparoscopic colorectal cancer surgery,there is a risk of incisional hernia (IH) at the site where the tumor specimen was removed.
Research motivation
IH that occurs after laparoscopic colorectal cancer surgery affects the recovery of patients and causes a great burden to patients.
Research objectives
This study aimed to investigate the incidence of IH at extraction sites after laparoscopic colorectal cancer surgery and the risk factors affecting the incidence of IH.
Research methods
This study presents a retrospective analysis of medical records from 1614 patients who underwent radical colorectal cancer surgery at our center between January 2017 and the present.The focus is on examining the incidence rate of IH and factors influencing IH incidence.
Research results
The incidence of postoperative IH was higher in the off-midline incision group (8.8%) than in other groups [the supraumbilical midline (2.6%),infraumbilical midline (2.2%),and umbilical incision (2.9%) groups],and the difference was statistically significant (χ2=24.985;P< 0.05).Apart from the off-midline incision,factors such as age,female gender,obesity,incision infection,combined chronic cough,and hypoproteinemia were identified as independent risk factors for IH at the site of laparoscopic colorectal cancer surgical extraction.
Research conclusions
The incidence of postoperative IH at the extraction site varies across different laparoscopic colorectal cancer surgery sites,with the off-midline incision being avoided whenever possible.Apart from the off-midline incision,factors such as age,female gender,obesity,incision infection,combined chronic cough,and hypoproteinemia were identified as independent risk factors for IH at the site of laparoscopic colorectal cancer surgical extraction
Research perspectives
According to the results of this study,an off-midline incision should be avoided at the site where the tumor specimen is removed for subsequent colorectal cancer surgery.
FOOTNOTES
Author contributions:Fan BH was responsible for investigation,writing of the original draft,formal analysis,data curation,and manuscript writing,review,and editing;Zhong KL was responsible for conceptualization,funding acquisition,methodology,project administration,and manuscript writing,review,and editing;Chen Z performed validation,formal analysis,and supervision;Zhu LJ performed supervision,formal analysis,validation,and data curation;Li F provided software,resources,and visualization;Wu WF provided software,resources,and formal analysis.
lnstitutional review board statement:This study was reviewed and approved by the Ethics Committee of Shenzhen People's Hospital.
lnformed consent statement:Patients were apprised of their rights to informed consent and provided with a signed document during postoperative follow-up.
Conflict-of-interest statement:We have no financial relationships to disclose.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Bao-Hang Fan 0009-0007-9698-5949;Ke-Li Zhong 0009-0005-9143-2961.
S-Editor:Qu XL
L-Editor:Wang TQ
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2024年3期
World Journal of Gastrointestinal Surgery2024年3期
- World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
