lmpact of frailty on short-term postoperative outcomes in patients undergoing colorectal cancer surgery: A systematic review and meta-analysis
Yao Zhou,Xiao-Lei Zhang,Hong-Xia Ni,Tian-Jing Shao,Ping Wang
Abstract BACKGROUND Colorectal cancer is a major global health challenge that predominantly affects older people.Surgical management,despite advancements,requires careful consideration of preoperative patient status for optimal outcomes.AIM To summarize existing evidence on the association of frailty with short-term postoperative outcomes in patients undergoing colorectal cancer surgery.METHODS A literature search was conducted using PubMed,EMBASE and Scopus databases for observational studies in adult patients aged ≥ 18 years undergoing planned or elective colorectal surgery for primary carcinoma and/or secondary metastasis.Only studies that conducted frailty assessment using recognized frailty assessment tools and had a comparator group,comprising nonfrail patients,were included.Pooled effect sizes were reported as weighted mean difference or relative risk (RR) with 95% confidence intervals (CIs).RESULTS A total of 24 studies were included.Compared with nonfrail patients,frailty was associated with an increased risk of mortality at 30 d (RR: 1.99,95%CI: 1.47-2.69),at 90 d (RR: 4.76,95%CI: 1.56-14.6) and at 1 year (RR: 5.73,95%CI: 2.74-12.0) of follow up.Frail patients had an increased risk of any complications (RR: 1.81,95%CI: 1.57-2.10) as well as major complications (Clavien-Dindo classification grade ≥ III) (RR: 2.87,95%CI: 1.65-4.99) compared with the control group.The risk of reoperation (RR: 1.18,95%CI: 1.07-1.31),readmission (RR: 1.70,95%CI: 1.36-2.12),need for blood transfusion (RR: 1.67,95%CI: 1.52-1.85),wound complications (RR: 1.49,95%CI: 1.11-1.99),delirium (RR: 4.60,95%CI: 2.31-9.16),risk of prolonged hospitalization (RR: 2.09,95%CI: 1.22-3.60) and discharge to a skilled nursing facility or rehabilitation center (RR: 3.19,95%CI: 2.0-5.08) was all higher in frail patients.CONCLUSION Frailty in colorectal cancer surgery patients was associated with more complications,longer hospital stays,higher reoperation risk,and increased mortality.Integrating frailty assessment appears crucial for tailored surgical management.
Key Words: Frailty;Frail adults;Colorectal surgery;Colorectal cancer;Complications;Mortality;Survival;Slinical outcomes;Meta-analysis
lNTRODUCTlON
Colorectal cancer presents a significant healthcare challenge.It currently ranks as the fourth most prevalent cancer worldwide and predominantly affects the older population[1].The management of colorectal cancer is centered on surgical procedures,with or without neoadjuvant therapy[2].A surgical approach is a challenging procedure,often involving complex resections and substantial postoperative recovery and is associated with numerous short-term complications.While advancements in surgical techniques and perioperative care have improved outcomes over the years,a growing body of evidence suggests that the preoperative status of patients plays a crucial role in determining postoperative results[3,4].Therefore,it is crucial to identify the risk factors,associated with postoperative complications in colorectal cancer patients,to enhance the care provided and to reduce potential complications.Frailty is one of the factors that has gained increasing attention in recent years.It is a complex multidimensional syndrome known to involve a range of characteristics,such as reduced muscle mass,lower levels of physical activity,cognitive challenges,and nutritional deficiencies[5-7].Frailty can affect individuals of various ages,and may potentially affect short-term postoperative outcomes in many cancers[8-10].Research on the impact of frailty on postoperative outcomes in patients undergoing colorectal cancer surgery has profound implications for the entire medical and surgical team.They should have the necessary skills to assess and recognize frailty in these patients.This recognition is crucial for tailoring preoperative preparations,which may involve optimizing nutrition,managing comorbidities,and addressing psychological concerns,all contributing to improved patient resilience.
Previous reviews have shown that frailty in patients undergoing colorectal cancer surgery is associated with higher mortality,prolonged hospital stay,serious complications,increased risk of readmission,and requirement for more support outside the home[11,12].With new studies being published on this issue,our study aims to update the existing evidence and to use a subgroup analysis to provide a more in-depth understanding of the impact of frailty on short-term postoperative outcomes,primarily,mortality and risk of complications in this cohort of patients.
MATERlALS AND METHODS
Search strategy and selection criteria
The review was performed following the PRISMA guidelines[13],and the protocol was registered with PROSPERO (registration number CRD42023461812).We conducted a thorough search on PubMed,EMBASE and Scopus to identify relevant studies published until August 31,2023.Our search strategy involved a combination of specific terms,including (Frailty OR muscle weakness OR sarcopenia OR impaired muscle function) AND (colorectal cancer surgery OR colorectal resection OR curative colorectal resection) AND (clinical outcomes OR post-operative outcomes OR mortality OR survival OR complications).
We included observational studies of prospective and retrospective cohort design,as well as case-control studies,which involved adult participants aged ≥ 18 years undergoing planned or elective colorectal surgery for primary carcinoma and/or secondary metastasis.Only studies that performed frailty assessments using established frailty assessment tools and defined and categorized frailty based on recognized criteria were included.The comparator group of the included studies should have consisted of nonfrail participants undergoing elective colorectal surgery for malignancy.Studies with either laparoscopic/robotic (minimally invasive) or open surgical approaches were eligible for inclusion.Additionally,the included studies should have reported at least one short-term postoperative outcome of interest and provided sufficient data for effect size calculation.There were no restrictions on the publication date.
Case reports,case series,reviews,conference abstracts,editorials,studies involving pediatric populations (participants aged < 18 years),or patients undergoing emergency colorectal surgery were excluded.Additionally,studies with patients undergoing colorectal surgery for non-carcinomatous indications were excluded.To prevent duplication,in cases where multiple publications originated from the same study,only the most comprehensive and recent publication was considered.
Process of article selection and quality assessment
After the initial search across the databases and the removal of duplicates,two researchers from our team conducted a meticulous review of the remaining studies.During the initial screening phase,titles and abstracts were searched.Full texts of the studies that met the predefined criteria were,subsequently,examined for eligibility.Any disagreements were resolved through discussion between the two authors.If necessary,we sought the perspective of a third author to reach a consensus.
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of the studies[14].Data extraction was conducted systematically by two independent reviewers using a standardized data extraction spreadsheet and included study identifiers such as author's name,publication year,study location,subject characteristics,sample size,the definition of frailty used,and the outcomes of interest.Any discrepancies during the data extraction process were resolved by discussion or by consulting a third senior reviewer.
Statistical analysis
All the analysis was done using STATA version 15.0.We reported the effect size as the relative risk (RR) for categorical outcomes and as the weighted mean difference (WMD) for continuous outcomes.Effect sizes were reported along with 95% confidence intervals (CIs).A random-effects model was used for all our analyses to account for variations in baseline characteristics among the included studies.Publication bias was assessed using both Egger’s test and visual inspection of the funnel plot[15].We conducted subgroup analysis based on study design (retrospective and prospective cohort),type of surgery (minimally invasive and open),and tumor stage.P< 0.05 indicated statistical significance.
RESULTS
Selection of studies for inclusion
Our search strategy initially identified 297 studies.After eliminating 83 duplicates,214 unique studies remained.After the review of titles and abstracts,181 studies were excluded.A thorough review of the complete texts of the remaining 33 studies was done,and eventually,24 studies were eligible for inclusion in our meta-analysis[16-39] (Figure 1).
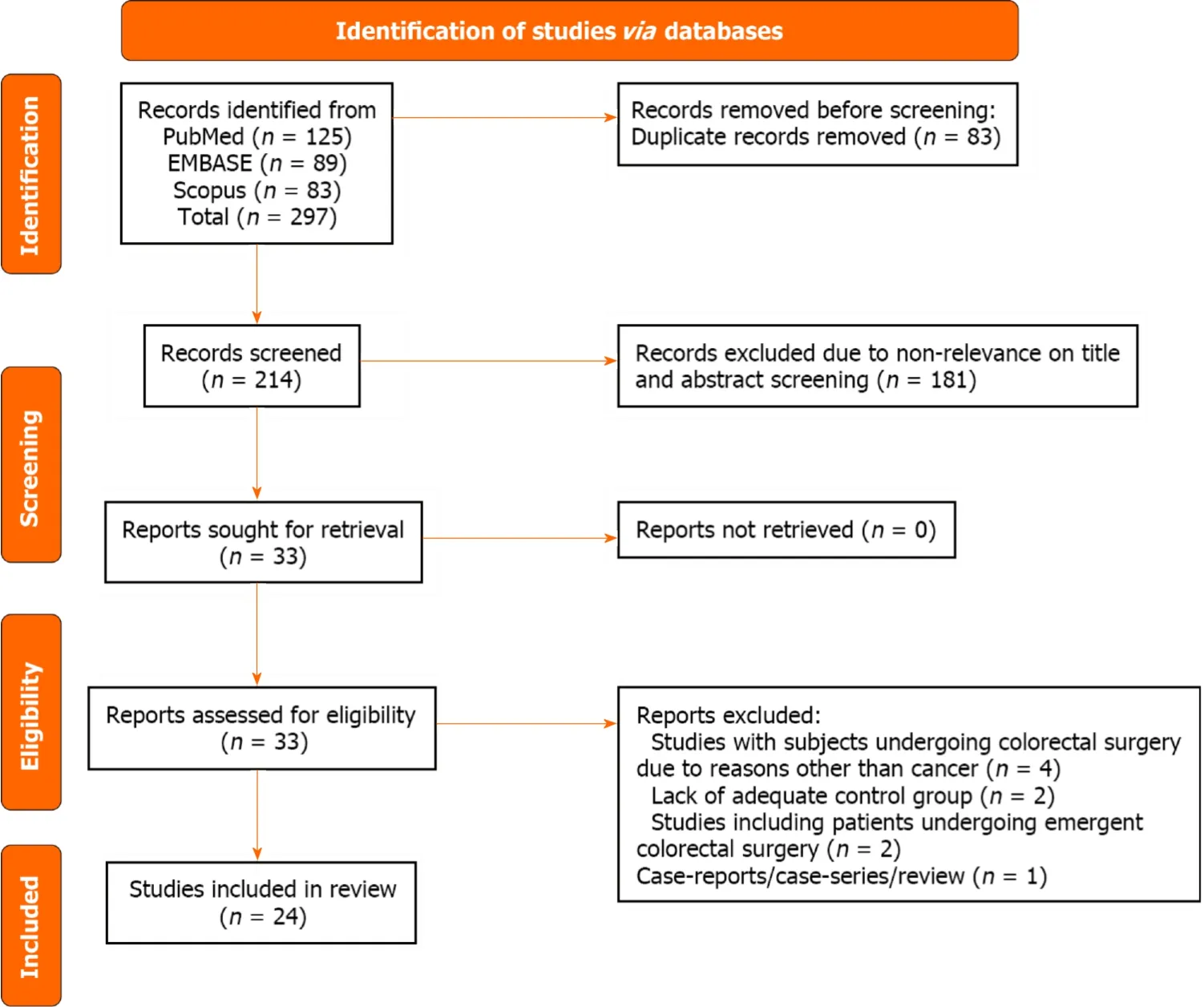
Figure 1 Selection process of studies included in the review.
Characteristics of the included studies
Of 24 studies,14 were retrospective cohort studies and the remaining 10 studies had a prospective design.The majority of the studies were conducted in the United States (n=5),Japan (n=4) and Netherlands (n=4).Two studies each were conducted in Norway and Spain.One study each was conducted in the United Kingdom,China,Italy,New Zealand,Mexico and Finland.One study was multicentric (Singapore and Japan).The assessment criteria for frailty varied significantly among the studies.Even when studies used the same assessment tool,the cutoff values of frailty differed.Modified Frailty Index (n=5) and the Clinical Frailty Scale (n=5) were the most used assessment criteria.The studies included a total of 277993 patients (77091 with frailty and 200902 without).The mean quality assessment score of the included studies was 7.3,indicating that the studies were of acceptable quality.There were eleven studies with an NOS score of 7 (out of the maximum attainable score of 9),eight studies with a score of 8,four studies with a score of 6,and one study scoring 9 (Table 1).
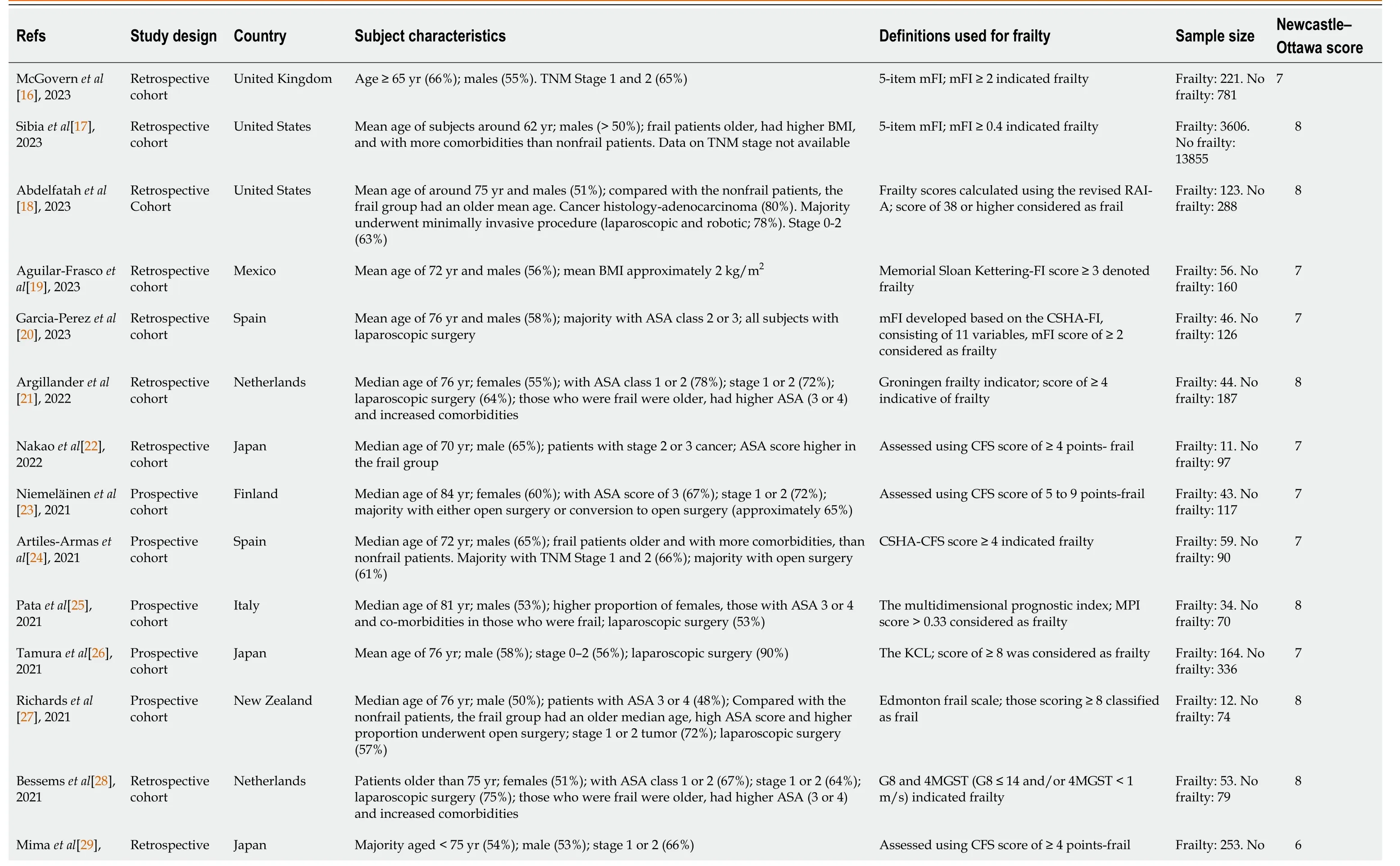
Table 1 Characteristics of the included studies
Risk of mortality
Compared with nonfrail patients,patients with frailty had increased risk of mortality at 30 d (RR: 1.99,95%CI: 1.47-2.69;n=11,I2=49.2%),at 90 d (RR: 4.76,95%CI: 1.56-14.6;n=5,I2=82.6%) and at 1 year (RR: 5.73,95%CI: 2.74-12.0;n=6,I2=80.5%) of follow-up (Figure 2).The observed pooled effect size of the risk of mortality at 6 mo of follow-up was not significant (RR: 3.05,95%CI: 0.42-21.9;n=2,I2=79.2%),possibly due to a limited number of studies (n=2) reporting on the mortality outcome at this time point.We did not find the presence of publication bias either on Egger’s test or on the visual inspection of the funnel plot.Egger’sPvalue for mortality at 30-d,90-d and 1-year of follow-up was 0.19,0.44 and 0.83 respectively.The funnel plots for mortality outcomes at different time points of follow-up have been presented inSupplementary Figures 1-3.

Figure 2 Risk of mortality among frail patients undergoing colorectal cancer surgery,compared with nonfrail patients. RR: Relative risk;CI: Confidence interval.
Subgroup analysis based on the study design showed that the risk of mortality for frail patients was higher and statistically significant in both retrospective and prospective cohort studies (Table 2).Similarly,there was an increased risk of mortality in frail patients irrespective of the mode of surgical management;that is,open surgery or minimally invasive surgery.Subgroup analysis of patients with stage 0 to 2 tumor showed that frailty was associated with the increased risk of mortality at 30 d,90 d and 12 months of follow-up (Table 2).
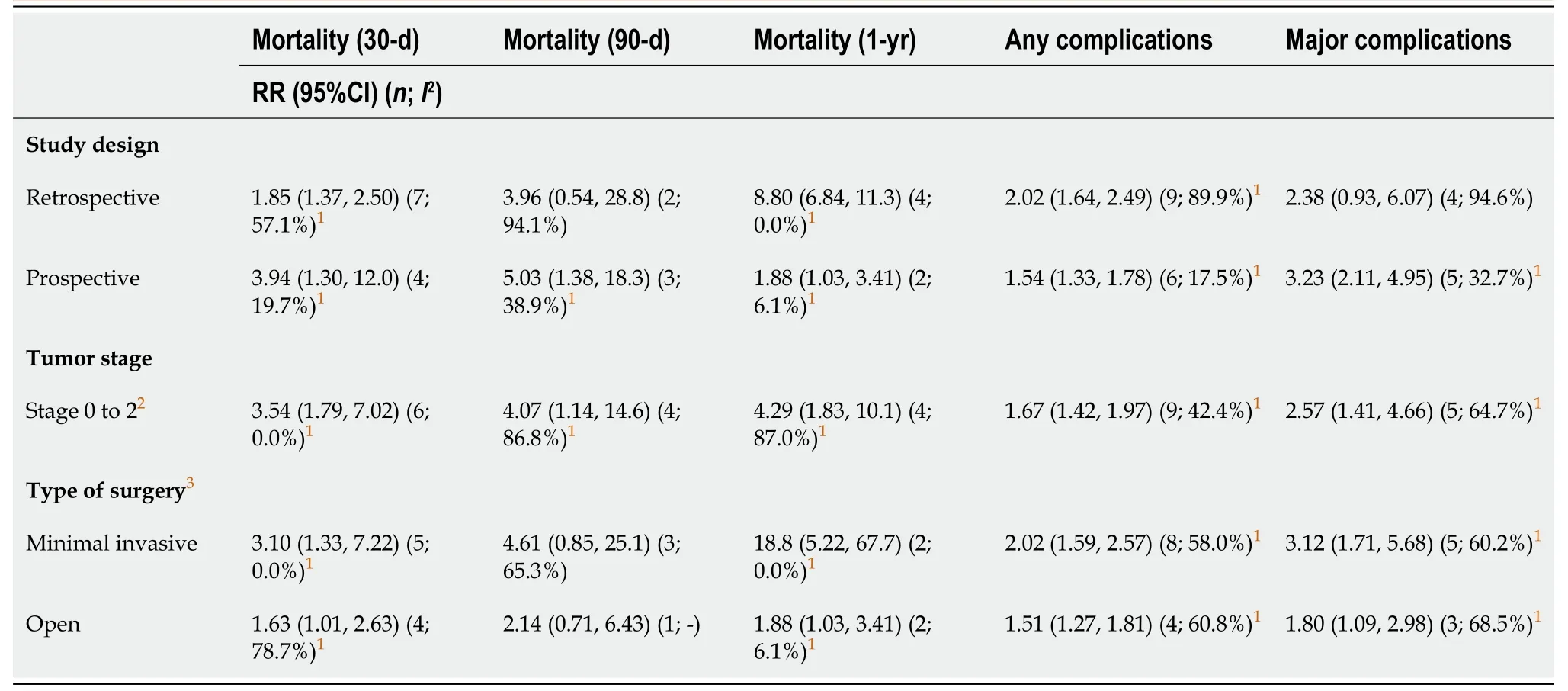
Table 2 Findings of the subgroup analysis
Risk of complications
Frail patients had an increased risk of any complications (RR: 1.81,95%CI: 1.57-2.10;n=15,I2=83.8%) as well as majorcomplications (Clavien-Dindo classification grade ≥ III) (RR: 2.87,95%CI: 1.65-4.99;n=9,I2=90.4%) (Figure 3).There was evidence for the presence of significant publication bias for any complications (P=0.02) or major complications (P=0.04) on Egger’s test.The funnel plots for both these outcomes are presented in Supplementary Figures 4 and 5.In the subgroup analysis,the increased risk of complications was observed among frail patients,irrespective of the study design (retrospective and prospective cohort) and mode of surgical management (open or minimally invasive surgery) (Table 2).
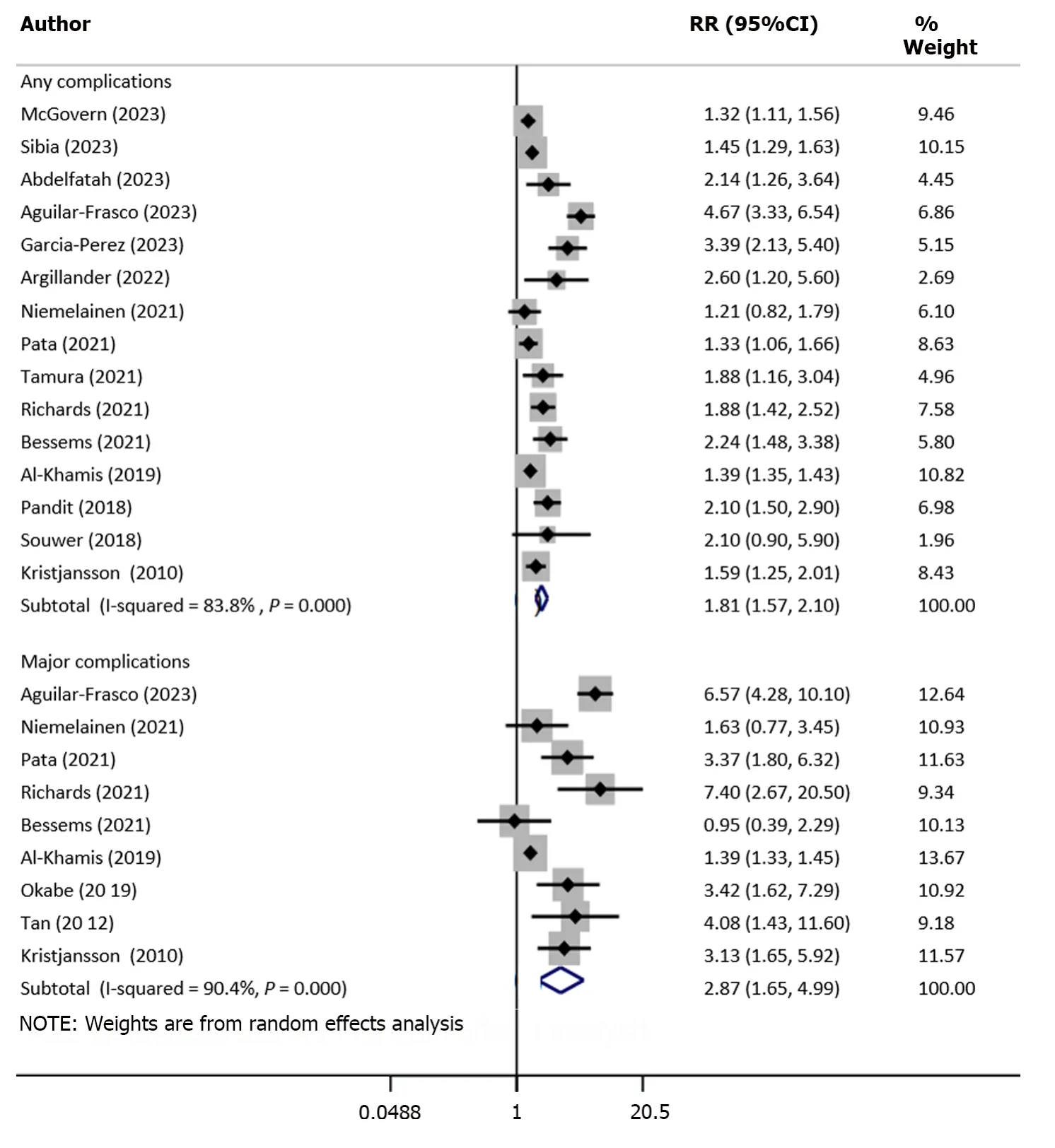
Figure 3 Risk of any and major complications among frail patients undergoing colorectal cancer surgery,compared with nonfrail patients. RR: Relative risk;CI: Confidence intervals.
Upon pooling of studies with patients with stage 0 to 2 tumor,we showed that frailty was associated with the increased risk of complications (Table 2).
More specifically,the risk of reoperation (RR: 1.18,95%CI: 1.07-1.31;n=4,I2=12.8%),readmission (RR: 1.70,95%CI: 1.36-2.12;n=8,I2=65.6%) and need for blood transfusion (RR: 1.67,95%CI: 1.52-1.85;n=4,I2=0.0%) was higher in frail compared with nonfrail patients (Figure 4).Similarly,the risk of wound complications (RR: 1.49,95%CI: 1.11-1.99;n=5,I2=39.1%),delirium (RR: 4.60,95%CI: 2.31-9.16;n=5,I2=0.0%) and discharge to skilled nursing facility or rehabilitation Centre (RR: 3.19,95%CI: 2.0-5.08;n=5,I2=78.2%) were all higher in frail patients (Figure 5).
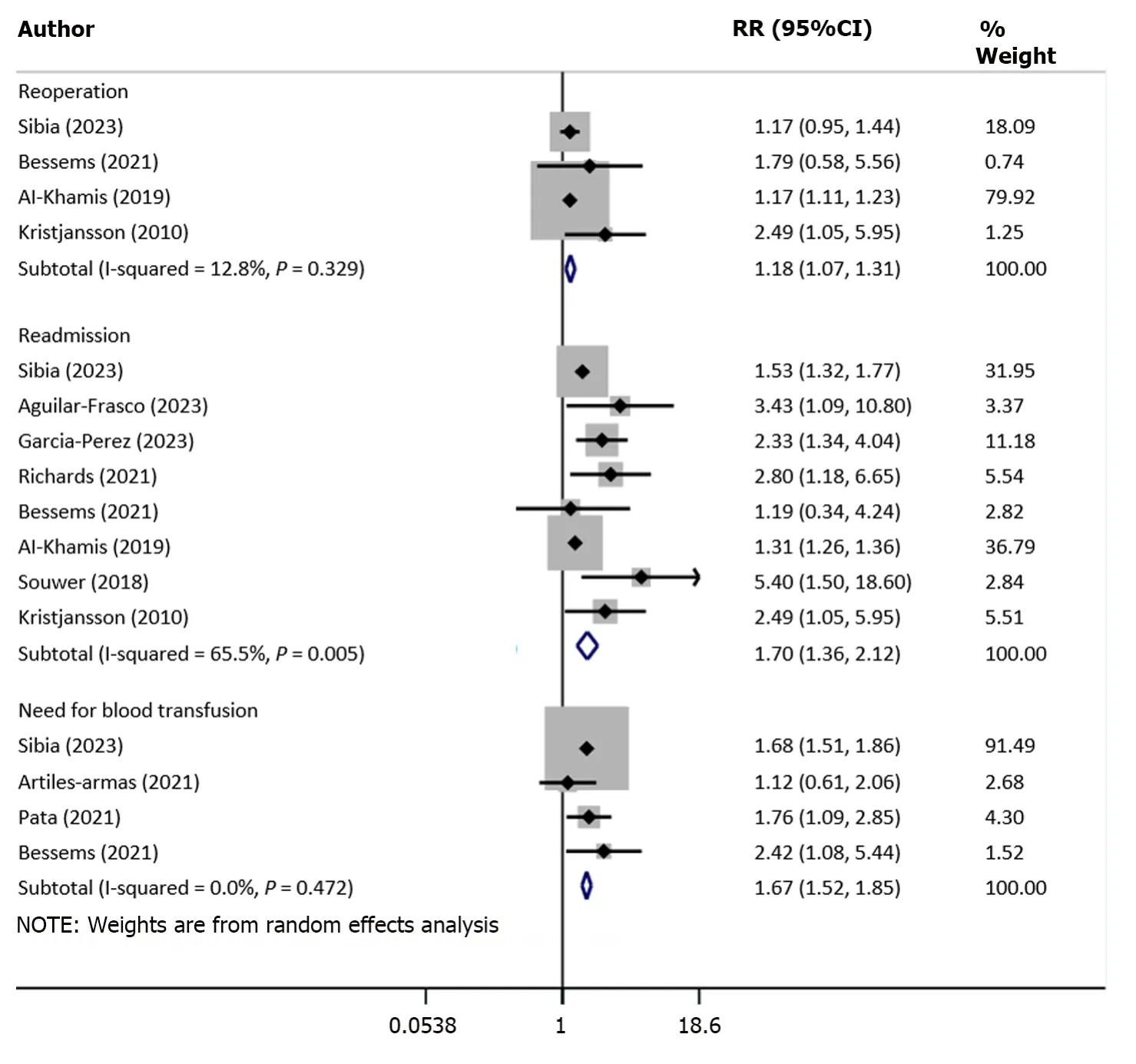
Figure 4 Risk of reoperation,readmission and need for blood transfusion among frail patients undergoing colorectal cancer surgery,compared with nonfrail patients. RR: Relative risk;CI: Confidence interval.

Figure 5 Risk of wound complication,delirium,prolonged hospital stay and discharge to skilled nursing facility among frail patients undergoing colorectal cancer surgery,compared with nonfrail patients. RR: Relative risk;CI: Confidence intervals.
Length of hospital stay
There was a significant increase in the length of hospital stay (in days) in frail patients,compared with normal/nonfrail patients (WMD: 3.80,95%CI: 3.05-4.56;n=11,I2=99.5%) (Figure 6).The risk of prolonged hospitalization (RR: 2.09,95%CI: 1.22-3.60;n=4,I2=88.0%) was also higher in frail patients (Figure 5).
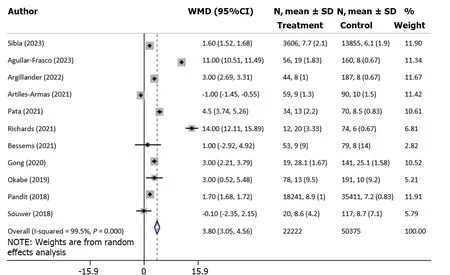
Figure 6 Duration of hospital stay (in days) among frail patients,compared with nonfrail patients,undergoing colorectal cancer surgery. WMD: Weighted mean difference;CI: Confidence interval.
DlSCUSSlON
Our meta-analysis showed a significant association between preoperative frailty and increased risk of mortality and complications,including reoperation,readmission,need for blood transfusion,wound complications,delirium,and risk of prolonged hospitalization.The increased mortality risks,identified at multiple time points,at 30 d,90 d,and 1 year of follow-up,further emphasize the enduring impact of frailty on survival prospects.Frail patients frequently face challenges related to their weakened cardiovascular,respiratory and immune systems,making them less resilient when it comes to the physical demands of surgery and its subsequent recovery[40-42].This fragility may result in a heightened risk of postoperative complications,ultimately contributing to elevated mortality rates.
The association between frailty and an increased incidence of postoperative complications is equally noteworthy.Frail patients in our study faced a nearly twofold higher risk of encountering any complication and the risk of major complications was nearly threefold higher.Colorectal cancer surgery is a complex and invasive procedure that can place significant physical and physiological stress on patients.Our results show that frailty is associated with a higher incidence of surgical complications such as wound infections.Our conclusions agree with previous studies that showed that the weakened physiological state of frail patients can impair the healing process,making them more susceptible to these surgical challenges[43,44].Frailty may disrupt the stress response,potentially leading to imbalanced inflammation,delayed wound healing,and impaired tissue recovery[45,46].These interconnected processes set off a chain of events that can increase the susceptibility of frail patients to various complications.Additionally,a compromised immune system of these patients makes them vulnerable to infections frequently associated with surgical procedures[47].
We also found an increased risk of prolonged hospital stay in frail patients that could also be attributed to the increased risk of complications that may eventually require longer hospitalization.In addition to the impact on the patient,extended hospitalization also strains the healthcare system.This strengthens the importance of more robust support systems to address the multifaceted needs of frail patients during their hospitalization.
Our findings strongly advocate the inclusion of a frailty assessment in the preoperative evaluation of candidates for colorectal cancer surgery.Early identification of frail patients can enable the implementation of personalized interventions to optimize their perioperative care,reduce potential complications,and enhance overall outcomes[48,49].This suggestion emanates from a recent systematic review by Guoet al[48] that included nine studies with 1313 cancer patients.The review found that prehabilitation for frailty reduced the risk of complications and the average length of hospital stay.However,the intervention did not have a significant impact on 30-d and 3-month mortality and readmission rates.These findings emphasize the importance of collaborative efforts involving surgical teams,geriatric specialists,and other relevant healthcare providers to ensure the comprehensive management of frail patients.
The findings of our review have implications for the healthcare team.It emphasizes the importance of a collaborative effort to minimize stressors,carefully monitor vital signs,and customize anesthetic and fluid management.Effective communication among healthcare professionals is paramount in ensuring that everyone is aware of the patient’s frailty status and potential risks.In the postoperative phase,nurses could play a critical role in monitoring patients for complications,such as infections or delirium,and advocating for appropriate pain management strategies.Additionally,they could actively participate in designing rehabilitation plans,offering patient and family education,and contributing to quality improvement efforts.Emotionally supporting frail patients and facilitating access to psychological services is one of the important aspects of the comprehensive care that nursing personnel can provide.
The finding that frailty correlates with adverse outcomes necessitates a thoughtful integration of this information into the crucial preoperative consent and decision-making process between patients and surgeons.During the informed consent discussions,surgeons should meticulously elaborate on the implications of frailty,elucidating the heightened risks associated with postoperative complications and prolonged recovery times.This discourse should not only encompass a comprehensive assessment of the individual’s frailty level but also foster shared decision-making,allowing patients to actively engage in treatment choices based on their values and preferences.Importantly,setting realistic expectations becomes paramount,creating awareness among patients about the challenges posed by frailty and the potential limitations of surgery.Additionally,preoperative interventions,like physical therapy and nutritional support,can be used to enhance patients’ resilience.The documentation of these discussions in medical records could ensure transparency,will aid continuity of care,and reinforce a patient-centric approach to managing colorectal cancer surgery in frail individuals.
There are several frailty assessment tools to choose from to evaluate and quantify frailty in older individuals.The best tool choice will depend on various factors,including the context of use,the population being assessed,and the specific goals of the assessment.The choice of the best frailty assessment tool will also depend on the specific needs of the healthcare setting,available resources,and the expertise of the assessors.Considering the reliability,validity and feasibility of a tool in the given context is important.Additionally,combining multiple tools or approaches may provide a more comprehensive understanding of frailty in older individuals.
We acknowledge several limitations in this meta-analysis.Firstly,the studies included displayed some heterogeneity in terms of patient populations,surgical techniques,and outcome definitions.This diversity may have introduced variations in the results for certain outcomes.Additionally,the variability in the methods used for assessing frailty across the studies could have led to inconsistent categorization of frailty,potentially affecting the strength of the observed associations.Moreover,the included studies were retrospective and may have involved selection bias when considering frail patients.This may have affected the internal validity of the results.The presence of unmeasured confounding variables,such as differences in comorbidities or socioeconomic factors,might have influenced the observed outcomes.
CONCLUSlON
This meta-analysis emphasizes the crucial role of frailty as a predictive factor for adverse postoperative outcomes in colorectal cancer surgery.The identified associations between frailty and elevated risks of mortality,complications and other adverse events highlight the urgency of implementing comprehensive strategies tailored to the specific requirements of frail individuals.The integration of frailty assessment into routine clinical practice has the potential to not only enhance patient care but also guide treatment decisions,ultimately improving surgical outcomes for this vulnerable patient population.
ARTlCLE HlGHLlGHTS
Research background
Colorectal cancer presents a significant healthcare challenge.The management is centered on surgical procedures,with or without neoadjuvant therapy.While advancements in surgical techniques have improved outcomes,recent evidence highlights the critical role of preoperative frailty in influencing postoperative results.Our review aimed to update existing evidence on the impact of preoperative frailty on survival and other key clinical outcomes in subjects with colorectal cancer undergoing elective surgery.
Research motivation
To update existing evidence,through inclusion of contemporary studies,in order to guide clinical practice.
Research objectives
To identify and include all relevant studies to analyze and document the association of frailty with short-term postoperative outcomes in patients undergoing colorectal cancer surgery.
Research methods
A comprehensive literature search was conducted using PubMed,EMBASE and Scopus to identify observational studies involving adults (age ≥ 18 years) undergoing planned colorectal surgery for primary carcinoma and/or secondary metastasis.Included studies utilized recognized frailty assessment tools and featured a comparator group of nonfrail patients.Pooled effect sizes,along with 95% confidence intervals,were reported.
Research results
A total of 24 studies were included.Frailty was found to be associated with increased risk of mortality at 30 d,90 d and 1 year of follow-up.Frail patients had increased risk of overall complications as well as major complications,compared with the nonfrail patients.The risk of need for reoperation,readmission,need for blood transfusion,wound complications,delirium,risk of prolonged hospitalization and discharge to skilled nursing facility or rehabilitation center was higher in frail patients.
Research conclusions
In patients undergoing colorectal cancer surgery,frailty was associated with a significant increase in perioperative complications,longer hospital stay,higher risk of reoperation and increased mortality rate.
Research perspectives
This finding of this meta-analysis emphasizes the crucial role of frailty as a predictive factor for adverse postoperative outcomes in colorectal cancer surgery.They further call for integration of frailty assessment into routine clinical practice to enhance patient care and guide treatment decisions.
FOOTNOTES
Co-first authors:Yao Zhou and Xiao-Lei Zhang.
Co-corresponding authors:Tian-Jing Shao and Ping Wang.
Author contributions:Zhou Y and Zhang XL designed the research;Ni HX,and Shao TJ performed the research;Wang P,Zhou Y and Ni HX analysed the data;Shao TJ and Wang P wrote the paper.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
PRlSMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist,and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Tian-Jing Shao 0009-0005-3953-2519;Ping Wang 0009-0006-0447-0044.
S-Editor:Fan JR
L-Editor:Kerr C
P-Editor:Cai YX
 World Journal of Gastrointestinal Surgery2024年3期
World Journal of Gastrointestinal Surgery2024年3期
- World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
